Age-Associated Changes in Value of the National Early Warning Score with the Japanese-Modified Glasgow Prognostic Score (NEWS-JmGPS) for Predicting In-Hospital Mortality of Elderly Patients Visiting the Emergency Department
Article Information
Toshiya Mitsunaga1,2*, Izumu Hasegawa1, Masahiko Uzura1, Kenji Okuno1, Akihiro Sekine2, Satoshi Takeda1
1 Department of Emergency Medicine, Jikei University School of Medicine, Tokyo, Japan
2 Centre for Preventive Medical Sciences, Chiba University, Chiba, Japan
*Corresponding author: Toshiya Mitsunaga, 3-25-8, Nishi-Shinbashi, Minato-ku, Tokyo, 1058471, Japan
Received: 24 December 2019; Accepted: 03 January 2020; Published: 06 January 2020
Citation: Toshiya Mitsunaga, Izumu Hasegawa, Masahiko Uzura, Kenji Okuno, Akihiro Sekine, Satoshi Takeda. Age-Associated Changes in Value of the National Early Warning Score with the Japanese-Modified Glasgow Prognostic Score (NEWS-JmGPS) for Predicting In-Hospital Mortality of Elderly Patients Visiting the Emergency Department. Archives of Clinical and Biomedical Research 4 (2020): 001-016.
View / Download Pdf Share at FacebookAbstract
Objective: The aim of this study is to evaluate the usefulness of the National Early Warning Score with the Japanese-modified Glasgow Prognostic Score (NEWS-JmGPS) for predicting in-hospital mortality of elderly patients. We also clarify the value of the NEWS-JmGPS for predicting in-hospital mortality of patients older than 75, 80, and 85 years.
Methods: This is secondary analysis of a retrospective, single-centred observational study conducted in one year, at the Emergency Department (ED) of Jikei University Kashiwa Hospital. A total of 1,830 acute medical patients age 65 and older were included in this study. Discrimination was assessed by plotting the receiver operating characteristics (ROC) curve and calculating the area under the ROC curve (AUC).
Results: The AUC of the NEWS-JmGPS was significantly higher than that of the NEWS for predicting in-hospital mortality (0.817 for the NEWSJmGPS, 0.797 for the NEWS) (p < 0.001). In the groups of older than 75 and 80 years, the AUC of NEWSJmGPS and NEWS for predicting in-hospital mortality were higher than those of the groups of younger than 75 and 80 years. On the other hand, in the group of older than 85 years, the AUC of NEWS-JmGPS and NEWS for predicting in-hospital mortality were lower than those of the group of younger than 85 years.
Conclusion: Our study demonstrated the utility of the NEWS-JmGPS as a strong predictor of in-hospital mortality in elderly patients. However, in the oldest-old patients older than 85 years, the NEWS-JmGPS does not have strong power for predicting in-hospital mortality.
Keywords
National Early Warning Score; Japanese modified Glasgow Prognostic Score; Elderly, Mortality; Emergency Department; Japan
National Early Warning Score articles, Japanese modified Glasgow Prognostic Score articles, Elderly articles, Mortality articles, Emergency Department articles, Japan articles
Article Details
Introduction
The growing ageing population is a major theme in public health worldwide. Life expectancy is increasing in many countries, and Japanese life expectancies are 81.1 years for men and 87.1 years for women, representing two of the highest in the world [1]. The percentage of people older than 65 years was 23.0% in 2010 and is expected to reach 29.1% by 2020 [2], and the number of patients older than 65 years presenting to EDs is increasing in parallel. As a result of the improving healthcare system, most of the people older than 65 years are healthy and people older than 75 years are defined as old people in Japan [3]. Moreover, one study has shown that the percentage that fails rapidly increases in people older than 80 years [4]. Overcrowding in hospital emergency departments (EDs) due to the high proportion of late-stage elderly patients has become a serious problem, and there is a critical need to make decisions for the efficient management of EDs as quickly as possible.
Several risk-scoring systems have been established to identify the risk of catastrophic deterioration and death of hospital inpatients. The National Early Warning Score (NEWS) was developed in 2012 in the UK by the National Early Warning Score Development and Implementation Group (NEWSDIG) on behalf of the Royal College of Physicians [5]. Several studies have explored the association between the NEWS and hospital admission or in-hospital mortality, and the findings suggest that the NEWS can also be used as a triage tool in EDs [6-8]. Although previous studies showed the good predictive value of the NEWS for in-hospital mortality for all adult patients, its predictive value for in-hospital mortality of elderly patients in our previous study was moderate [9].
The Glasgow Prognostic Score (GPS), which is based on inflammation criteria including serum C-reactive protein (CRP) and albumin, is a practical scoring system for the prognosis of patients with advanced cancer [10-14]. Recently, the studies conducted by Proctor et al. [15] and by Hirashima et al. [16] showed that the modified GPS (mGPS) is superior to GPS as a prognostic factor and that the Japanese-modified GPS (JmGPS), with a CRP cut-off of 0.5mg/dl, also has high value as a prognostic factor. Furthermore, a study conducted by Viviane et al. [17] showed that the mGPS correlates significantly with frailty in elderly patients.
To the best of our knowledge, no study has evaluated the value of the NEWS with the JmGPS (NEWS-JmGPS) for predicting in-hospital mortality of elderly patients, and it is still unclear whether the NEWS-JmGPS is superior to the original NEWS for predicting in-hospital mortality in this cohort. Moreover, there was also no study to compare the value of the NEWS-JmGPS for predicting in-hospital mortality in different cut-off of ages, the patients were divided at the age of 75 years, 80 years, and 85 years.
The aim of this study is to evaluate the value of the NEWS-JmGPS for predicting in-hospital mortality of patients older than 65 years who present to EDs. And we also clarify the value of the NEWS-JmGPS for predicting in-hospital mortality of patients older than 75 years, 80 years, and 85 years.
Materials & Methods
Study design
This was a planned secondary analysis of data from the retrospective, single-centred observational study conducted in one year between 1 April 2017 and 31 March 2018, at the ED of Jikei University Kashiwa Hospital (664 beds with approximately 8,500 ED visits annually) in Chiba, Japan. The study was conducted in order to evaluate the values of the NEWS-JmGPS for predicting in-hospital mortality in acute medical patients older than 65 years who came to the ED by ambulance.
Study setting and population
In Japan, emergency medical institutions nationwide are grouped into three categories: (1) primary emergency medical institutions, which treat patients with mild conditions and walk-in patients; (2) secondary emergency medical institutions, which treat patients with mild or moderate conditions that might require hospitalisation; and (3) tertiary emergency medical institutions, which treat or resuscitate seriously ill or injured patients [18]. Our hospital is a tertiary emergency medical institution that accepts approximately 5,000 cases brought to ED by ambulance annually. The population of the city of Kashiwa is about 415,000, and about 105,000 (25.3%) are people older than 65 years.
In this study, acute medical patients older than 65 years who arrived at the ED by ambulance during the study period were included. Patients who died before arriving at the hospital or were transferred to other hospitals from the ED were excluded.
Data sources and measurements
On arrival, all patients were first triaged by the chief nurse and guided to the appropriate emergency room. In some cases, each department’s doctors were called directly; the junior and senior residents of emergency medicine see all other patients who come to our ED; and the chief doctors of emergency medicine follow up all examinations, treatments, and dispositions. All data, including vital signs, were recorded in electronic medical records by the nurses during this process, and all serum biomarkers could be seen 30 minutes after samples were taken.
We calculated the first vital signs just after each patient arrived at the ED. All patients who presented at the ED were followed up through discharge or death for a maximum of 28 days. Data on patients’ in-hospital mortality was recorded. Diagnostic categories were based on the Major Diagnostic Categories (MDC) and classified as (1) Neurology, (2) Pulmonology, (3) Cardiology, (4) Gastroenterology, (5) Endocrinology, (6) Nephrology/Urology, (7) Hematology, (8) Collagen disease, (9) Otolaryngology, (10) Gynecology, (11) Dermatology, (12) Ophthalmology, (13) Psychology, (14) Toxicology or (15) Others.
We obtained complete information including age, gender, diagnostic categories, duration of stay in the ED, disposition, and in-hospital mortality. However, we were unable to obtain data regarding vital signs or serum biomarkers of some patients. There were two major reasons for missing values: (1) due to ED overcrowding, nurses were unable to input a patient’s information on the medical record, and (2) some patients went directly to treatment rooms such as otolaryngology. In the present study, missing values were not excluded, and substitutions were made using multiple imputation analysis.
The NEWS and the JmGPS were calculated using the recorded physiological parameters and serum biomarkers of the patients. The NEWS consists of seven parameters: respiratory rate, peripheral oxygen saturation, the presence of inhaled oxygen parameters, body temperature, systolic blood pressure, pulse rate and the AVPU (Alert, responds to Voice, responds to Pain, Unresponsive) score. The range for the NEWS is between 0 and 20 (Table 1). The AVPU score was derived from the Glasgow Coma Scale (GCS) as follows: A = 14–15, V = 9–13, P = 4–8, U = 3. The JmGPS was derived from two serum biomarkers: CRP and albumin. The JmGPS total ranges from 0 to 2 (Table 2), and the NEWS-JmGPS total ranges from 0 to a maximum of 22.
|
3 |
2 |
1 |
0 |
1 |
2 |
3 |
|
|
Respiratory rate (bpm) |
≤8 |
|
9−11 |
12−20 |
|
21−24 |
≥25 |
|
Oxygen saturation (%) |
≤91 |
92−93 |
94−95 |
≥96 |
|
|
|
|
Inhaled oxygen |
Yes |
No |
|||||
|
Temperature (▢) |
≤35.0 |
|
35.1−36.0 |
36.1−38.0 |
38.1−39.0 |
≥39.1 |
|
|
Systolic blood pressure (mmHg) |
≤90 |
91−100 |
101−110 |
111−219 |
≥220 |
||
|
Pulse rate (bpm) |
≤40 |
41−50 |
51−90 |
91−110 |
111−130 |
≥131 |
|
|
AVPU |
A |
V, P, or U |
Table 1: National Early Warning Score (NEWS)
AVPU; A, alert; V, to voice; P, to pain; U, to unresponsive; bpm, beats or breaths per minute.
|
Score |
|
|
0 |
CRP ≤ 0.5mg/dl |
|
1 |
CRP > 0.5mg/dl and Albumin ≥ 3.5g/dl |
|
2 |
CRP > 0.5mg/dl and Albumin < 3.5g/dl |
Table 2: Japanese modified Glasgow Prognostic Score (JmGPS)
CRP: C-reactive protein.
For in-hospital mortality, the patients were divided into two groups: survivors and non-survivors. For calculation of value of predicting in-hospital mortality in different cut-off ages, the patients were divided at the age of 75 years, 80 years, and 85 years.
Statistical analysis
The continuous variables were described as the medians and interquartile ranges, and they were compared using the Student’s t-test and the Mann–Whitney U-test. The categorical variables were described as a number (%) and were compared using Pearson’s χ2 test. ANOVA (analysis of variance) was used to compare differences among the three groups. The receiver operating characteristics (ROC) analysis and the area under the ROC curve (AUC) were used to evaluate the predictive value of the NEWS-JmGPS and the NEWS for in-hospital mortality. The cut-off values for the NEWS-JmGPS and the NEWS were determined by using Youden’s index (sensitivity + specificity-1). Using these determined cut-off points, the sensitivity, specificity, and odds ratio of the NEWS-JmGPS and the NEWS were calculated for the in-hospital mortality. A p-value of less than 0.05 was considered to indicate statistical significance. Sample size was calculated by EPV (event per variables). Peduzzi et al. [19] demonstrated that 10 EPVs were required for accurate estimation of regression coefficients in a logistic regression model. We calculated 9 variables for the NEWS-JmGPS in our study, so we needed more than 90 events. The previous studies reported that the mortality rates were 4.7% to 6.9% [20,21], and we assumed the mortality rate to be 5.8%. Finally, we set the sample size to 1,590 cases. Data were analysed using SPSS (version 16.0; SPSS Inc., Chicago, IL, USA).
Results
During the study period, 1,830 elderly patients were presented to the ED by ambulance. Of these, 250 cases (13.7%) were missing data for vital signs, 28 cases (1.5%) were missing data for biomarkers, and 237 cases (13.0%) were missing data for vital signs and biomarkers. We recovered the missing data completely using multiple imputation analysis.
The median age (interquartile range) of the patients was 78 (11) years, and 837 (45.7%) were females. The major diagnostic categories were 493 (26.9%) cardiology cases, 301 (16.4%) neurology cases, 306 (16.7%) gastroenterology cases, 173 (9.5%) pulmonology cases, 132 (7.2%) nephrology/urology cases, 131 (7.2%) otolaryngology, and 129 (7.0%) other cases (multi-organ failure, severe sepsis, heat stroke, etc.). The median length (interquartile range) of stay in the ED was 122 (116) minutes, and 715 (39.1%) patients were discharged from the ED; 764 (41.7%) patients were admitted to a ward; and 351 (19.2%) patients were admitted to the ICU. A total of 119 (6.5%) patients died within 28 days after being presented to the ED. In the complete-data group, the proportion of those discharged from the ED was smaller than that of those admitted to hospital. Moreover, the mortality rate was about four times higher in the complete-data group than in the incomplete-data group (Table 3).
|
Total population (n=1,830) Median (interquartile range) |
Data Complete Group (n=1315) |
Data Incomplete Group (n=515) |
p value (Complete group vs Incomplete group) |
|
|
Age, years |
78 (11) |
78 (11) |
78 (9) |
< 0.05 |
|
Sex [n (%)] |
< 0.01 |
|||
|
Male |
993 (54.3) |
741 (56.3) |
252 (48.9) |
|
|
Female |
837 (45.7) |
574 (43.7) |
263 (51.1) |
|
|
Diagnostic Category [n (%)] |
< 0.001 |
|||
|
Cardiology |
493 (26.9) |
434 (33.0) |
59 (11.5) |
|
|
Neurology |
301 (16.4) |
242 (18.4) |
59 (11.5) |
|
|
Gastroenterology |
306 (16.7) |
205 (15.6) |
101 (19.6) |
|
|
Pulmonology |
173 (9.5) |
146 (11.1) |
27 (5.2) |
|
|
Nephrology/Urology |
132 (7.2) |
78 (5.9) |
54 (10.5) |
|
|
Otolaryngology |
131 (7.2) |
36 (2.7) |
95 (18.4) |
|
|
Endocrinology |
36 (2.0) |
23 (1.7) |
13 (2.5) |
|
|
Hematology |
36 (2.0) |
22 (1.7) |
14 (2.7) |
|
|
Dermatology |
23 (1.3) |
13 (1.0) |
10 (1.9) |
|
|
Ophthalmology |
22 (1.2) |
1 (0.1) |
21 (4.1) |
|
|
Gynecology |
18 (1.0) |
10 (0.8) |
8 (1.6) |
|
|
Psychiatry |
18 (1.0) |
6 (0.5) |
12 (2.3) |
|
|
Toxicology |
7 (0.4) |
7 (0.5) |
0(0) |
|
|
Collagen disease |
5 (0.3) |
4 (0.3) |
1 (0.2) |
|
|
Others |
129 (7.0) |
88 (6.7) |
41 (8.0) |
|
|
Length of stay in ED [min] |
122 (116) |
131 (116) |
99 (109) |
< 0.001 |
|
Disposition [n (%)] |
< 0.001 |
|||
|
Discharge |
715 (39.1) |
358 (27.2) |
357 (69.3) |
|
|
Admission to a ward |
764 (41.7) |
619 (47.1) |
145 (28.2) |
|
|
Admission to ICU |
351 (19.2) |
338 (25.7) |
13 (2.5) |
|
|
Death [n (%)] |
119 (6.5) |
107 (8.1) |
12 (2.3) |
< 0.001 |
Table 3: Baseline characteristics of the study population
The median NEWS-JmGPS and the NEWS of non-survivors were significantly higher than those of survivors. The proportion of the presence of oxygen supplementation and poor status of consciousness of non-survivors was significantly higher than those of survivors. In addition, there were significant differences between survivors and non-survivors in regard to vital signs except for body temperature (Table 4).
|
Median (interquartile range) |
|||
|
Group1 |
Group 2 |
p value |
|
|
Age, years |
78 (11) |
80 (9) |
0.079 |
|
Sex [n (%)] |
0.109 |
||
|
Male |
920 (53.8) |
73 (61.3) |
|
|
Female |
791 (46.2) |
46 (38.7) |
|
|
Length of stay in ED [(min)] |
120 (113) |
159 (110) |
< 0.001 |
|
Respiratory rate (bpm) |
19 (7.0) |
22.0 (10.0) |
< 0.001 |
|
Oxygen saturation (%) |
98.0 (3.0) |
97.0 (5.0) |
< 0.001 |
|
Inhaled oxygen |
< 0.001 |
||
|
Yes |
552 (32.3) |
94 (79.0) |
|
|
No |
1159 (67.7) |
25 (21.0) |
|
|
Temperature (▢) |
36.6 (1.1) |
36.6 (1.3) |
0.083 |
|
Systolic blood pressure (mmHg) |
143 (40.0) |
127.0 (57.0) |
< 0.001 |
|
Pulse rate (bpm) |
85 (30.5) |
97.0 (27.5) |
< 0.001 |
|
AVPU [n (%) |
< 0.001 |
||
|
Alert |
1469 (85.9) |
54 (45.4) |
|
|
Voice |
158 (9.2) |
30 (25.2) |
|
|
Pain |
46 (2.7) |
13 (10.9) |
|
|
Unresponsive |
38 (2.2) |
22 (18.5) |
|
|
CRP (mg/dl) |
1 (4.2) |
4 (12.3) |
< 0.001 |
|
Albumin (g/dl) |
4 (0.8) |
3 (1.0) |
< 0.001 |
|
NEWS |
3 (5.0) |
8 (6.0) |
< 0.001 |
|
NEWS-JmGPS |
4 (5.0) |
9 (5.0) |
< 0.001 |
Table 4: Comparison of parameters between the survivors and non-survivors.
Data are presented as the median (interquartile range) for continuous variables and the number (%) for categorical variables. CRP, C-reactive protein; NEWS, National Early Warning Score; NEWS-JmGPS, National Early Warning Score with Japanese modified Glasgow Prognostic Score; bpm, beats or breaths per minute.
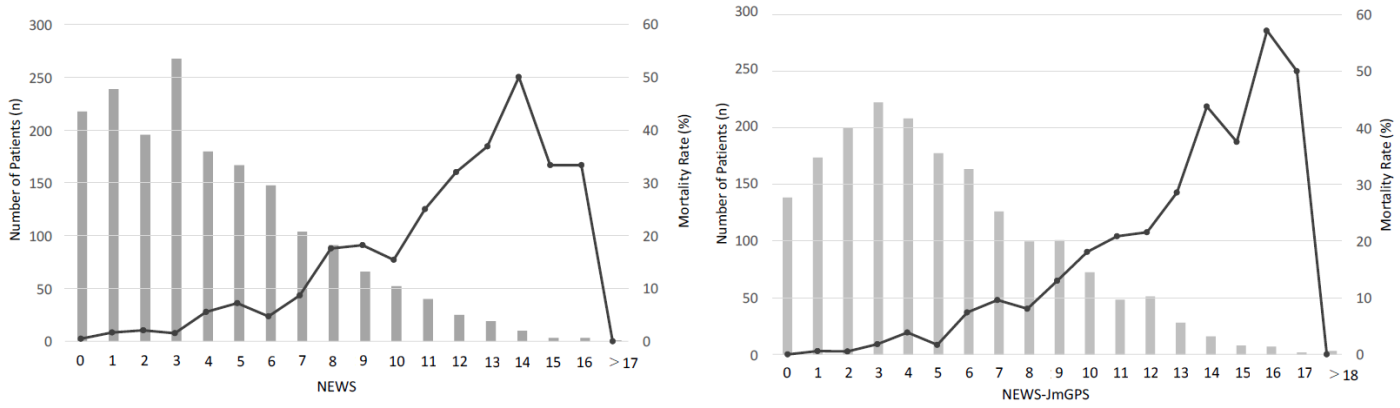
The evaluation of the mortality versus NEWS graph showed that when NEWS increased from 7 to 8, the in-hospital mortality rate increased from 8.7 to 17.6 %. Again, when NEWS increased from 10 to 11, the in-hospital mortality rate increased from 15.4 to 25.0 %. For this reason, the patients were divided into the following risk groups: NEWS less than 8, NEWS 8-10, and NEWS more than 10. A total of 1520 (83.1%) patients were in the NEWS less than 8 group, 209 (11.4%) were in the NEWS 8-10 group, and 101 (5.5%) were in the NEWS more than 10 group.
The evaluation of the mortality versus NEWS-JmGPS graph also showed that when NEWS-JmGPS increased from 5 to 6, the in-hospital mortality rate increased from 1.7 to 7.4 %. Again, when NEWS-JmGPS increased from 12 to 13, the in-hospital mortality rate increased from 21.6 to 28.6 %. From this finding, the patients were divided into the following risk groups: NEWS-JmGPS less than 6, NEWS-JmGPS 6-12, and NEWS-JmGPS more than 12. A total of 1109 (60.6%) patients were in the NEWS-JmGPS less than 6 group, 657 (35.9%) were in the NEWS-JmGPS 6-12 group, and 64 (3.5%) were in the NEWS-JmGPS more than 12 group (Figure 1).
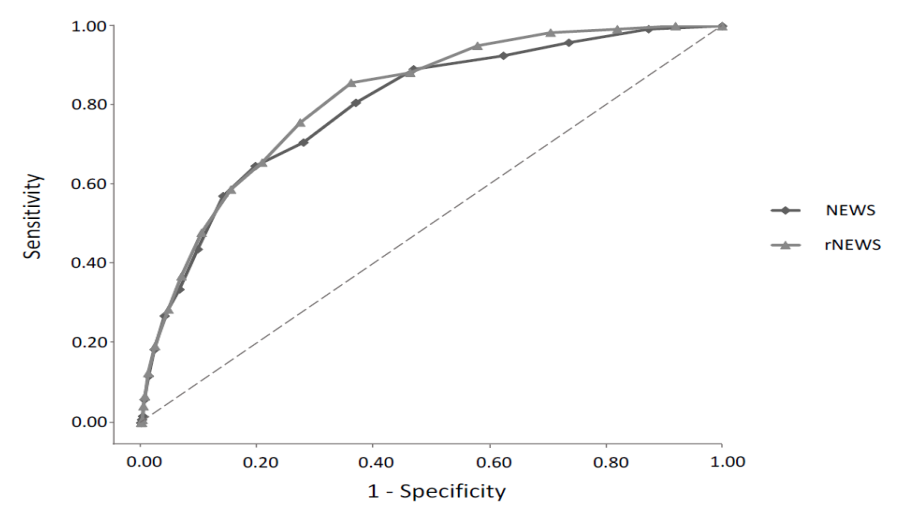
The AUC for predicting in-hospital mortality was 0.817 [95% CI 0.781 to 0.853, p < 0.001] for the NEWS-JmGPS and 0.797 [95% CI 0.756 to 0.837, p < 0.001] for the NEWS. The AUC of the NEWS-JmGPS was significantly higher than that of the NEWS for predicting in-hospital mortality (p < 0.001). The cut-off values for in-hospital mortality were 7 for the NEWS-JmGPS and 7 for the NEWS. The NEWS-JmGPS value of 7 or more had a sensitivity rate of 75.6%, a specificity rate of 72.6%, and an odds ratio of 8.22 for predicting in-hospital mortality. The NEWS of 7 or more had a sensitivity rate of 64.7%, a specificity rate of 80.3%, and an odds ratio of 7.47 for predicting in-hospital mortality (Figure 2).
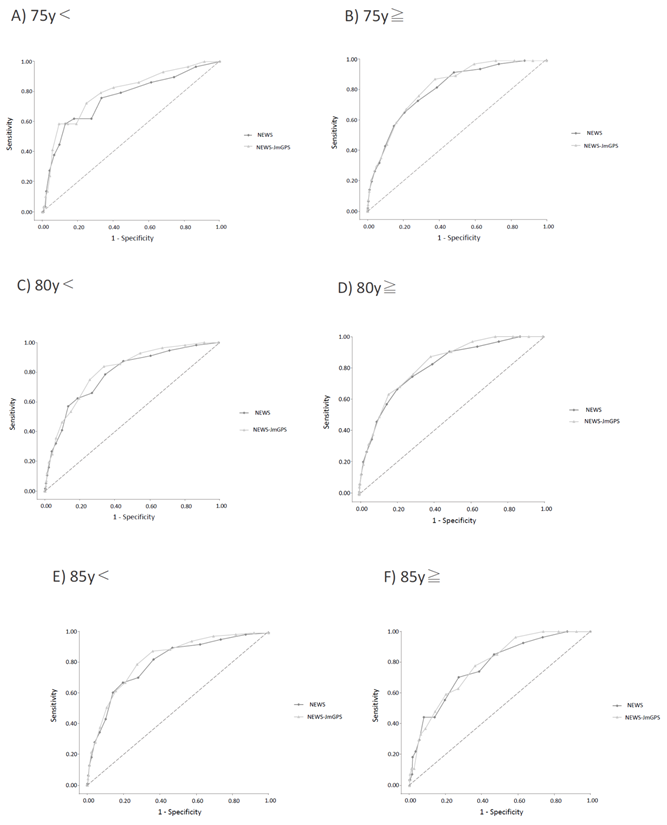
In the patients younger than 75 years, the AUC for predicting in-hospital mortality was 0.795 [95% CI 0.706 to 0.885, p < 0.001] for the NEWS-JmGPS and 0.759 [95% CI 0.657 to 0.860, p < 0.01] for the NEWS. The AUC of the NEWS-JmGPS was significantly higher than that of the NEWS for predicting in-hospital mortality (p < 0.001) (Figure 3A). In the patients older than 75 years, the AUC for predicting in-hospital mortality was 0.822 [95% CI 0.784 to 0.860, p < 0.001] for the NEWS-JmGPS and 0.807 [95% CI 0.764 to 0.850, p < 0.001] for the NEWS. The AUC of the NEWS-JmGPS was significantly higher than that of the NEWS for predicting in-hospital mortality (p < 0.05) (Figure 3B). In the patients younger than 80 years, the AUC for predicting in-hospital mortality was 0.809 [95% CI 0.755 to 0.863, p < 0.001] for the NEWS-JmGPS and 0.787 [95% CI 0.726 to 0.849, p < 0.001] for the NEWS. The AUC of the NEWS-JmGPS was significantly higher than that of the NEWS for predicting in-hospital mortality (p < 0.05) (Figure 3C). In the patients older than 80 years, the AUC for predicting in-hospital mortality was 0.821 [95% CI 0.773 to 0.869, p < 0.001] for the NEWS-JmGPS and 0.803 [95% CI 0.749 to 0.858, p < 0.001] for the NEWS. The AUC of the NEWS-JmGPS was significantly higher than that of the NEWS for predicting in-hospital mortality (p < 0.05) (Figure 3D).
In the patients younger than 85 years, the AUC for predicting in-hospital mortality was 0.826 [95% CI 0.786 to 0.866, p < 0.001] for the NEWS-JmGPS and 0.803 [95% CI 0.757 to 0.849, p < 0.001] for the NEWS. The AUC of the NEWS-JmGPS was significantly higher than that of the NEWS for predicting in-hospital mortality (p < 0.001) (Figure 3E). In the patients older than 85 years, the AUC for predicting in-hospital mortality was 0.785 [95% CI 0.706 to 0.864, p < 0.001] for the NEWS-JmGPS and 0.776 [95% CI 0.687 to 0.864, p < 0.001] for the NEWS. There was no significant difference between the AUC of the NEWS-JmGPS and that of NEWS for predicting in-hospital mortality (p=0.454) (Figure 3F).
- A) The patients younger than 75 years, B) The patients older than 75 years, C) The patients younger than 80 years, D) The patients older than 80 years, E) The patients younger than 85 years, F) The patients older than 85 years.
The cut-off values, sensitivity, specificity, and odds ratio for the prediction of in-hospital mortality in different cut-off ages were shown in Table 5. At the cut-off 85 years, the odds ratio as well as the AUC was reversed in young and old groups, compared with those of the groups at the cut-off 75 and 80 years (Table 5).
|
Score |
AUC (95% CI) |
Cut-off values |
Sensitivity |
Specificity |
Odds ratio |
|
[NEWS] Total population 75y< 75y> 80y< 80ygt; 85y< 85y> |
0.797 (0.756-0.837) 0.759 (0.657-0.860) 0.807 (0.764-0.850) 0.787 (0.726-0.849) 0.803 (0.749-0.858) 0.803 (0.757-0.849) 0.776 (0.687-0.864) |
7 5 6 5 6 7 6 |
64.7% 75.9% 73.3% 78.6% 74.6% 67.4% 70.4% |
80.3% 66.7% 71.9% 65.2% 71.1% 80.3% 72.8% |
7.47 6.29 7.04 6.88 7.21 8.41 6.36 |
|
[NEWS-JmGPS] Total population 75y< 75y> 80y< 80y> 85y< 85y> |
0.817 (0.781-0.853) 0.795 (0.706-0.885) 0.822 (0.784-0.860) 0.809 (0.755-0.863) 0.821 (0.773-0.869) 0.826 (0.786-0.866) 0.785 (0.706-0.864) |
7 7 7 7 7 7 6 |
75.6% 72.4% 76.7% 75.0% 76.2% 79.4% 77.8% |
72.6% 75.1% 71.4% 74.1% 70.7% 72.5% 63.7% |
8.22 7.93 8.20 8.59 7.70 10.11 6.15 |
Table 5: AUC, cut-off values, sensitivity, specificity, and odds ratio for the prediction of in-hospital mortality in different cut-off ages.
NEWS: National Early Warning Score; JmGPS: Japanese modified Glasgow Prognostic Score.
Discussion
Our single-centred, retrospective observational study demonstrated that the NEWS-JmGPS has higher predictive value for in-hospital mortality than the original NEWS. However, in the elderly patients older than 85 years, the AUC of NEWS-JmGPS and NEWS for predicting in-hospital mortality was lower than that in the patients younger than 85 years.
Several studies have evaluated the effectiveness of risk-scoring systems for predicting admissions to critical care units from wards or in-hospital mortality in the last decade; such systems were focused on in-hospital management [6, 8, 22]. Only a few studies that were conducted in an ED setting have shown the predictive value of the NEWS for hospitalisation or in-hospital mortality [23].
However, previous studies had several limitations, such as a relatively small number of people studied, and the performance of the risk-scoring system for elderly patients was unclear.
Several studies have evaluated that early warning scores with other biomarkers have strong power for predicting a patient’s prognosis. A study carried out by Rasmussen et al. [24] evaluated that the NEWS with Soluble Urokinase Plasminogen Activator Receptor (SuPAR) improves risk prediction. Another study carried out by Hasan et al. [25] demonstrated that the Modified Early Warning Score with rapid lactate level was also a powerful scoring system for detecting mortality of 65 years and older patients, and the AUC of the Modified Early Warning Score with rapid lactate level was 0.872 for in-hospital mortality.
In the previous study conducted by Anna et al. [6], the GPS showed moderate prognostic accuracy (AUC 0.67) in Emergency Department. Moreover, a study carried out by Rui et al. [27] demonstrated that the GPS is a strong predictor of poor prognosis in elderly patients with acute myocardial infarction.
In our study, we found that the NEWS-JmGPS is highly effective for predicting in-hospital mortality of elderly patients older than 65 years, and the AUC for in-hospital mortality was 0.817. Moreover, the AUC of the NEWS-JmGPS was significantly higher than that of the original NEWS for predicting in-hospital mortality.
A study conducted by Zerrin et al. [28] demonstrated that the VitalPac Early Warning Score (VIEWS), which was developed before the NEWS, was a powerful scoring system for use with elderly acute medical patients older than 65 years; the AUC of VIEWS was 0.756 for hospitalisation and 0.900 for in-hospital mortality. By contrast, one study carried out by Groot et al. [22] demonstrated the low prognostic performance of the NEWS for risk stratification in elderly septic patients older than 75 years but a higher prognostic performance in septic patients younger than 75 years. For this reason, in the patients older than 75 years, it might be difficult to expect the elderly patient’s prognosis by using these scores.
In the subgroup analysis of our study, the AUCs for in-hospital mortality of the patients older than 75 years and 80 years were higher than that of the patients younger than 75 years and 80 years. In contrast, the AUC for in-hospital mortality of the patients older than 85 years was lower than that of the patients younger than 85 years. The reason of these findings is that these oldest-old patients have several factors, such as frailty, dementia, and atypical physiological reaction that affect the variables that configure the score.
In previous studies by Abbott et al. [20, 21] the mortality rates were 4.7% (15 patients out of 322) to 6.9% (13 patients out of 189), and in our study, the in-hospital mortality rate was 6.5% (119 patients out of 1,830) within 28 days after admission, which is similar to the previous study. Furthermore, the EPV was 13.2, and we secured the number of event cases necessary for accurate estimation.
The NEWS has been introduced to the ED to predict patients’ prognoses in the United Kingdom.
No study has yet evaluated the usefulness of risk-scoring systems for predicting elderly patients’ prognoses in Japan. Because it is very difficult to predict the severity of illness in elderly patients who are delivered to emergency departments, we need to accumulate more evidence of the value of clinical risk scores in order to more clearly anticipate each patient’s prognosis and to perform appropriate and timely triage in the ED.
Our study has demonstrated that the NEWS-JmGPS has high utility as a predictor of in-hospital mortality. However, it takes several hours to get the results of biomarkers, and the original NEWS was determined to be faster than the NEWS-JmGPS. Therefore, it is difficult to introduce this revised score as a criterion for judging the need for admission or whether we should transport a patient to an intensive care unit as rapidly as possible.
This study has several limitations. First, it is a retrospective, single-centred study, and we did not evaluate the external validation. Second, the proportion of missing data was relatively high at about 30%. Third, in our study, discharged patients were not followed up in terms of readmissions to EDs and out-of-hospital mortality. These limitations may reduce the generalisability of the study. Combining risk-scoring systems and some biomarkers or other scores should be studied in order to determine those that are effective and rapid predictors of a patient’s prognosis.
Conclusions
According to the results of our study, the NEWS-JmGPS is a good predictor of in-hospital mortality among elderly patients, whereas the original NEWS is a moderate predictor of in-hospital mortality. However, in the oldest-old patients older than 85 years, the NEWS-JmGPS does not have strong power for predicting in-hospital mortality. Further evidence from multicentre studies is needed before introducing the new risk-scoring systems to the ED context.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Ethics approval
The protocol for this research was approved by a suitably constituted Ethics Committee of the institution and conforms to the provisions of the Declaration of Helsinki (Committee of Jikei University School of Medicine, Approval No. 30-094(9115)/ Committee of Chiba University, Approval No. 3229).
Acknowledgements
None
Conflicts of interest
None
References
- World Health Statistics 201 Monitoring health for the SDGs. https://apps.who.int/iris/bitstream/handle/10665/272596/9789241565585-eng.pdf?ua=1
- Lee YS, Lee JW, Lee J, et al. The usefulness of modified national early warning score with the age level in critically ill medical patients. Intensive Care Med Experimental 3 (2015): A834.
- Ouchi Y, Rakugi H, Arai H, et al. Redefining the elderly as aged 75 years and older: Proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatri Gerontol Int 17 (2017): 1045-1047.
- Francesco L, Alfonso JCJ, Rosa LAR, et al. Sarcopenia and mortality risk in frail older persons aged 80 years and older: results from ilSIRENTE study. Age Ageing 42 (2013): 203-209.
- Royal College of Physicians London. National Early Warning Score (NEWS): Standardising the assessment of acute-illness severity in the NHS. Report of working party. Royal college of Physicians.
- Subbe CP, Kruger M, Rutherford P, et al. Validation of a modified Early Warning Score in medical admissions. QJM - Int J Med 94 (2001): 521-6.
- Burch VC, Tarr G, Morroni C. Modified early warning score predicts the need for hospital admission and in hospital mortality. Emerg Med J 25 (2008): 674-8.
- Cei M, Bartolomei C, Mumoli N. In-hospital mortality and morbidity of elderly medical patients can be predicted at admission by the Modified Early Warning Score: A prospective study. Inter J Clin Prac 63 (2009): 591-5.
- Mitsunaga T, Izumu H, Masahiko U, et al. Comparison of the National Early Warning Score (NEWS) and the Modified Early Warning Score (MEWS) for predicting admission and in-hospital mortality in elderly patients in the pre-hospital setting and in the emergency department. Peer J 7 (2019): e6947.
- McMillan DC, Crozier JE, Canna K, et al. Evaluation of an inflammation-based prognostic score (GPS) in patients undergoing resection for colon and rectal cancer. Int J Colorectal Dis 22 (2007): 881-886.
- Kobayashi T, Teruya M, Kishiki T, et al. Inflammation-based prognostic score, prior to neoadjuvant chemoradiotherapy, predicts postoperative outcome in patients with esophageal squamous cell carcinoma. Surg 144 (2008): 729-735.
- Crumley AB, McMillan DC, McKernan M, et al. Evaluation of an inflammation-based prognostic score in patients with inoperable gastro-oesophageal cancer. Br J Cancer 94 (2006): 637-641.
- Glen P, Jamieson NB, McMillan DC, et al. Evaluation of an inflammation-based prognostic score in patients with inoperable pancreatic cancer. Pancreatology 6 (2006): 450-453.
- Forrest LM, McMillan DC, McArdle CS, et al. Comparison of an inflammation-based prognostic score (GPS) with performance status (ECOG) in patients receiving platinum-based chemotherapy for inoperable non-small-cell lung cancer. Br J Cancer 90 (2004): 1704-1706.
- Proctor MJ, Morrison DS, Talwar D, et.al. An inflammation-based prognostic score (mGPS) predicts cancer survival independent of tumor site: a Glasgow inflammation outcome study. Br J Cancer 104 (2011): 726-734.
- Hirashima K, Watanabe M, Shigaki H, et al. Prognostic significance of the modified Glasgow prognostic score in elderly patients with gastric cancer. J Gastroenterol 49 (2014): 1040-1046.
- Viviane L, Damila CT, Fernanda BFS, et al. Applicability of modified Glasgow Prognostic Score in the assessment of elderly patients with cancer: A pilot study. J Geriatr Oncol 6 (2015): 479-483.
- Tanigawa K, Tanaka K. Emergency medical service systems in Japan: Past. Present, and future. Resuscitation 69 (2006): 365-370.
- Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49 (1996): 1373-9.
- Abbott TEF, Torrance HDT, Cron N, et al. A single-centre cohort study of National Early Warning Score (NEWS) and near patient testing in acute medical admissions. Eur J Intern Med 35 (2016): 78-82.
- Abbott TE, Cron N, Vaid N, et al. Pre-hospital National Early Warning Score (NEWS) is associated with in-hospital mortality and critical care unit admission: A cohort study. Ann Med Surg 27 (2018): 17-21.
- Groot B, Stolwijk F, Warmerdam M, et al. The most commonly used disease severity scores are inappropriate for risk stratification of older emergency department sepsis patients: an observational multi-centre study. Scandinavian Journal of Trauma, Resuscitation Emerg Med 25 (2017): 91.
- Lee YS, Choi JW, Park YH, et al. Evaluation of the efficacy of the National Early Warning Score in predicting in-hospital mortality via the risk stratification. J Crit Care 47 (2018): 222-226.
- Rasmussen LJH, Ladelund SB, Haupt TH, et al. Combining National Early Warning Score With Soluble Urokinase Plasminogen Activator Receptor (suPAR) Improves Risk Prediction in Acute Medical Patients: A Registry-Based Cohort Study. Crit Care Med 12 2018): 1961-1968.
- Hasan BC, Ozlem K, Deniz S, et al. The predictive value of the modified early warning score with rapid lactate level (ViEWS-L) for mortality in patients of age 65 or older visiting the emergency department. Intern Emerg Med 12 (2017): 1253-1257.
- Anna CR, Alexander K, Susan F, et al. Procalcitonin Improves the Glasgow Prognostic Score for Outcome Prediction in Emergency Patients with Cancer: A Cohort Study. Dis Markers 2015: 9.
- Rui W, Xiaodan W, Cheng H, et al. Association between inflammation-based prognostic scores and in-hospital outcomes in elderly patients with acute myocardial infarction. Clin Intervent Aging 14 (2019): 1199-1206.
- Zerrin DD, Mehmet E, Mehmet AK, et al. Modified Early Warning Score and VitalPac Early Warning Score in geriatric patients admitted to emergency department. Eur J Emerg Med 23 (2016): 406-412.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 