Desmoplastic Fibroblastoma of the Maxillary Sinus
Article Information
Dubey Hitashi, Yong-Qian Liu, Zhao Xinxiang*
Department of Radiology, The Second Affiliated Hospital of Kunming Medical University, P.R China
*Corresponding Author: Dr. Xinxiang Zhao, Department of Radiology, The Second Affiliated Hospital of Kunming Medical University, 374,Dianmian Road, Wuhua District, Yunnan Province 650000, P.R.China
Received: 29 September 2021; Accepted: 12 October 2021; Published: 22 October 2021
Citation: Dubey Hitashi, Yong-Qian Liu, Zhao Xinxiang. Desmoplastic Fibroblastoma of the Maxillary Sinus. Archives of Clinical and Medical Case Reports 5 (2021): 733-740.
View / Download Pdf Share at FacebookAbstract
Desmoplastic fibroblastoma, also called collagenous fibroma, is an uncommon, firm, slow-growing, painless, benign fibrous soft tissue tumor [1] once in a while, including bone. Evans first described this tumor in 1995. The maxillary sinus is a very uncommon site for desmoplastic fibroblastoma. Men are two and a half times more likely than women to experience these neoplasms in their fifth or sixth decades of life. Subcutaneous tissue or near the deep aspect of the skin Muscles of the skeleton of the arm, for example, are common position shoulder, upper back, and posterior neck [3]. Desmoplastic fibroblastoma in the Maxillary sinus is a very rare location to have in the third decade of life by location and age. Here we intend to present a case report of this particular case.
Keywords
Maxillary sinus; Magnetic resonance imaging; Computed tomography; Desmoplastic fibroblastoma; Collagenous fibroma; Soft tissue tumors
Maxillary sinus articles; Magnetic resonance imaging articles; Computed tomography articles; Desmoplastic fibroblastoma articles; Collagenous fibroma articles; Soft tissue tumors articles
Maxillary sinus articles Maxillary sinus Research articles Maxillary sinus review articles Maxillary sinus PubMed articles Maxillary sinus PubMed Central articles Maxillary sinus 2023 articles Maxillary sinus 2024 articles Maxillary sinus Scopus articles Maxillary sinus impact factor journals Maxillary sinus Scopus journals Maxillary sinus PubMed journals Maxillary sinus medical journals Maxillary sinus free journals Maxillary sinus best journals Maxillary sinus top journals Maxillary sinus free medical journals Maxillary sinus famous journals Maxillary sinus Google Scholar indexed journals Magnetic resonance imaging articles Magnetic resonance imaging Research articles Magnetic resonance imaging review articles Magnetic resonance imaging PubMed articles Magnetic resonance imaging PubMed Central articles Magnetic resonance imaging 2023 articles Magnetic resonance imaging 2024 articles Magnetic resonance imaging Scopus articles Magnetic resonance imaging impact factor journals Magnetic resonance imaging Scopus journals Magnetic resonance imaging PubMed journals Magnetic resonance imaging medical journals Magnetic resonance imaging free journals Magnetic resonance imaging best journals Magnetic resonance imaging top journals Magnetic resonance imaging free medical journals Magnetic resonance imaging famous journals Magnetic resonance imaging Google Scholar indexed journals Computed tomography articles Computed tomography Research articles Computed tomography review articles Computed tomography PubMed articles Computed tomography PubMed Central articles Computed tomography 2023 articles Computed tomography 2024 articles Computed tomography Scopus articles Computed tomography impact factor journals Computed tomography Scopus journals Computed tomography PubMed journals Computed tomography medical journals Computed tomography free journals Computed tomography best journals Computed tomography top journals Computed tomography free medical journals Computed tomography famous journals Computed tomography Google Scholar indexed journals Desmoplastic fibroblastoma articles Desmoplastic fibroblastoma Research articles Desmoplastic fibroblastoma review articles Desmoplastic fibroblastoma PubMed articles Desmoplastic fibroblastoma PubMed Central articles Desmoplastic fibroblastoma 2023 articles Desmoplastic fibroblastoma 2024 articles Desmoplastic fibroblastoma Scopus articles Desmoplastic fibroblastoma impact factor journals Desmoplastic fibroblastoma Scopus journals Desmoplastic fibroblastoma PubMed journals Desmoplastic fibroblastoma medical journals Desmoplastic fibroblastoma free journals Desmoplastic fibroblastoma best journals Desmoplastic fibroblastoma top journals Desmoplastic fibroblastoma free medical journals Desmoplastic fibroblastoma famous journals Desmoplastic fibroblastoma Google Scholar indexed journals fibroblastoma articles fibroblastoma Research articles fibroblastoma review articles fibroblastoma PubMed articles fibroblastoma PubMed Central articles fibroblastoma 2023 articles fibroblastoma 2024 articles fibroblastoma Scopus articles fibroblastoma impact factor journals fibroblastoma Scopus journals fibroblastoma PubMed journals fibroblastoma medical journals fibroblastoma free journals fibroblastoma best journals fibroblastoma top journals fibroblastoma free medical journals fibroblastoma famous journals fibroblastoma Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Collagenous fibroma articles Collagenous fibroma Research articles Collagenous fibroma review articles Collagenous fibroma PubMed articles Collagenous fibroma PubMed Central articles Collagenous fibroma 2023 articles Collagenous fibroma 2024 articles Collagenous fibroma Scopus articles Collagenous fibroma impact factor journals Collagenous fibroma Scopus journals Collagenous fibroma PubMed journals Collagenous fibroma medical journals Collagenous fibroma free journals Collagenous fibroma best journals Collagenous fibroma top journals Collagenous fibroma free medical journals Collagenous fibroma famous journals Collagenous fibroma Google Scholar indexed journals Radioembolization articles Radioembolization Research articles Radioembolization review articles Radioembolization PubMed articles Radioembolization PubMed Central articles Radioembolization 2023 articles Radioembolization 2024 articles Radioembolization Scopus articles Radioembolization impact factor journals Radioembolization Scopus journals Radioembolization PubMed journals Radioembolization medical journals Radioembolization free journals Radioembolization best journals Radioembolization top journals Radioembolization free medical journals Radioembolization famous journals Radioembolization Google Scholar indexed journals Soft tissue tumors articles Soft tissue tumors Research articles Soft tissue tumors review articles Soft tissue tumors PubMed articles Soft tissue tumors PubMed Central articles Soft tissue tumors 2023 articles Soft tissue tumors 2024 articles Soft tissue tumors Scopus articles Soft tissue tumors impact factor journals Soft tissue tumors Scopus journals Soft tissue tumors PubMed journals Soft tissue tumors medical journals Soft tissue tumors free journals Soft tissue tumors best journals Soft tissue tumors top journals Soft tissue tumors free medical journals Soft tissue tumors famous journals Soft tissue tumors Google Scholar indexed journals
Article Details
1. Introduction
Collagenous fibroma (desmoplastic fibroblastoma) is a unique fibrous soft tissue tumor that comprises spindle-shaped to stellate fibroblastic cells sparsely distributed in a dense fibrous background. Previously depicted by Evans in 1995 [1]. From that point forward, the sore's most significant arrangement, with 63 cases, was distributed by Miettinen and Fetsch [2] in 1998. This tumor is characterized by spindle-shaped to stellate fibroblastic cells. Clinically, desmoplastic fibroblastoma presents as a firm mobile, painless mass, which develops gradually and is situated inside the subcutaneous tissues or skeletal muscle. Surgery is the treatment of choice. Neither nearby repeat nor metastases have been accounted for after resection [4]. It ordinarily happens in the fifth to seventh decade of life, with a significant male transcendence [2]. It has a wide anatomical distribution; nonetheless, the arms, shoulders, neck, hands, and feet are generally continuous destinations [2, 3]. It is usually situated in the subcutaneous tissue and skeletal muscle [2]. Uncommon areas for desmoplastic fibroblastoma includes the joint, oral cavity, dermis, lower abdomen, the parotid and lacrimal glands [4-10]. To the best of our knowledge, no radiologic reports of desmoplastic fibroblastoma mimicking maxillary sinus have been found.
Herein, we report an unusual case of a desmoplastic fibroblastoma of the maxillary sinus in a 28-year-old male patient, including magnetic resonance imaging MRI and computed tomography CT combined with pathological findings of the maxillary sinus.
2. Case Report
2.1 Clinical history
The patient, a 28-year-old male, was admitted to the hospital due to "left facial discomfort for six days." The patient complained of facial discomfort after tooth extraction five days ago, with secretions flowing from the tooth's root, no pain, such as nose and pus, and occasionally first-class discomfort. He went to Zhaotong hospital of traditional Chinese medicine and underwent a CT examination of accessory nasal solid. It was found that there was a solid lesion on the left side, which was recommended to the higher hospital for further treatment. The patient came to our hospital for further treatment and was admitted with an "upper lesion on the left side." The diet was ok; expected the urine and stool; the weight was not reduced; the history of hypertension and heart disease was denied. The history of the urinary disease, vascular disease, and mental disease was also denied.
Physical examination T: 36.7 C, P: 8/min, R: 19 times/min, P: 136, bilateral ears symmetrical, no deformity, no injury, no redness, swelling and seeding, external auditory canal unobstructed, no atresia, cleanness, no redness, no swelling, no drum, no hole, no blood clotting, light cone, signs, bilateral mastoid without redness, swelling and pressure cancer, no deformity of the external nose, no skin laceration, no redness and swelling of anterior skin, no hair falling off, irregular deviation of the nasal septum, hematoma, slightly hyperemia of cavity, bilateral inferior nail hypertrophy, chronic hyperemia, bilateral middle nasal meatus and fissure was seen, In the bilateral nose a little sticky substance was seen.
The bilateral atrial area was without pressure; pharynx was hanging in the middle, partial mucosa hyperemia, retropharyngeal few lymph vesicle hyperplasias were found. Bilateral tonsils were 1 degree large. It had a smooth surface without hyperemia; no pyogenic column was there. The larynx had bilateral pear-shaped symmetry, no effusion, and new organisms were found. Larynx epiglottis- was without curvature, sticky, smooth, bloodless, bilateral without swelling and organisms, bilateral activity was seen good, glottis seemed closed well, the left upper tooth was missing, and the surface was seen new and red.
An auxiliary examination from a previous hospital visit from a different hospital showed bone changes on the maxillary sinus's left upper and peripheral images, arterial-like bone cysts, right superior inflammation, septal deviation, and bilateral inferior nail hypertrophy there.
2.2 Radiological findings
In contrast-enhanced scan injected Iohexol 350, 100 ml, injection speed 5ml intravenously. The alveolar definite mixed low-density shadow of the left maxillary molar showed no noticeable enhancement; the size was about 4.2*3.4*5.6 cm. There were multiple broken rings and absorption of the adjacent bone, no definite sclerotic edge, the precise boundary of the lesion, symmetrical structure of the rest nasopharynx, tissue interface was distinct. There was no stenosis and displacement of pharyngeal fossa and parapharyngeal space. No abnormality of bilateral carotid sheath area and no abnormality of the corresponding intracranial structure was seen. The bony window showed no destruction of the skull base. The nasal septum was seen slightly to the right. The double inferior turbinate was hypertrophic, and the local nasal mucosa was somewhat thickened. In the other groups, the accessory nose was developed usually, gasified well, and found no abnormal density shadow in the cavity; no abnormality was found in the other paranasal sinuses.
- an alveolar space- occupying lesion of the left upper molar, alveolar swelling was considered.
- septum partial right deviation, double inferior turbinate hypertrophy, rhinitis was there.
- the rest of the pharynx, paranasal sinuses plain scan, no apparent abnormalities were found.
2.3 Histopathological findings
Pathological report of the left maxillary mass biopsy, Production content was the wax block, one slice: 5 pieces of immunohistochemistry: 7. In items of special staining: 1 object from the naked eye has been observed. Found a pile of grayish- white and grayish red soft tissue, 1*1*0.2 cm in size, buried in the box. The pathological findings were as follows: (left maxillary sinus tumor) part of the fibrous tissue for proliferation and necrotic tissue; no malignant lesions were found. Immunohistochemical results showed that wax block 1ck wide (-), CK low (EA (-) 167 (3%) P40 (-), CK 5/6 (Ca (scattered +) particular staining results was one wax block with silver staining (+) positive.
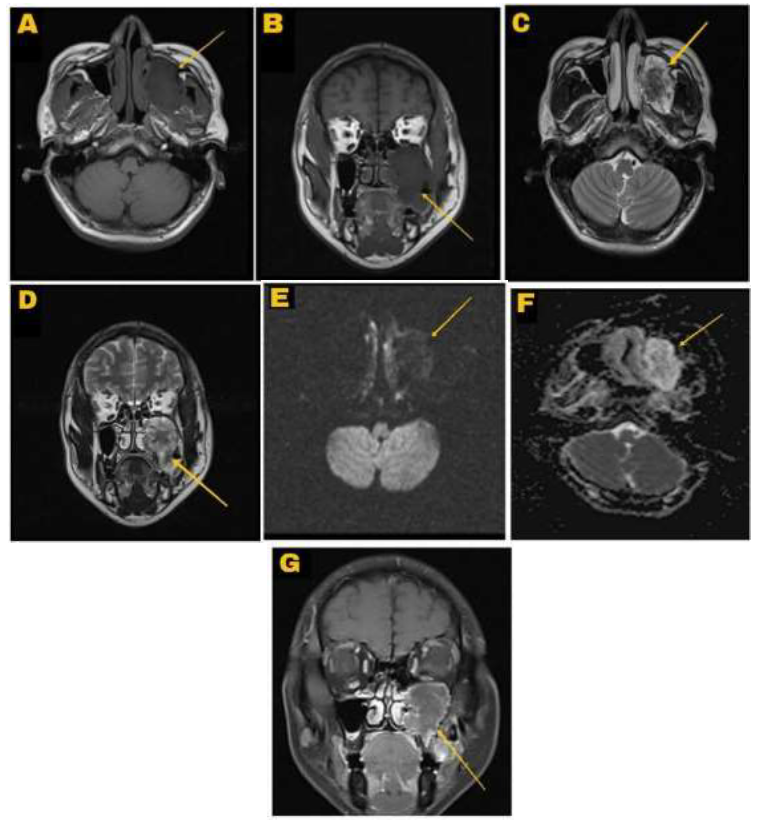
Figure 1: A. T1 Axial image showed that lesion was hypointense compare to surrounding solitary nodule involving left maxillary sinus with size about 4.2*3.4*5.6 cm with no definite sclerotic edge and septum deviated partially to the right. B. T1 coronal image showed the lesion was hypointense C. T2 Axial image showed the lesion was not evenly hyperintense in the periphery and hypointense in the middle and towards median aspect D. T2 Coronal image showed the lesion was hypointense in the middle and slightly hyperintense in periphery E. DWI Diffusion-weighted image showed hypointense in the middle & hyperintense towards periphery signal F. ADC apparent diffusion coefficient image showed hyperintense lesion which was slightly hypointense in the middle G. Post-contrast coronal view showed hyperintense lesion which was slightly hypointense in the middle in the left maxillary sinus.
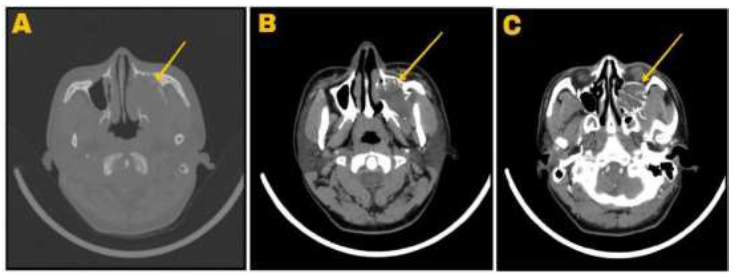
Figure 2: A. CT Bone window showed a lesion in the left maxillary sinus with partial right septal deviation with no definite sclerotic edge B. CT Soft tissue window showed a lesion in the left maxillary sinus with double inferior turbinate was hypertrophic, and the local nasal mucosa was slightly thickened with no abnormal density shadow in the sinus C. CT enhanced view showing uneven hypo and hyperdense lesion in the left maxillary sinus.
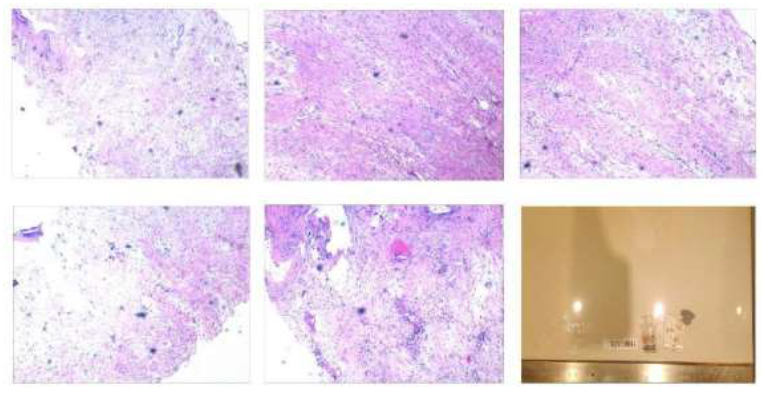
Figure 3: Showing histopathological features (hematoxylin and eosin stain). (H and E, ×200) photomicrograph of the tumor demonstrating fibrous and myxocollagenous areas. The tumor border is well defined. The fibrous site shows wavy and dense collagen fibers. The tumor cells are spindle-shaped and stellate, with poor cellularity—Photomicrograph of a myxocollagenous stroma, revealing benign-appearing spindle cells with higher cellularity than the fibrous region. Desmoplastic fibroblastoma lesion left maxillary sinus. A high-power photomicrograph (shows spindled (thin arrows) and stellate (thick arrows) fibroblasts that are characteristic of desmoplastic fibroblastoma within a loose myxoid stroma (hematoxylin and eosin without any atypia within a dense collagenous background. After surgery, the stellate-shaped tumor cells had eosinophilic cytoplasm, prominent basophilic nucleoli (H&E staining, ×40), and tumors.
3. Discussion
Desmoplastic fibroblastoma is a distinctive form of benign fibrous soft-tissue tumor described for the first time by Evans. Several articles reported this entity, with Miettinen and Fetsch publishing the most extensive 63 cases [2]. It is most commonly seen in the subcutaneous tissue and skeletal muscle. Men are two and a half times more likely than women to develop these neoplasms in their fifth or sixth decades of life. Excision of the lesion is curative, and there has been no evidence of aggressive development (12).
Desmoplastic fibroblastoma manifests itself clinically as a well-circumscribed, painless, firm, round or oval, movable, slowly developing mass. The diameters ranged from 1 to 20 centimeters. It is frequently present in subcutaneous tissue or the deep aspect of skeletal muscles. The arm, shoulder, posterior neck, and upper back are all common places [1-8]. Tumors growing in the thigh have been described in a few prior instances [1, 2, 6, 8]. The tumor in our current patient seems to have originated in the maxillary sinus. The left superior sinus occupied the space, the lesion grew downward, involved the left superior alveolar, locally protruded into the left ethmoid sinus. The lesion was well-circumscribed, the diameter was under the range.
Under the microscope, the bland spindle or stellate-shaped fibroblasts are dispersed in the dense and abundant collagenous matrix [15]. In the presented case, the dispersed spindle-shaped & stellate tumor cells present inside a dense myxoid stroma matrix and benign-appearing spindle cells presenting higher cellularity than in the fibrous area, which is characteristic of desmoplastic fibroblastoma. You can easily appreciate this from histopathological findings in the presenting picture.
Desmoplastic fibroblastoma radiological features, as described by vandevanne [16]. Desmoid tumors with a high SI appear to expand in size on T2- weighted imaging. As a result, they show an increase in low SI areas on T2- weighted imaging. Finally, they obtain a low overall SI. On T1- & T2-weighted pictures, as well as a decrease in the scale. The majority of soft tissue tumors were found to have a high signal intensity on T2 weighted images and T1 weighted images with low SI, as presented here in our patient.
In radiological findings of our case, there was a mass of slightly long T1 mixed T2 signal shadow in the left maxillary sinus with clear boundary, about 4.2*3.4*5.6 cm in size. The bone of the sinus wall was destroyed, the lesion grew downward, involved the left upper alveolar, and locally protruded into the left ethmoid. The lower part of the lesion revealed notable uneven enhancement on the contrast-enhanced imaging. The rest showed edge enhancement and pushed the surrounding pterygoid and masseter muscles. The morphological signals of the right superior sinus, frontal sinus right ethmoid sinus were normal. On MRI, T1-weighted images of the mass represented a mixture of low-intensity SI and ISO. With T2 weighting, the mass showed scattered areas of high IS within an area of low IS. Contrast-weighted T1 images demonstrated inhomogeneous enhancement after contrast administration and the unenhanced regions corresponding to the low-IS areas on T1-weighted images without contrast.
In some instances, bone desmoid-type fibromatosis treatment includes marginal or wide resection with or without replacement by allograft or amputation. However, complete surgical excision is recommended for desmoplastic fibroblastoma due to the benign nature of this neoplasm. There have been no reports of tumor recurrence during follow-up, including the current case, when surgical resection was undertaken. Strong mass without calcification is the most common radiological finding in desmoplastic fibroblastoma. On rare occasions, a highly calcified mass or the presence of diffused dystrophic calcification has been discovered [13, 14]. Desmoplastic fibroblastomas have inhomogeneously low to moderate signal intensity on T1-weighted pictures, low to slightly higher signal intensity on T2-weighted images, and contrast-enhanced images. Low to moderate or heterogeneous enhancement with areas of no enhancement can be seen in T1-weighted images [8, 11, 13, 14].
Desmoplastic fibroblastoma of the maxillary sinus tumor is an uncommon type of desmoplastic fibroblastoma. Also, it's not common in the thirty's age group. Clinically, MRI imaging with and without contrast and CT along with histopathological findings make it helpful to diagnose.
Confidentiality Statement
We have de-identified all data to ensure patient confidentiality.
Consent
The patient's written informed consent for print, and the authors acquired electronic publication of this case report.
Declaration of Conflicting Interest
The authors declared no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics
The hospital's ethical committee has approved this case report.
References
- Evans HL. Desmoplastic fibroblastoma. A report of seven cases. Am J Surg Pathol 19 (1995): 1077-1081.
- Nielsen GP, O'Connell JX, Dickersin GR, et al. Collagenous fibroma (desmoplastic fibroblastoma): a report of seven cases. Mod Pathol 9 (1996): 781-785.
- Kamata Y, Anazawa U, Morioka H, et al. Natural evolution of desmoplastic fibroblastoma on magnetic resonance imaging: a case report. J Med Case Rep 5 (2011): 139.
- Jaafari-Ashkavandi Z, Shirazi MY, Assar S. Desmoplastic Fibroblastoma in Maxillary Alveolar Bone Mimicking An Odontogenic Lesion: A Novel Case Report with Review of Literature. Turk Patoloji Derg 34 (2018): 247-250.
- Lee SM, Ha DH, Kang SH, et al. Desmoplastic fibroblastoma mimicking tenosynovial giant cell tumor encasing a tendon of the foot. Skeletal Radiol 48 (2019): 637-641.
- Yue Y, Liu Y, Song L, et al. MRI findings of low-grade fibromyxoid sarcoma: a case report and literature review. BMC Musculoskelet Disord 19 (2018):65.
- Urigo C, Schenkel MC, Assal M, et al. Calcified desmoplastic fibroblastoma of the foot: imaging findings. Skeletal Radiol 46 (2017): 565-569.
- Bonardi M, Zaffarana VG, Precerutti M. US and MRI appearance of a collagenous fibroma (desmoplastic fibroblastoma) of the shoulder. J Ultrasound 17 (2013): 53-56.
- Ge Y, Guo G, You Y, et al. Magnetic resonance imaging features of fibromas and giant cell tumors of the tendon sheath: differential diagnosis. Eur Radiol 29 (2019): 3441-3449.
- Kresse ME, Kransdorf MJ, Fox MG, et al. Desmoplastic Fibroblastoma: An Uncommon Tumor With a Relatively Characteristic MRI Appearance. AJR Am J Roentgenol 215 (2020): 178-183.
- Bonardi M, Zaffarana VG, Precerutti M. US and MRI appearance of a collagenous fibroma (desmoplastic fibroblastoma) of the shoulder. J Ultrasound 17 (2013): 53-56.
- Ogose A, Hotta T, Emura I, et al. Collagenous fibroma of the arm: a report of two cases. Skeletal Radiol 29 (2000): 417-420.
- Shuto R, Kiyosue H, Hori Y, et al. CT and MR imaging of desmoplastic fibroblastoma. Eur Radiol 12 (2002): 2474-2476.
- Yamamoto A, Abe S, Imamura T, et al. Three cases of collagenous fibroma with rim enhancement on postcontrast T1-weighted images with fat suppression. Skeletal Radiol 42 (2013): 141-146.
- Gong LH, Liu WF, Ding Y, et al. Diagnosis and Differential Diagnosis of Desmoplastic Fibroblastoma by Clinical, Radiological, and Histopathological Analyses. Chin Med J (Engl) 131 (2018): 32-36.
- Vandevenne JE, De Schepper AM, De Beuckeleer L, et al. New concepts in understanding evolution of desmoid tumors: MR imaging of 30 lesions. Eur Radiol 7 (1997): 1013-1019.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
