A Rare Case of Acute Cerebral Embolism from Left Atrial Myxoma Complicated by Postoperative Atrial Fibrillation
Article Information
Yaser Khalid1*, Neethi Dasu1, Kirti Dasu2, Maziyar Daneshvar1, Vivek Sailam3
1Rowan School of Medicine, Jefferson Health System, Stratford, NJ, USA
2Department of Biology, Syracuse University, Syracuse, NY, USA
3Department of Interventional Cardiology, Virtua Lourdes, Camden, NJ, USA
*Corresponding Author: Yaser Khalid, Rowan School of Medicine, Jefferson Health System, One Medical Center Dr, UDP Suite 2300, Stratford, NJ, USA, 08084
Received: 13 May 2020; Accepted: 22 May 2020; Published: 12 June 2020
Citation: Yaser Khalid, Neethi Dasu, Kirti Dasu, Maziyar Daneshvar, Vivek Sailam. A Rare Case of Acute Cerebral Embolism from Left Atrial Myxoma Complicated by Postoperative Atrial Fibrillation. Cardiology and Cardiovascular Medicine 4 (2020): 230-238.
View / Download Pdf Share at FacebookAbstract
Primary cardiac tumors are those that originate in the heart and are extremely rare. Myxomas are the most common form of primary cardiac tumors. They have a variety of presentations, such as constitutional symptoms, cardioembolic events like cerebrovascular accidents (CVA), or hemodynamic abnormalities. Paroxysmal atrial fibrillation (PAF) is a well-known postoperative complication of coronary artery bypass grafting (CABG), but there are extremely few cases of PAF occurring post-operatively after left atrial myxoma surgical resection. We present a case of a 69- year-old female with a history of subarachnoid hemorrhage (SAH) who was diagnosed with CVA secondary to thromboembolism from left atrial myxoma. She then developed atrial fibrillation which required cardioversion. This case presents a challenge in terms of keeping left atrial myxoma as part of the differential diagnosis for cardioembolic CVA; deciding optimal timing for surgical resection; and finally, how to manage the subsequent new-onset atrial fibrillation.
Keywords
Acute Cerebral Embolism; Atrial Fibrillation
Article Details
Introduction
Cardiac myxomas are the most common primary tumors of the heart. They are most often located in the left atrium. The majority of patients with left atrial myxomas are asymptomatic, but they can present classically as a triad of obstruction, constitutional symptoms, and/or embolic events. Transthoracic echocardiography (TTE) is the initial imaging of choice for cardiac myxomas, but they can be better visualized on transesophageal echocardiography (TEE) and cardiac magnetic resonance imaging (CMR). Surgical excision is the only definitive treatment. We report a case of a large left atrial myxoma discovered following a new cerebrovascular accident from systemic embolization.
Case report
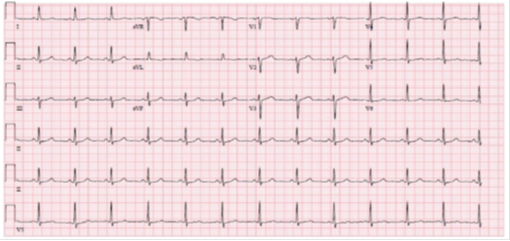
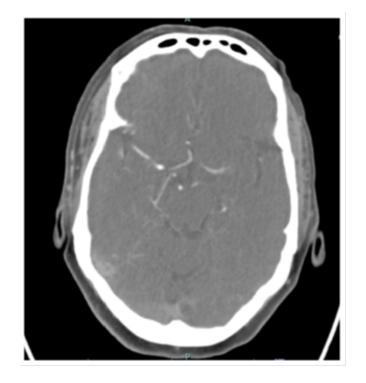
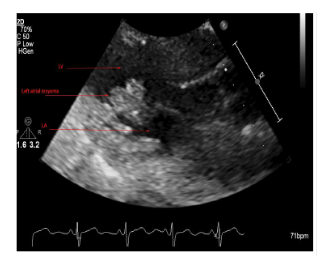
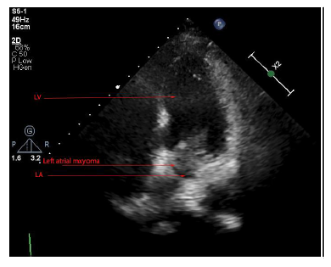
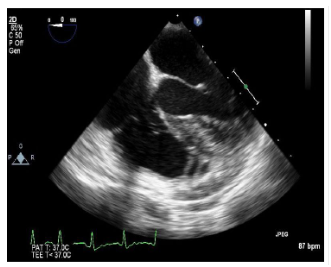
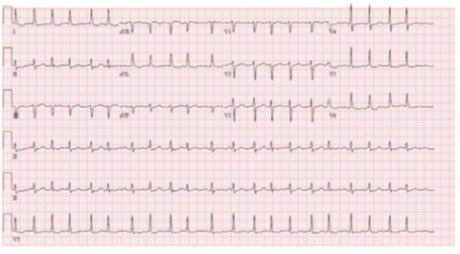
A 69-year-old female with a past medical history of hypertension, previous subarachnoid hemorrhage (SAH) secondary to an anterior communicating artery (ACOM) aneurysm that required clipping and hyperlipidemia who presented for confusion, dysphagia and word finding difficulties. Computed tomography (CT) of the head was unremarkable. The patient’s symptoms persisted for one hour before returning to baseline. Electrocardiogram (ECG) showed normal sinus rhythm with no underlying arrhythmias or left atrial enlargement (Figure 1). Thus, due to having a high clinical suspicion of a cerebrovascular event (CVA), a CTA was performed which revealed acute occlusion of the left internal carotid artery leading to left middle cerebral artery occlusion (Figures 2-3). This territory of her brain was previously affected by a SAH for which she was still being treated with aspirin and clopidogrel, thus she was not a tissue plasminogen activator (tPA) candidate. During the patient's diagnostic work-up for her acute CVA, a TTE revealed a highly mobile 1.6cm x 2.7cm echodensity which was attached to the left interatrial septum (Figures 4 and 5) and protruded through the mitral valve (Video 1, Video 2, Video 3). There was high suspicion that the mass was a left atrial myxoma based on the TTE features, thus, the patient was transferred to our facility for cardiothoracic care.
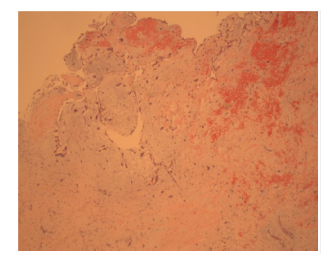
The patient underwent a minimally invasive excision of the cardiac mass, repair of the septal defect with patch closure, and cryoablation of the left atrium with no complications. Gross dissection of the mass showed a 1.2cm x 1.1cm x 0.3 cm pedunculated mass with a 1.5cm stalk. Pathology of the left atrial mass revealed cardiac muscle with variable degenerative changes, areas of necrosis, and clusters of hemosiderin laden macrophages. These findings were consistent with a left atrial myxoma on hematoxylin and eosin staining (Figure 6). Postoperative TTE (Figure 7) showed complete resection of the left atrial myxoma (Video 4, Video 5, Video 6).
On postoperative day three, the patient developed atrial fibrillation with rapid ventricular response. She was treated with intravenous amiodarone with successful chemical cardioversion to normal sinus rhythm. She was maintained on both oral amiodarone for rhythm control as well as metoprolol for rate control. Then, she was monitored for five days on the telemetry floors and subsequently discharged to a subacute rehabilitation facility. At the time of discharge, the patient was deemed too high risk for anticoagulation given her history of intracranial bleeding despite a CHADSVASC score of 4, so no anticoagulation was begun.
Finally, the patient was seen for post-operative follow-up in the office where she was found to have recurrent atrial fibrillation with rapid ventricular rate (RVR) (Figure 8). On readmission, the patient was started on an intravenous cardizem and digoxin for rate control. After weighing the benefits and risks, anticoagulation was now recommended by the neurology team. A TEE did not reveal left atrial thrombus and was followed by successful synchronized cardioversion. Upon discharge, she maintained normal sinus rhythm. She continued apixaban for anticoagulation and amiodarone for rhythm control.
Discussion:
Cardiac tumors are categorized into primary cardiac tumors, which have an incidence rate of 0.001% to 0.28%, and secondary tumors which represent the metastatic invasion of cardiac tissue and are estimated to be one hundred times more common than primary tumors [1,2]. The majority of primary cardiac tumors are benign, of which 50% are myxomas originating in the left atrium [3].
Atrial myxomas are most commonly found in women from the ages of thirty to sixty years old [4]. Myxomas are generally sporadic, although there is a familial component which accounts for approximately 7% of the cases [4]. Around 90% of these tumors are solitary lesions that are smooth, villous or pedunculated in appearance. They generally present with symptoms when larger than seventy grams, because this size causes intracardiac obstruction [5–7]. A tumor thrombus causing CVA is an extremely uncommon manifestation but should be considered as part of the differential diagnosis in patients who present with neurologic symptoms, given the potential for catastrophic sequelae.
Echocardiography remains the initial preferred diagnostic imaging tool and can identify the location, shape, size and the attachment site of the tumor [8]. TEE is the preferred non-invasive modality to analyze the location of stalk attachment and size of atrial myxomas, especially those that are smaller [8]. Other imaging options include CT, which can demonstrate a well-defined spherical or ovoid intracavitary mass, and cardiac magnetic resonance imaging (CMR) with gadolinium can be helpful in visualizing the point of attachment [9].
Our patient initially presented with neurological symptoms, confusion and dysphagia, which were determined to be due to an acute cardioembolic CVA due to the left atrial myxoma as she had no previous cardiac history. Initial ECGs showed normal sinus rhythm and arrhythmias were not observed on telemetry, thus atrial tachyarrhythmias, such as atrial fibrillation, were ruled out as a cause of the CVA. Complications from atrial myxomas include systemic and cardiac embolism and are associated with a high mortality rate [8,10]. It is likely that the tumor thrombus embolized and caused the patient’s CVA. Nonetheless, it is extremely rare for patients presenting only with neurological symptoms to have an underlying left atrial myxoma as the etiology. Thus, it was important in this case that further workup, such as echocardiography, was obtained after the patient’s initial CT imaging was negative, as neurologic manifestations can be devastating. Myxomas greater than 25 mm have a higher rate of embolic events, as observed with our patient who had a 16mm x 27mm sized tumor [11].
Surgical excision is the definitive treatment for left atrial myxomas, but for patients with contraindications to surgery, conservative management with systemic anticoagulation and surveillance TTE is an option [12]. In this case, due to the patient’s history of SAH, anticoagulation and thrombolytics were contraindicated. Fortunately, the patient’s symptoms resolved. The surgical approach is decided based on the size of the mass and the type of attachment. Most commonly, a bi-atrial approach allows for correct resection margin by confirming the tumor pedicle under visualization and reduces the risk of post-surgical complications [12,13].
The most common postoperative complications for surgical excision of left atrial myxomas are pneumonia and coronary sinus rupture [4]. Atrial fibrillation is an extremely uncommon complication. ECG findings for atrial fibrillation in patients with left atrial myxomas can show an increase in P-wave amplitude, duration and dispersion [14]. These findings on ECG are seen because left atrial myxomas increase the left atrial chamber size and obstruct the left ventricular outflow tract, which then increases the left atrial pressure, and this is manifested on ECG as an increased P-wave amplitude [15,16]. Previous studies have demonstrated that left atrial enlargement correlates with increased tumor size and subsequently it is one of the main predictors for the development of postoperative atrial fibrillation [15]. Interestingly, our patient’s preoperative echocardiogram and ECG revealed no evidence of left atrial enlargement or unusual P-wave morphology demonstrating a unique and under-reported presentation of a crdiac myxoma. Clinicians must be vigilant in monitoring for post-operative arrhythmias in for these patients because studies show that there is a significant decrease in 10-year survival rate, increased risk of the development of multiple post-operative complications, and longer intensive care unit stays for patients with the development of post-operative atrial fibrillation following left atrial myxoma excision [17].
References:
- Kumar AS, Jayalakshmi TS, Kale SC, et al. Management of massive air embolism during open heart surgery. International Journal of Cardiology 9 (1985): 413-416.
- Yu K, Liu Y, Wang H, et al. Epidemiological and pathological characteristics of cardiac tumors: a clinical study of 242 cases. Interactive Cardiovascular and Thoracic Surgery 6 (2007): 636-639.
- Reynen K. Cardiac myxomas. New England Journal of Medicine 333 (1995): 1610-1617.
- Lee KS, Kim GS, Jung Y, et al. Surgical resection of cardiac myxoma—a 30-year single institutional experience. Journal of Cardiothoracic Surgery 12 (2017): 18.
- Mihaela O, Anca M, Dinesch M, et al. Atrial Fibrillation, the First Manifestation of Atrial Myxoma.
- Latifi AN, Ibe U, Gnanaraj J. A case report of atrial myxoma presenting with systemic embolization and myocardial infarction. European Heart Journal-Case Reports 3 (2019): ytz104.
- Fontes-Oliveira M, Rodrigues P, Silveira I, et al. Cardiac Mass: Left Atrial Myxoma. Journal of Cardiovascular Imaging 28 (2020): 63-66.
- Kalçik M, Bayam E, Güner A, et al. Evaluation of the potential predictors of embolism in patients with left atrial myxoma. Echocardiography 36 (2019): 837-843.
- Biswas A, Thakur AK. An unusual presentation of atrial myxoma in an elderly patient: a case report. Cases Journal 1 (2008): 384.
- Zheng Z, Guo G, Xu L, et al. Left atrial myxoma with versus without cerebral embolism: length of symptoms, morphologic characteristics, and outcomes. Texas Heart Institute Journal 41 (2014): 592-595.
- He DK, Zhang YF, Liang Y, et al. Risk factors for embolism in cardiac myxoma: a retrospective analysis. Medical science monitor: International Medical Journal of Experimental and Clinical Research 21 (2015): 1146.
- Ullah W, McGovern R. Natural history of an atrial myxoma. Age and ageing 34 (2005): 186-188.
- Sellke FW, Lemmer Jr JH, Vandenberg BF, et al. Surgical treatment of cardiac myxomas: longterm results. The Annals of Thoracic Surgery 50 (1990): 557-561.
- McCarron EP, Clinton A, Herron B, et al. Atrial flutter with underlying left atrial myxoma. The American Journal of Medicine (2019).
- Sahin M, Dundar C, Alici G, et al. Postoperative atrial fibrillation in patients with left atrial myxoma. Cardiovascular Journal of Africa 26 (2015): 120.
- Wang H, Li Q, Xue M, et al. Cardiac myxoma: a rare case series of 3 patients and a literature review. Journal of Ultrasound in Medicine 36 (2017): 2361-2366.
- Attaran S, Shaw M, Bond L, Pullan MD, Fabri BM. Atrial fibrillation postcardiac surgery: a common but a morbid complication. Interactive Cardiovascular and Thoracic Surgery 12 (2011): 772-777.



 Impact Factor: * 3.5
Impact Factor: * 3.5 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 14.80%
Acceptance Rate: 14.80%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 