Burnout Leads to Premature Surgeon Retirement: A Nationwide Survey
Article Information
Nicole Cimbak1, Allan Stolarski1, Jennifer Moseley2, Patrick O’Neal2, Edward Whang2,3, Gentian Kristo2,3*
1Department of Surgery, Boston Medical Center, Boston University, Boston, MA, USA
2Department of Surgery, Veterans Affairs Boston Healthcare System, Boston, MA, USA
3Department of Surgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA
*Corresponding Author: Gentian Kristo, Department of Surgery, Veterans Affairs Boston Healthcare System (116-C), 1400 VFW Parkway, West Roxbury, Boston, MA 02132, USA
Received: 12 August 2019; Accepted: 28 August 2019; Published: 02 September 2019
Citation: Nicole Cimbak, Allan Stolarski, Jennifer Moseley, Patrick O’Neal, Edward Whang, Gentian Kristo. Burnout Leads to Premature Surgeon Retirement: A Nationwide Survey. Journal of Surgery and Research 2 (2019): 159-169.
View / Download Pdf Share at FacebookAbstract
Background: Retirement of surgeons has important workforce implications given the shortage of surgeons throughout the country. Our study was designed to evaluate factors that influence surgeon retirement decisions.
Material and methods: A paper-based survey regarding retirement decisions was mailed nationwide from April to June of 2018 to retired General, Colorectal, Vascular, and Cardiothoracic surgeons that are members of the American College of Surgeons.
Results: A total of 2295 of 5282 surveys were completed (43.4% response rate). The mean age of respondents was 79.0 ± 0.8 years, their mean age of retirement was 63.9 ± 0.1 years, and their mean interval since retirement was 15.2 ± 0.9 years. The five most common reasons for retirement were advancing age, personal health, increased outside interference, burnout, and worsening malpractice environment. The most common reported health problems leading to retirement were musculoskeletal disorders. The percentage of reported burnout was significantly lower in academic surgeons (5.8%) vs. surgeons in private practice (10.5%); academic/private practice combination (10.0%); those employed by community hospital or health system (11.4%); and Veteran Affairs institution, military hospital, and Indian Health Service (13.8%). Burnout was the only factor associated with an earlier retirement age (61.2 ± 0.4 years vs. 65.8 ± 0.2 years in the absence of burnout). Results were comparable when stratified by surgical specialty.
Conclusion: Our survey brings awareness to potentially-modifiable factors influencing surgeon retirement, such as outside interference, occupational health problems, burnout, and worsening malpractice env
Keywords
Surgeon retirement, Occupational health, Burnout
Surgeon retirement articles, Occupational health articles, Burnout articles
Surgeon retirement articles Surgeon retirement Research articles Surgeon retirement review articles Surgeon retirement PubMed articles Surgeon retirement PubMed Central articles Surgeon retirement 2023 articles Surgeon retirement 2024 articles Surgeon retirement Scopus articles Surgeon retirement impact factor journals Surgeon retirement Scopus journals Surgeon retirement PubMed journals Surgeon retirement medical journals Surgeon retirement free journals Surgeon retirement best journals Surgeon retirement top journals Surgeon retirement free medical journals Surgeon retirement famous journals Surgeon retirement Google Scholar indexed journals Occupational health articles Occupational health Research articles Occupational health review articles Occupational health PubMed articles Occupational health PubMed Central articles Occupational health 2023 articles Occupational health 2024 articles Occupational health Scopus articles Occupational health impact factor journals Occupational health Scopus journals Occupational health PubMed journals Occupational health medical journals Occupational health free journals Occupational health best journals Occupational health top journals Occupational health free medical journals Occupational health famous journals Occupational health Google Scholar indexed journals Burnout articles Burnout Research articles Burnout review articles Burnout PubMed articles Burnout PubMed Central articles Burnout 2023 articles Burnout 2024 articles Burnout Scopus articles Burnout impact factor journals Burnout Scopus journals Burnout PubMed journals Burnout medical journals Burnout free journals Burnout best journals Burnout top journals Burnout free medical journals Burnout famous journals Burnout Google Scholar indexed journals musculoskeletal disorders articles musculoskeletal disorders Research articles musculoskeletal disorders review articles musculoskeletal disorders PubMed articles musculoskeletal disorders PubMed Central articles musculoskeletal disorders 2023 articles musculoskeletal disorders 2024 articles musculoskeletal disorders Scopus articles musculoskeletal disorders impact factor journals musculoskeletal disorders Scopus journals musculoskeletal disorders PubMed journals musculoskeletal disorders medical journals musculoskeletal disorders free journals musculoskeletal disorders best journals musculoskeletal disorders top journals musculoskeletal disorders free medical journals musculoskeletal disorders famous journals musculoskeletal disorders Google Scholar indexed journals surgical workforce articles surgical workforce Research articles surgical workforce review articles surgical workforce PubMed articles surgical workforce PubMed Central articles surgical workforce 2023 articles surgical workforce 2024 articles surgical workforce Scopus articles surgical workforce impact factor journals surgical workforce Scopus journals surgical workforce PubMed journals surgical workforce medical journals surgical workforce free journals surgical workforce best journals surgical workforce top journals surgical workforce free medical journals surgical workforce famous journals surgical workforce Google Scholar indexed journals Cardiothoracic surgeons articles Cardiothoracic surgeons Research articles Cardiothoracic surgeons review articles Cardiothoracic surgeons PubMed articles Cardiothoracic surgeons PubMed Central articles Cardiothoracic surgeons 2023 articles Cardiothoracic surgeons 2024 articles Cardiothoracic surgeons Scopus articles Cardiothoracic surgeons impact factor journals Cardiothoracic surgeons Scopus journals Cardiothoracic surgeons PubMed journals Cardiothoracic surgeons medical journals Cardiothoracic surgeons free journals Cardiothoracic surgeons best journals Cardiothoracic surgeons top journals Cardiothoracic surgeons free medical journals Cardiothoracic surgeons famous journals Cardiothoracic surgeons Google Scholar indexed journals surgeon’s posture articles surgeon’s posture Research articles surgeon’s posture review articles surgeon’s posture PubMed articles surgeon’s posture PubMed Central articles surgeon’s posture 2023 articles surgeon’s posture 2024 articles surgeon’s posture Scopus articles surgeon’s posture impact factor journals surgeon’s posture Scopus journals surgeon’s posture PubMed journals surgeon’s posture medical journals surgeon’s posture free journals surgeon’s posture best journals surgeon’s posture top journals surgeon’s posture free medical journals surgeon’s posture famous journals surgeon’s posture Google Scholar indexed journals open surgery articles open surgery Research articles open surgery review articles open surgery PubMed articles open surgery PubMed Central articles open surgery 2023 articles open surgery 2024 articles open surgery Scopus articles open surgery impact factor journals open surgery Scopus journals open surgery PubMed journals open surgery medical journals open surgery free journals open surgery best journals open surgery top journals open surgery free medical journals open surgery famous journals open surgery Google Scholar indexed journals surgeon retirement articles surgeon retirement Research articles surgeon retirement review articles surgeon retirement PubMed articles surgeon retirement PubMed Central articles surgeon retirement 2023 articles surgeon retirement 2024 articles surgeon retirement Scopus articles surgeon retirement impact factor journals surgeon retirement Scopus journals surgeon retirement PubMed journals surgeon retirement medical journals surgeon retirement free journals surgeon retirement best journals surgeon retirement top journals surgeon retirement free medical journals surgeon retirement famous journals surgeon retirement Google Scholar indexed journals Premature Surgeon articles Premature Surgeon Research articles Premature Surgeon review articles Premature Surgeon PubMed articles Premature Surgeon PubMed Central articles Premature Surgeon 2023 articles Premature Surgeon 2024 articles Premature Surgeon Scopus articles Premature Surgeon impact factor journals Premature Surgeon Scopus journals Premature Surgeon PubMed journals Premature Surgeon medical journals Premature Surgeon free journals Premature Surgeon best journals Premature Surgeon top journals Premature Surgeon free medical journals Premature Surgeon famous journals Premature Surgeon Google Scholar indexed journals
Article Details
1. Introduction
Unlike some other professions, surgery has no federally mandated retirement age in the United States, ultimately leaving the decision to retire up to the individual surgeon [1]. Understanding the factors that contribute to the surgeon’s decision to retire has important workforce implications given the shortage of surgeons throughout the country [2]. However, the reasons why surgeons decide to retire have not been adequately explored. A few studies report personal health decline and concern with compensation as reasons to retire [3]. One systematic review of retirement planning among all physicians reported the most common retirement age between 60-69 years, with only a minimal number of studies in this review being specifically based on retirement plans of surgeons [4]. Given the paucity of data on the recent retirement plans of surgeons in particular and the importance of this data for predicting the future of the surgical workforce, this study aims to identify the average age of retirement as well as major reasons why surgeons retire. This information can help to inform data on the overall outflow of surgeons from the workforce through retirement. With the surgeon shortage on the horizon, understanding why surgeons retire can serve as valuable fodder for future interventions to sustain our current workforce and to help inform future generations about retirement planning.
2. Methods
A list of possible survey questions was generated from interviews with young and senior practicing attending surgeons. Survey validity was assessed via a 30 minutes focus group session with three retired surgeons. After the survey was pilot-tested in a small group of 5 retired surgeons, we modified the survey questions based on their feedback. A survey consisting of 15 questions (8 open-ended; 5 multiple-choice; 2 yes/no) was mailed nationwide from April to June of 2018 to all retired General, Colorectal, Vascular, and Cardiothoracic surgeons that are members of the American College of Surgeons (Table 1).
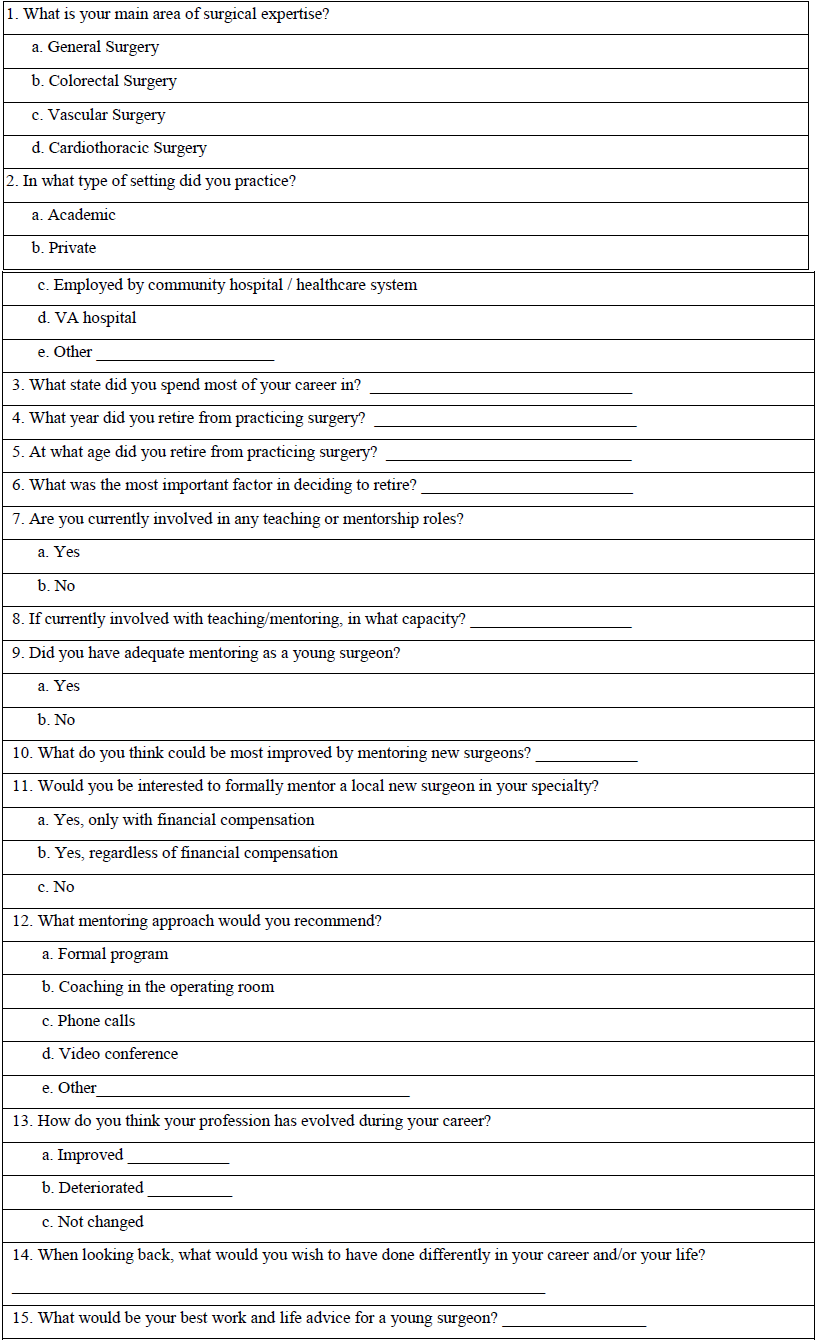
Table 1: Survey of Retired Surgeons.
All data were collected in accordance with the requirements of our Institutional Review Board. Completion of the survey was voluntary, and anonymity was ensured by not requiring any personal identifiers. Only surveys with >80% of items completed were included in the analysis. Results were calculated based on the number of responses received to each individual question. Free-text responses from open-ended questions were independently coded and the resulting nominal data are presented as percentage of responses per category. Data were analyzed with SAS statistical. Chi-square test was used to measure the relationship between nominal scale variables. The Mann-Whitney rank sum test was used to compare ordinal scale variables. Data are presented as mean (± SEM) where appropriate. A p value of <0.05 was considered statistically significant.
3. Results
From a total of 5876 surveys that were mailed, 462 envelopes were returned due to a change of address, 9 surgeons were medically unable to complete the questionnaire (as reported by their family members), and 123 surgeons had passed away by the time the survey reached their address. A total of 2295 of 5282 surveys were completed, for an overall response rate of 43.4 percent. At least one survey participant from 50 states and Washington D.C. responded.
3.1 Demographics
The mean age of respondents was 79.0 ± 0.8 years, their mean age of retirement was 63.9 ± 0.1 years, and their mean interval since retirement was 15.2 ± 0.9 years. The vast majority (99.2%) of respondents were males. Most retired surgeons were in private practice (66.4%), with other practice environments including academic teaching hospital (12%), academic/private combination (11.3%), employment by community hospital or health system (6.4%), Veteran Affairs institution (2.7%), military hospital (1%), and Indian Health Service (0.09%).
3.2 Reasons for retirement
The most common reason for retirement was advancing age followed by personal health; increased outside interference; burnout; worsening malpractice environment; desire to pursue other interests and hobbies; spending more time with family; high call frequency; decreasing reimbursements; desire to retire “at top of the game”; fatigue, family member health issue; advent of Electronic Medical Records; financial stability; and institutional retirement age mandate (Figure 1). Other factors (9.3%) influencing retirement decision included inability to professionally slow down prior to retirement; decreased patient referrals; increased practice costs; advent of new surgical techniques; change of practice location; closure of practice; workplace conflicts; pursuing a non-surgical career; transitioning to administrative role; medical disability; death of spouse, child, or close friend; recent lawsuits; frustration with institutional politics; sexual harassment; and gender discrimination. Among 372 (16.2%) surgeons who retired for personal health reasons, 277 participants (74.5%) offered specific information on their health issues. The most common reported health problems leading to retirement were musculoskeletal disorders (affecting, in order of frequency, the back, hands, lower extremities, and neck) followed by decreased vision, heart disease (such as cardiac dysrhythmia, myocardial infarction, coronary bypass grafting surgery, other heart surgeries, and cardiac arrest), non-work related injuries, stroke, cancer diagnosis, intentional hand tremor, Parkinson’s disease, decreased hearing, and multiple sclerosis (Figure 2).
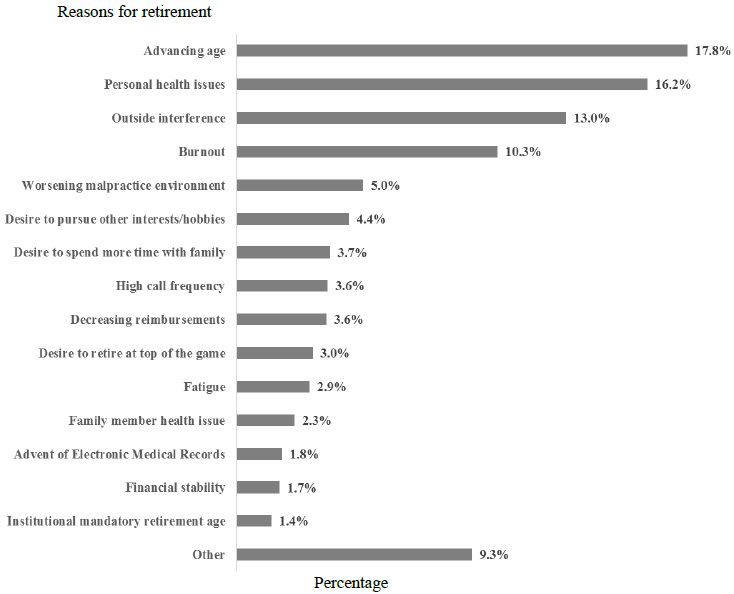
Figure 1: Reasons for retirement.
Other reported health problems (7.9%) influencing retirement decision included latex allergy; severe hypertension; renal failure, hepatitis C infection; liver failure secondary to hepatitis A; major depression; stress-induced asthma; abdominal aortic aneurysm surgery; autoimmune disease; encephalitis; amyotrophic lateral sclerosis; and chemotherapy-induced immunosuppression. The percentage of reported burnout was significantly lower in academic surgeons vs. surgeons in private practice, academic/private practice combination, those employed by community hospital or health system, and surgeons in Veteran Affairs institution, military hospital, and Indian Health Service (Figure 3). Logistic regression showed that burnout was the only factor associated with a significantly earlier retirement age (61.2 ± 0.4 years vs. 65.8 ± 0.2 years in the absence of burnout). Results were comparable when stratified by surgical specialty. Among 236 (10.3%) surgeons who retired due to burnout, 53 participants (22.5%) offered specific information on the cause of their burnout. The most common reason for burnout leading to retirement was a high number of nights and weekends on call (43.4%), followed by increased regulatory interference (28.3%), and a feeling of being overworked (15.1%). Other burnout reasons (13.2%) included lack of support in the workplace, toxic institutional politics, and being sued for malpractice.
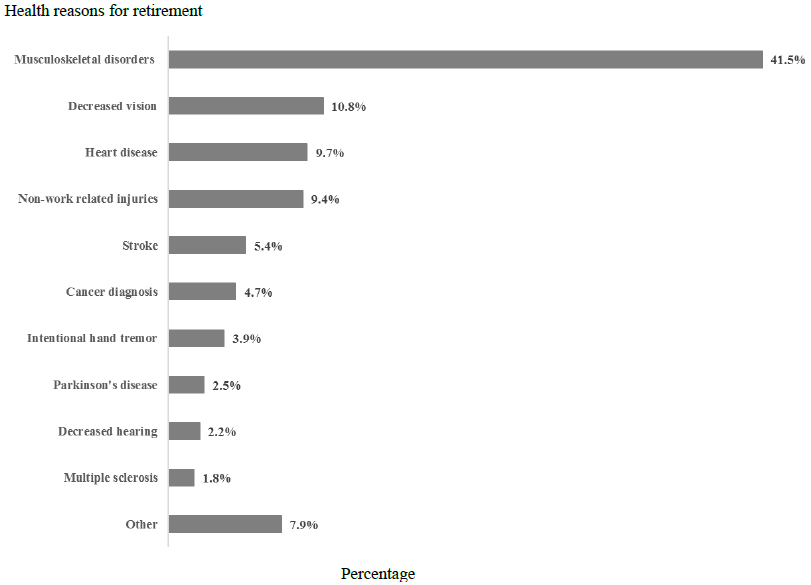
Figure 2: Health-related retirement reasons.
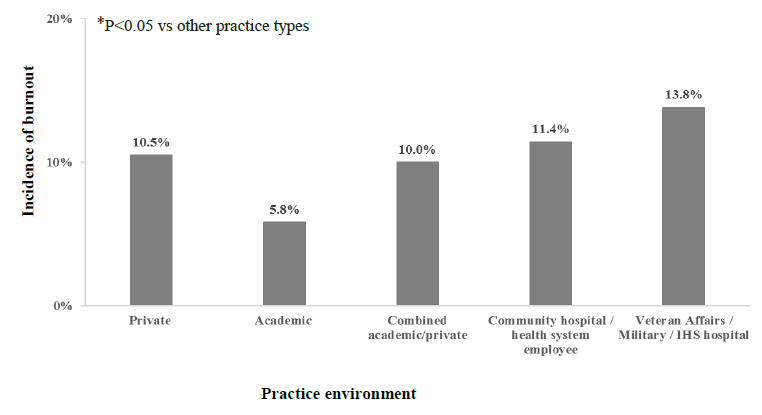
Figure 3: Incidence of burnout according to the practice setting.
4. Discussion
The mean age of retirement reported in our nationwide survey was 63.9 years, which is consistent with findings of other studies [4]. The principle reason for retirement was advanced age followed by personal health. Musculoskeletal (MSK) issues were the most common health reason our respondents chose to retire. This is line with other studies that have found a high prevalence of MSK disorders in surgeons [5]. It comes as no surprise that the physical demands of being a surgeon are often compared to those of highly physically demanding jobs such as coal miners, firefighters, and construction workers. Surgeons often spend extended hours standing in stationary positions completing repetitive movements. In one study by Szeto et al. [6], researchers were able to measure the movements of surgeons intra-operatively with the use of biaxial inclinometer. They found that surgeons generally held a flexed neck position in open surgery and an extended neck position during laparoscopic surgeries, along with external factors such as screen monitor, operative table height that affect the surgeon’s posture.
These positions in the operating room are thought to be the source of many MSK issues for surgeons. Evidence suggests that neck and back pain are the most common complaints among work-related MSK pathology [5, 7]. Additionally, surgeons start experiencing MSK pain symptoms at ages as young as 35 [7]. The pain experienced by surgeons extends beyond the operative room-studies found that of those surgeons who report pain while operating, 41% endorse that this pain affects their relationships with other people and 50% said that the pain of operative interferes with sleep [8]. One study reported that surgeons experiencing MSK pain required a leave of absence, practice restriction, or even early retirement in 12% of cases [5].The results of our study align with this conclusion.
Increased awareness of intraoperative ergonomic risks to surgeons had led to exploration of various protective interventions. One randomized control trial [9] compared physical performance and mental focus between two groups: one group participated in “microbreaks” during operations while the other group was the control arm. Authors defined microbreaks as 1.5-2-minute exercises in the sterile field every 40 minutes while operating. The intervention was shown to significantly reduce pain reported in neck and shoulders and equally important, 34% of surgeons reported an increase in mental focus after the microbreak intervention. The success of this study is exemplified by the fact that 87% of participants hoped to implement microbreaks as standard practice in their institution. Other ergonomic interventions described include ergonomics devices (anti-fatigue floor mats and supportive furniture), ergonomically improved medical technology (alternative video displays for microsurgery), and personalized ergonomic assessment programs to educate surgeons on the importance of the neutral posture during operations [5, 10, 11].
In addition to MSK-related occupational health problems, our study identified that outside interference, worsening malpractice environment, and burnout are three significant and potentially-modifiable factors for surgeon retirement. In the recent era of healthcare reform, particularly from increased governmental influences, insurance companies, and hospital administration, many physicians perceive a decrease in their professional autonomy. Our findings are supported by similar evidence that suggests premature physician retirement is related to the job dissatisfaction resulting from this perceived reduced autonomy [4, 12].
Surgical specialties have a high malpractice risk that increases with age [13]. Among surgeons, 80% are projected to face a malpractice claim by the age of 45 years, and 99% by the age of 65 years [13]. In line with existing evidence [4, 14] our study shows that many surgeons choose to retire when faced with increasing litigation risk and rising malpractice insurance premiums. In particular, the impact of physician burnout has serious negative career implications. Our survey revealed that surgeon burnout decreases the average retirement age by 4.6 years, which is in line with studies that have similarly evaluated the negative career implications of physician burnout [15-17]. Excessive workload and increased bureaucracy were reported by our survey participants as the two most important causes for their burnout.
Similar to other studies [18], we showed that academic surgeons reported the lowest incidence of burnout among different practice settings. Although we did not explore reasons for this significant finding, we believe that it is due to different workplace challenges faced by surgeons in academic vs. non-academic practice. In a survey of the American College of Surgeons membership in 2008, Balch et al. [19] showed that burnout risk factors may differ in academic vs. private practice surgeons. For academic surgeons, more nights on call and hours worked were factors strongly associated with burnout. In private practice, the strongest burnout factors were significant time spent for non-clinical activities and having incentive-based pay.
In our survey, burnout was reported the most by VA, military, and IHS surgeons. The reasons for these high burnout reports remains undetermined. Although there are no studies that have specifically explored surgeon burnout in these three practice settings, in a survey examining burnout profiles in all VA employees, Yanchus et al. [20] found the lack of personal accomplishments in the workplace to be the main driver of burnout.
Interventions for surgeon burnout must be multi-factorial in order to address the complex etiology of this issue. One meta-analysis identified a wide variety of burnout interventions at the individual physician level including: how to manage the stress of a medical practice with interpersonal and communication skills training, mindfulness-based meditation, and behavioral therapy [21]. West et al. [22] report that many of the studied interventions can reduce overall burnout by 10% and decrease feelings of emotional exhaustion and depersonalization. However, we believe that promoting surgeon well-being is a multi-faceted process that should be addressed not only by individual surgeons but also through structural and regulatory interventions by professional organizations and workplace occupational leadership. Understanding the specific burnout risk profile of different practice settings is very important as it could inform development of surgeon wellness programs tailored to the underlying workplace risk factors for burnout.
Our study is subject to a number of limitations. First, our survey was distributed only to retired surgeons who are members of the ACS. A response bias may exist such that retired surgeons who retain their ACS membership are more likely to complete surveys due to ongoing interest in the topic of surgeon retirement. Second, with a response rate of 43.4%, we cannot exclude meaningful differences between retired surgeons who answered our questionnaire and the non-respondents. The wide distribution of our survey and representation of all states, various practice environments, and different surgical specialties helps mitigate non-response bias. Third, because our survey is national, we are unable to determine retirement factors related to geography and local practice culture and regulations. Last but not least, women are under-represented in this study, constituting only 1.2% of survey recipients and 0.8% of respondents. This is very important as female surgeons may face a different set of workplace and retirement challenges. For instance, in our study sexual harassment and gender discrimination were reported as retirement factors only by female surgeons. In our opinion the low female representation in our study is an illustration of the major gender gap that, while has historically persisted in surgery, it was more severe decades ago, when the current generation of retired surgeons was starting their training [23, 24]. This gender cap calls for research dedicated to exploring specific reasons on how and why female surgeons decide to retire.
These limitations notwithstanding, we believe our findings provide meaningful insights into factors that influence surgeon retirement decisions.
Conclusions
Our survey brings awareness to potentially-modifiable factors influencing surgeon retirement, such as occupational health problems, outside interference, worsening malpractice environment, and burnout. To prevent surgeon shortage greater attention should be focused on supporting surgeons adjust adequately to regulatory policy changes, improving surgeon well-being, and providing fair malpractice protection.
Author Contributions
- Study concept and design: Cimbak; Whang, Kristo
- Acquisition of data: Cimbak; Moseley; Kristo
- Analysis and interpretation of data: Cimbak; Oneal; Whang; Kristo
- Drafting of manuscript: Cimbak; Stolarski; Kristo
- Critical revision: Cimbak; Stolarski, Oneal; Whang; Kristo
The Author Disclosure Statement
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
References
- Greenfield LJ, Proctor MC. Attitudes toward retirement. A survey of the American Surgical Association. Ann Surg 220 (1994): 382-390.
- Smart DR. Physician Characteristics and Distribution in the U.S. Chicago, IL. American Medical Association (2006).
- Jackson TN, Pearcy CP, Truitt M, et al. The Physician Attrition Crisis: A Cross-Sectional Survey of the Risk Factors for Reduced Job Satisfaction Among US Surgeons. World Journal of Surgery 42 (2018): 1285-1292.
- Silver MP, Hamilton AD, Biswas A, et al. A systematic review of physician retirement planning. Hum Resour Health 14 (2016): 1-16.
- Epstein S, Sparer EH, Tran BN, et al. Prevalence of Work-Related Musculoskeletal Disorders Among Surgeons and Interventionalists: A Systematic Review and Meta-analysis. JAMA Surg 153 (2018): 174947.
- Szeto GP, Cheng SW, Poon JT, et al. Surgeons' static posture and movement repetitions in open and laparoscopic surgery. J Surg Res 172 (2012): 19-31.
- Soueid A, Oudit D, Thiagarajah S, et al. The pain of surgery: pain experienced by surgeons while operating. International Journal of Surgery 8 (2010): 118-210.
- Cleeland CS, Ryan, KM. Pain assessment: global use of the brief pain inventory. Ann Acad Med Singap 23 (1994): 129-138.
- Hallbeck MS, Lowndes BR, Park AE, et al. The impact of intraoperative microbreaks with exercises on surgeons: A multi-center cohort study. Applied Ergonomics 60 (2017): 334-341.
- Schurr MO, Buess GF, Botsch M, et al. Ergonomic surgeon's chair for use during minimally invasive surgery. Surg Laparosc Endosc Percutan Tech 9 (1999): 244-247.
- Albayrak A, van Veelen MA, Kazemier G, et al. A newly designed ergonomic body support for surgeons. Surg Endosc 21 (2007): 1835-1840.
- National Physician Outlook and Practice Trends Report (2013).
- Anupam B, Jena AB, Chandra A, et al. Malpractice Risk According to Physician Specialty. N Engl J Med 365 (2011): 629-636.
- Medical Liability Monitor.
- Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu rev Psychol 52 (2001): 397-422.
- Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Archives of surgery 144 (2009): 371.
- Shanafelt TD, Balch CM, Freischlag J, et al. Burnout and medical errors among American surgeons. Annals of surgery 251 (2010): 995.
- Varkey P, Boone LS, Shanafelt TD, et al. Physician Satisfaction and Burnout at Different Career Stages. Mayo Clin Proc 88 (2013): 1358-1367.
- Balch CM, Shanafelt TD, Freischlag JA, et al. Distress and career satisfaction among 14 surgical specialties, comparing academic and private practice settings. Annals of surgery 254 (2011): 558-568.
- Yanchus NJ, Beckstrand J, Osatuke K. Examining burnout profiles in the Veterans Administration: All Employee Survey narrative comments. Burnout Research 2 (2015): 97-107.
- Wiederhold BK, Cipresso P, Riva G, et al. Intervention for Physician Burnout: A Systematic Review. Open Med (Wars) 13 (2018): 253-263.
- West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 388 (2016): 2272-2281.
- Wirtzfeld DA. The history of women in surgery. Can J Surg 52 (2009): 317-320.
- Freischlag JA. Women surgeons--still in a male-dominated world. Yale J Biol Med 81 (2008): 203-204.


 Impact Factor: * 4.2
Impact Factor: * 4.2 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 