Cavernous Hemangioma: Uncommon Cause of Obscure Gastrointestinal Bleeding Diagnosed by Video Capsule Endoscopy and Contrast Enhanced Computed Tomography
Article Information
Roberto Monreal-Robles, Angel Noe del Cueto- Aguilera, Diego García-Compean*, José Alberto González- González, Omar David Borjas-Almaguer, Joel Omar Jaquez-Quintana, Héctor Jesus Maldonado Garza
Servicio de Gastroenterología y Endoscopia Digestiva, Departamento de Medicina Interna, Hospital Universitario “Dr. José E. González”, Universidad Autónoma de Nuevo León. Ave. Madero y Gonzalitos S/N, Monterrey, NL, México
*Corresponding Author: Dr. Diego García-Compean, MMSc. Gastroenterology Service and Department of Internal Medicine. University Hospital "Dr. José E. González” and Faculty of Medicine. Universidad Autónoma de Nuevo León. Madero y Gonzalitos S/N, Monterrey NL, México
Received: 10 April 2020; Accepted: 24 April 2020; Published: 28 May 2020
Citation: Angel Noe del Cueto- Aguilera, Roberto Monreal-Robles, Diego García-Compean, José Alberto González- González, Joel Omar Jaquez-Quintana, Héctor Jesus Maldonado Garza. Cavernous Hemangioma: Uncommon Cause of Obscure Gastrointestinal Bleeding Diagnosed by Video Capsule Endoscopy and Contrast Enhanced Computed Tomography. Archives of Clinical and Medical Case Reports 4 (2020): 512-519.
View / Download Pdf Share at FacebookAbstract
We present the case of a 63-year-old woman with obscure gastrointestinal bleeding (OGIB) due to jejunal cavernous hemangioma diagnosed by video capsule endoscopy (VCE), contrast enhanced computed tomography (CECT) and CT angiography, who was successfully treated with surgical resection. Small bowel cavernous hemangioma is a rare cause of OGIB, most commonly presenting as an iron-deficiency anemia. Two decades ago, the preoperative diagnosis was quite difficult. Currently, the use of VCE and device assisted enteroscopy (DAE) allow detection of the lesion. Biopsy is not recommended due to the risks of uncontrolled bleeding. The use of CECT and CT angiography may be useful for demonstrate the vascular nature of the lesion, and define localization, number and extension of the lesion preoperatively in order to improve surgical results as was observed in our patient. Surgery is the most frequent treatment, notwithstanding, endoscopic resection of lesions has been recently reported. However, the experience is small and there are serious limitations of this technique.
Keywords
Cavernous hemangioma; Obscure gastrointestinal bleeding; Video capsule endoscopy; Contrast enhanced computed tomography; Angiography
Cavernous hemangioma articles, Obscure gastrointestinal bleeding articles, Video capsule endoscopy articles, Contrast enhanced computed tomography articles, Angiography articles
Cavernous hemangioma articles Cavernous hemangioma Research articles Cavernous hemangioma review articles Cavernous hemangioma PubMed articles Cavernous hemangioma PubMed Central articles Cavernous hemangioma 2023 articles Cavernous hemangioma 2024 articles Cavernous hemangioma Scopus articles Cavernous hemangioma impact factor journals Cavernous hemangioma Scopus journals Cavernous hemangioma PubMed journals Cavernous hemangioma medical journals Cavernous hemangioma free journals Cavernous hemangioma best journals Cavernous hemangioma top journals Cavernous hemangioma free medical journals Cavernous hemangioma famous journals Cavernous hemangioma Google Scholar indexed journals Obscure gastrointestinal bleeding articles Obscure gastrointestinal bleeding Research articles Obscure gastrointestinal bleeding review articles Obscure gastrointestinal bleeding PubMed articles Obscure gastrointestinal bleeding PubMed Central articles Obscure gastrointestinal bleeding 2023 articles Obscure gastrointestinal bleeding 2024 articles Obscure gastrointestinal bleeding Scopus articles Obscure gastrointestinal bleeding impact factor journals Obscure gastrointestinal bleeding Scopus journals Obscure gastrointestinal bleeding PubMed journals Obscure gastrointestinal bleeding medical journals Obscure gastrointestinal bleeding free journals Obscure gastrointestinal bleeding best journals Obscure gastrointestinal bleeding top journals Obscure gastrointestinal bleeding free medical journals Obscure gastrointestinal bleeding famous journals Obscure gastrointestinal bleeding Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals gastrointestinal bleeding articles gastrointestinal bleeding Research articles gastrointestinal bleeding review articles gastrointestinal bleeding PubMed articles gastrointestinal bleeding PubMed Central articles gastrointestinal bleeding 2023 articles gastrointestinal bleeding 2024 articles gastrointestinal bleeding Scopus articles gastrointestinal bleeding impact factor journals gastrointestinal bleeding Scopus journals gastrointestinal bleeding PubMed journals gastrointestinal bleeding medical journals gastrointestinal bleeding free journals gastrointestinal bleeding best journals gastrointestinal bleeding top journals gastrointestinal bleeding free medical journals gastrointestinal bleeding famous journals gastrointestinal bleeding Google Scholar indexed journals Video capsule endoscopy articles Video capsule endoscopy Research articles Video capsule endoscopy review articles Video capsule endoscopy PubMed articles Video capsule endoscopy PubMed Central articles Video capsule endoscopy 2023 articles Video capsule endoscopy 2024 articles Video capsule endoscopy Scopus articles Video capsule endoscopy impact factor journals Video capsule endoscopy Scopus journals Video capsule endoscopy PubMed journals Video capsule endoscopy medical journals Video capsule endoscopy free journals Video capsule endoscopy best journals Video capsule endoscopy top journals Video capsule endoscopy free medical journals Video capsule endoscopy famous journals Video capsule endoscopy Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals endoscopy articles endoscopy Research articles endoscopy review articles endoscopy PubMed articles endoscopy PubMed Central articles endoscopy 2023 articles endoscopy 2024 articles endoscopy Scopus articles endoscopy impact factor journals endoscopy Scopus journals endoscopy PubMed journals endoscopy medical journals endoscopy free journals endoscopy best journals endoscopy top journals endoscopy free medical journals endoscopy famous journals endoscopy Google Scholar indexed journals CT scan articles CT scan Research articles CT scan review articles CT scan PubMed articles CT scan PubMed Central articles CT scan 2023 articles CT scan 2024 articles CT scan Scopus articles CT scan impact factor journals CT scan Scopus journals CT scan PubMed journals CT scan medical journals CT scan free journals CT scan best journals CT scan top journals CT scan free medical journals CT scan famous journals CT scan Google Scholar indexed journals Angiography articles Angiography Research articles Angiography review articles Angiography PubMed articles Angiography PubMed Central articles Angiography 2023 articles Angiography 2024 articles Angiography Scopus articles Angiography impact factor journals Angiography Scopus journals Angiography PubMed journals Angiography medical journals Angiography free journals Angiography best journals Angiography top journals Angiography free medical journals Angiography famous journals Angiography Google Scholar indexed journals Contrast enhanced computed tomography articles Contrast enhanced computed tomography Research articles Contrast enhanced computed tomography review articles Contrast enhanced computed tomography PubMed articles Contrast enhanced computed tomography PubMed Central articles Contrast enhanced computed tomography 2023 articles Contrast enhanced computed tomography 2024 articles Contrast enhanced computed tomography Scopus articles Contrast enhanced computed tomography impact factor journals Contrast enhanced computed tomography Scopus journals Contrast enhanced computed tomography PubMed journals Contrast enhanced computed tomography medical journals Contrast enhanced computed tomography free journals Contrast enhanced computed tomography best journals Contrast enhanced computed tomography top journals Contrast enhanced computed tomography free medical journals Contrast enhanced computed tomography famous journals Contrast enhanced computed tomography Google Scholar indexed journals
Article Details
1. Introduction
Hemangioma accounts for only 0.5% of all gastrointestinal neoplasms. They represent 5-10% of all benign small bowel lesions [1]. They are more frequently placed in the jejunum presenting as a solitary or multiple lesion. The main symptoms include bleeding, abdominal pain, obstruction, intussusception, or rarely, perforation. Chronic iron-deficiency anemia is the most frequent manifestation although severe acute bleeding has been described [2-5]. Hemangioma originates in the submucosal vessels and may extend transmurally to the muscular layer or the serosa. [6] They are classified as cavernous, capillary or mixed types based on the diameter of the affected vessels [6]. The preoperative diagnosis was not possible for long time [7]. Currently, modern endoscopic methods such as video capsule endoscopy (VCE) and device-assisted enteroscopy (DAE) allow the detection of these lesions [8, 9]. VCE is considered as the first line procedure for assessing small bowel [10]. DAE can be used for hemostasis in cases of active bleeding. Besides, imaging procedures such as contrast enhanced computed tomography (CECT) and CT angiography can be useful for determining vascular nature and the number and location of lesions in order to determine the most appropriate therapy [11, 12].
We present here a patient with a cavernous hemangioma manifested as chronic iron-deficiency anemia, detected by VCE, CECT and CT angiography who was successfully treated with surgical resection.
2. Case Presentation
A 63-year-old woman was attended in our gastroenterology out-patient unit due to an eleven-year history of anemic syndrome. She was chronically treated with iron-oral supplementations. During the previous year, she had exacerbation of the anemic symptoms requiring several hospital admissions and showing decreased serum hemoglobin levels (5 to 6 g/dL) treated with blood transfusions. During this period, she underwent repeatedly esophagogastroduodenoscopy and colonoscopy without finding a source of bleeding.
At admission, she referred a 20-year history of diabetes mellitus and systemic arterial hypertension. She denied overt gastrointestinal bleeding or non-steroidal anti-inflammatory drugs (NSAID) chronic intake. Physical examination revealed only pale skin and conjunctivae. Laboratory tests revealed moderate anemia (serum hemoglobin of 8.2 g/dL, mean corpuscular volume 66.9 fL, mean concentration hemoglobin 19.1 pg), white blood cell count of 4,400 cells/µL, and a platelet count of 250,000/µL. Fecal occult blood test was positive.
An evaluation of her small bowel was decided through VCE which detected a solitary red polypoid lesion with eroded surface in the proximal jejunum without active bleeding (Figure 1).

Figure 1: Video capsule endoscopy image. Smooth rounded lesion with eroded surface (arrows) without active bleeding located in the jejunum.
A CECT was performed that demonstrated a unique contrast-enhancing lesion on jejunum. The angiography CT tridimensional reconstruction revealed an aberrant vessel originating from an arterial branch of the superior mesenteric artery which ended in a dilated vascular structure in the mucosa of jejunum. Active bleeding was not observed (Figure 2).
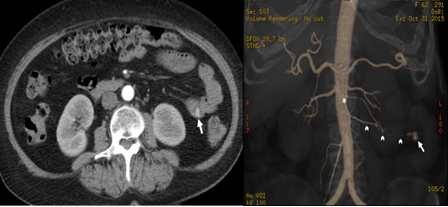
Figure 2: Abdominal contrast enhanced computed tomography and CT angiography images. (A) Hyper enhanced polypoid image on the proximal jejunum lumen (arrow) on arterial phase; (B) Vascular malformation (arrow) originating from an arterial branch (arrow heads) of the superior mesenteric artery (asterisk) by angiography computed tomography reconstruction.
With the diagnosis of a vascular lesion the patient was sent for surgical resection. An open laparotomy was performed during which no serosal vascular lesion or palpable nodule was detected. An intraoperative enteroscopy demonstrated a 22-mm diameter polypoid lesion with eroded mucosa surface at 50 cm from the Treitz ligament (Figure 3). A 20 cm-segmental resection of the proximal jejunum and end-to-end anastomosis was performed.
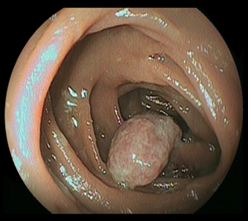
Figure 3: Intraoperative enteroscopy image. Reddish polypoid lesion with eroded mucosal surface detected in the proximal jejunum at 50 cm from the Treitz ligament.
Microscopic examination of the lesion showed vascular proliferation within the submucosa with large, dilated, blood-filled vessels lined by flattened endothelia and separated by connective tissue suggestive of cavernous hemangioma (Figure 4).
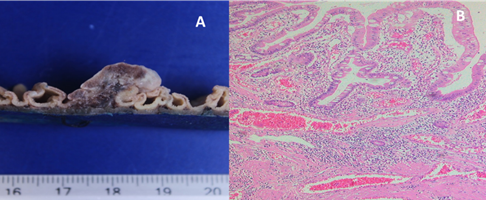
Figure 4: Pathologic features of the resected lesion. (A) Polipoid lesion involving submucosa with presence of a central vessel; (B) Microscopic examination showed proliferation of large dilated vascular channels within the submucosa separated by connective tissue stroma.
The patient had good postoperative evolution and was discharged from the hospital 7 days afterwards with normal hemoglobin serum levels. She has remained free of anemia after two years of follow-up since surgery.
3. Discussion
The cavernous is the most frequent histologic type of hemangioma. It is more frequently observed in males from 9 to 74 years and the size of the lesions may vary from 0.8 cm to 50 cm in diameter [13]. The preoperative diagnosis was rare before 2000. Currently, with the use of VCE and DAE the preoperative identification has significatively increased [7, 14]. They usually present as red or blueish raspberry-like sessile or polypoid lesions, however the endoscopic recognition may be difficult in some lesions which do not have the typical appearance, as was observed in our patient [9].
The determination of the vascular nature is important in order to define management. Biopsy is not recommended due to risks of severe bleeding. Therefore, the use of complementary imaging procedures may be useful [15]. In our patient we decided to perform a CECT and CT angiography in order to confirm the vascular nature of the polyp and to determine localization and number of lesions. CECT may reveal hemangioma as thickening of the small bowel with heterogenous and persistent enhancement of the lesion [14]. The distinctive CECT radiographic feature in hemangioma is strengthening of the lesion during the arterial phase as was observed in our case [11, 12]. On the other hand, CT angiography is a quick, imaging modality with excellent spatial and temporal resolution. Modern CT scanners can provide sub-millimeter isotropic three-dimensional datasets within a single breath-hold during the first past of intravenous contrast medium [15]. CT angiography has also a high diagnostic accuracy in detecting and localizing the source of gastrointestinal bleeding, with a sensitivity of approximately 85% [16], and it can detect bleeding rates of as little as 0.3 ml/min [17]. These imaging procedures are highly recommended particularly in patients in whom, a surgical approach is considered [14].
In only few of the published reported cases of small bowel hemangioma, CECT or CT angiography as complementary diagnostic procedures have been used [13, 18] We think that they should be used more frequently, particularly in patients in whom surgical treatment is considered. Surgical resection is the most frequent treatment, although endoscopic resection with snare polypectomy after submucosal saline solution injection has been recently described [18]. In a recent systematic review of 15 published cases of uncomplicated cavernous hemangioma diagnosed with VCE, DAE and CECT, from 2000 to 2018, 14 patients were treated surgically (with laparoscopy: 5 cases and laparotomy: 9 cases) and only 1 was treated endoscopically [13]. In this case report of a 19-year old patient, 4 sessile vascular lesions (0.8 to 14 mm in diameter), were successfully resected by snare polypectomy through DAE [19]. Although endoscopic treatment seems to be an attractive modality, there is still a very small experience in this technique. Besides, it may increase the risks of uncontrolled bleeding and gut perforation in transmural hemangiomas. In addition, large, numerous and widely disseminated lesions are beyond the scope of this technique [14, 18, 20]. In our case, we decided to perform small-bowel resection of the affected segment.
4. Conclusions
In conclusion, the cavernous hemangioma is a rare cause of small bowel bleeding. The use of VCE is a useful tool for detection of the lesion. The vascular nature of the lesion may be difficult in many cases. DAE has some limitations due to non-availability or the risks of bleeding due to biopsy. CETC and CT angiography can be considered as a complementary imaging study in order to confirm vascular nature and determine number and location of lesions especially when surgical approach is considered. More experience with endoscopic resection of lesions is necessary in order to define its precise role in the treatment of selected cases.
Author Contributions
R Monreal-Robles collected patient´s data; AN del Cueto-Aguilera, and OD Borjas-Almaguer performed the literature research; JA González-González, JO Jaquez-Quintana and HJ Maldonado-Garza critically reviewed the manuscript. D. García-Compean performed the capsule endoscopy procedure, wrote the manuscript and is the article guarantor. All authors red and approved the manuscript.
Supportive Foundations
None
Patient Informed Consent
Informed patient consent was obtained for publication of this case.
Conflict of Interest
The authors declare no conflicts of interest.
References
- Garvin PJ, Herrmann V, Kaminski DL, et al. Benign and malignant tumors of the small intestine. Curr Probl Cancer 3 (1979): 1-46.
- Kharrasse G, Hadjkacem H, Azouguagh R, et al. Intestinal hemangioma: an unusual cause of unexplained gastrointestinal bleeding, a case report. Pan Afr Med J 19 (2014): 64.
- Elias G, Toubia N. Hemangioma of the small intestine presenting with recurrent overt, obscure gastrointestinal bleeding. Clin Gastroenterol Hepatol 8 (2010): A18.e1.
- ElGendy K, Salem A. Multiple intestinal haemangiomas presenting as intussusception and bleeding. BMJ Case Rep (2014): bcr2014206365
- Rao AB, Pence J, Mirkin DL. Diffuse infantile hemangiomatosis of the ileum presenting with multiple perforations: a case report and review of the literature. J Pediatr Surg 45 (2010): 1890-1892.
- Camilleri M, Chadwick VS, Hodgson HJ. Vascular anomalies of the gastrointestinal tract. Hepatogastroenterology 31 (1984): 149-153.
- Akazawa Y, Hiramatsu K, Nosaka T et al. Preoperative diagnosis of cavernous hemangioma presenting with melena using wireless capsule endoscopy of the small intestine. Endosc Int Open 4 (2016): E249-E251.
- Alcalde Vargas A, Lopez T, Caballero J, et al. Intermittent gastrointestinal bleeding secondary to small bowel cavernous hemangioma diagnosed by wireless capsule endoscopy]. Med Clin (Barc) 140 (2013): 190-191.
- Khurana V, Dala R, Barkin JS. Small bowel cavernous hemangioma. Gastrointest Endosc 60 (2004): 96.
- Gerson LB, Fidler JL, Cave DR, et al. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol 110 (2015): 1265-1287.
- Huprich JE, Barlow JM, Hansel SL, et al. Multiphase CT enterography evaluation of small-bowel vascular lesions. AJR Am J Roentgenol 201 (2013): 65-72.
- Cui J, Huang LY, Lin SJ, et al. Small intestinal vascular malformation bleeding: a case report with imaging findings. World J Gastroenterol 20 (2014): 14076-14078.
- Durer C, Durer S, Sharbatji M, et al. Cavernous Hemangioma of the Small Bowel: A Case Report and Literature Review. Cureus 10 (2018): e3113.
- Takase N, Fukui K, Tani T, et al. Preoperative detection and localization of small bowel hemangioma: Two case reports. World J Gastroenterol 23 (2017): 3752-3757.
- Corsi A, Ingegnoli A, Abelli P, et al. Imaging of a Small Bowel Cavernous Hemangioma: Report of a Case with Emphasis on the Use of Computed Tomography and Enteroclysis Acta Biomed 78 (2007): 139-143.
- García-Blázquez V, Vicente-Bártulos A, Olavarria-Delgado A, et al. Accuracy of CT angiography in the diagnosis of acute gastrointestinal bleeding: systematic review and meta-analysis. Eur Radiol 23 (2013): 1181-1190.
- Kuhle WG, Sheiman RG. Detection of active colonic hemorrhage with use of helical CT: findings in a swine model. Radiology 228 (2003): 743-752.
- Hu PF, Chen H, Wang XH, et al. Small intestinal hemangioma: Endoscopic or surgical intervention? A case report and review of literature. World J Gastrointest Oncol 10 (2018): 516-521.
- Willert RP, Chong AK. Multiple cavernous hemangiomas with iron deficiency anemia successfully treated with double-balloon enteroscopy. Gastrointest Endosc 67 (2008): 765-767.
- Ruiz AR, Ginsberg AL. Giant mesenteric hemangioma with small intestinal involvement: an unusual cause of recurrent gastrointestinal bleed and review of gastrointestinal hemangiomas. Dig Dis Sci 44 (1999): 2545-2551.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
