Development of Renal Cell Carcinoma in A Young Patient with Ileocecal Crohn’s Disease Under Treatment with Infliximab: Case Report and Review of the Literature
Article Information
John K. Triantafillidis1,2*, Eleni Triantafyllidi2, Apostolos Ε. Papalois3,4
1Inflammatory Bowel Disease Unit, “Metropolitan General” Hospital, Holargos, Athens, Greece. 264 Mesogeion Avenue, Cholargos, 15562, Athens, Greece
2Hellenic Society of Gastrointestinal Oncology, Iera odos 354, 12461, Haidari, Greece
3Experimental, Educational and Research Center ELPEN, Pikermi Athens, Greece. 95 Marathonos Av, Pikermi, 19009, Attica, Athens, Greece
4European University Cyprus, School of Medicine, Diogenous St, 2404 Engomi, PO Box 22006, Nicosia, 1516, Cyprus
*Corresponding Author: Dr. John K. Triantafillidis, Hellenic Society of Gastrointestinal Oncology, Iera odos 354, 12461, Haidari, Greece
Received: 10 January 2020; Accepted: 20 January 2020; Published: 03 February 2020
Citation: John K. Triantafillidis, Eleni Triantafyllidi, Apostolos Ε. Papalois. Development of Renal Cell Carcinoma in A Young Patient with Ileocecal Crohn’s Disease Under Treatment with Infliximab: Case Report and Review of the Literature. Archives of Clinical and Medical Case Reports 4 (2020): 153-157.
View / Download Pdf Share at FacebookAbstract
We describe a rare case of a young patient with Crohn’s disease, who accidentally was found to have developed renal cell carcinoma while on treatment with anti-TNF-α biologic agent. The patient was submitted to laparoscopic resection of the tumor. Up to December 2019 he is in perfect condition without receiving any kind of antineoplastic treatment. Clinicians should bear in mind this clinical combination in patients with Crohn’s disease under treatment with biologic anti-TNF-α agents. Because the exact influence of anti-TNF-α biologic agents is largely unclear for now, the continuation of treatment might be a possible option.
Keywords
Inflammatory bowel disease; Crohn’s disease; Renal carcinoma; Biologic agents; Infliximab
Inflammatory bowel disease articles, Crohns disease articles, Renal carcinoma articles, Biologic agents articles, Infliximab articles
Inflammatory bowel disease articles Inflammatory bowel disease Research articles Inflammatory bowel disease review articles Inflammatory bowel disease PubMed articles Inflammatory bowel disease PubMed Central articles Inflammatory bowel disease 2023 articles Inflammatory bowel disease 2024 articles Inflammatory bowel disease Scopus articles Inflammatory bowel disease impact factor journals Inflammatory bowel disease Scopus journals Inflammatory bowel disease PubMed journals Inflammatory bowel disease medical journals Inflammatory bowel disease free journals Inflammatory bowel disease best journals Inflammatory bowel disease top journals Inflammatory bowel disease free medical journals Inflammatory bowel disease famous journals Inflammatory bowel disease Google Scholar indexed journals disease articles disease Research articles disease review articles disease PubMed articles disease PubMed Central articles disease 2023 articles disease 2024 articles disease Scopus articles disease impact factor journals disease Scopus journals disease PubMed journals disease medical journals disease free journals disease best journals disease top journals disease free medical journals disease famous journals disease Google Scholar indexed journals Crohn’s disease articles Crohn’s disease Research articles Crohn’s disease review articles Crohn’s disease PubMed articles Crohn’s disease PubMed Central articles Crohn’s disease 2023 articles Crohn’s disease 2024 articles Crohn’s disease Scopus articles Crohn’s disease impact factor journals Crohn’s disease Scopus journals Crohn’s disease PubMed journals Crohn’s disease medical journals Crohn’s disease free journals Crohn’s disease best journals Crohn’s disease top journals Crohn’s disease free medical journals Crohn’s disease famous journals Crohn’s disease Google Scholar indexed journals Renal carcinoma articles Renal carcinoma Research articles Renal carcinoma review articles Renal carcinoma PubMed articles Renal carcinoma PubMed Central articles Renal carcinoma 2023 articles Renal carcinoma 2024 articles Renal carcinoma Scopus articles Renal carcinoma impact factor journals Renal carcinoma Scopus journals Renal carcinoma PubMed journals Renal carcinoma medical journals Renal carcinoma free journals Renal carcinoma best journals Renal carcinoma top journals Renal carcinoma free medical journals Renal carcinoma famous journals Renal carcinoma Google Scholar indexed journals carcinoma articles carcinoma Research articles carcinoma review articles carcinoma PubMed articles carcinoma PubMed Central articles carcinoma 2023 articles carcinoma 2024 articles carcinoma Scopus articles carcinoma impact factor journals carcinoma Scopus journals carcinoma PubMed journals carcinoma medical journals carcinoma free journals carcinoma best journals carcinoma top journals carcinoma free medical journals carcinoma famous journals carcinoma Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals Biologic agents articles Biologic agents Research articles Biologic agents review articles Biologic agents PubMed articles Biologic agents PubMed Central articles Biologic agents 2023 articles Biologic agents 2024 articles Biologic agents Scopus articles Biologic agents impact factor journals Biologic agents Scopus journals Biologic agents PubMed journals Biologic agents medical journals Biologic agents free journals Biologic agents best journals Biologic agents top journals Biologic agents free medical journals Biologic agents famous journals Biologic agents Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals Infliximab articles Infliximab Research articles Infliximab review articles Infliximab PubMed articles Infliximab PubMed Central articles Infliximab 2023 articles Infliximab 2024 articles Infliximab Scopus articles Infliximab impact factor journals Infliximab Scopus journals Infliximab PubMed journals Infliximab medical journals Infliximab free journals Infliximab best journals Infliximab top journals Infliximab free medical journals Infliximab famous journals Infliximab Google Scholar indexed journals Respiratory dysfunction articles Respiratory dysfunction Research articles Respiratory dysfunction review articles Respiratory dysfunction PubMed articles Respiratory dysfunction PubMed Central articles Respiratory dysfunction 2023 articles Respiratory dysfunction 2024 articles Respiratory dysfunction Scopus articles Respiratory dysfunction impact factor journals Respiratory dysfunction Scopus journals Respiratory dysfunction PubMed journals Respiratory dysfunction medical journals Respiratory dysfunction free journals Respiratory dysfunction best journals Respiratory dysfunction top journals Respiratory dysfunction free medical journals Respiratory dysfunction famous journals Respiratory dysfunction Google Scholar indexed journals
Article Details
1. Introduction
Although descriptions of the appearance of renal cell carcinoma (RCC) on the ground of ulcerative colitis have been previously described [1,2,3], descriptions of RCC developed on the course of Crohn’s disease (CD) are scarce [4]. Patients with CD are at increased risk for both intestinal and extra-intestinal malignancies [5] and this risk is mainly attributed to chronic inflammation and immunosuppression [6, 7]. We describe here a young patient with CD who accidentally was found to have developed RCC during his treatment with anti-TNF-α biologic agent. The patient was submitted to laparoscopic resection of the RCC. Up to December 2019 he is in perfect condition without receiving any kind of antineoplastic treatment.
2. Case Report
A male patient, aged 35, was suffering from stenotic ileocecal CD, since the age of 23. During the last 4 years he was under treatment with anti-TNF-α agent (infliximab) with initially satisfactory clinical results. However, during the last two years it became necessary to shorten the intervals of the administration of infliximab due to gradual loss of response. In May 2018 he was finally switched on to ustekinumab because of the appearance of a severe allergic reaction to infliximab. At that time, abdominal imaging techniques (computed tomography and magnetic resonance imaging) performed on the basis of his regular follow-up, revealed the presence of an almost 3 cm-diameter tumor in the right kidney with imaging characters compatible with RCC (Figures 1-3]. After a thorough discussion with the patient and his relatives, a laparoscopic excision of the tumor was finally performed. The histological picture of the 5 × 4 × 1cm surgical specimen was compatible with RCC. A grade III malignancy stage according to Fuhrman classification was described. In some areas the tumor was reaching the renal capsule, however without infiltrating it. Surgical margins were free of tumor invasion. After the complete excision of the tumor no further treatment was applied. At present (December 2019), the patient is in a satisfactory clinical situation under treatment with ustekinumab.

Figure 1: Abdominal MRI showing inflammatory ileal involvement, as well as a renal mass of 3cm diameter, occupying the upper part of the right kidney.

Figure 2: Computed Tomography of the abdomen showing extensive terminal ileum involvement from Crohn’s disease along with an inflamed mass connecting the two involved parts of the bowel.
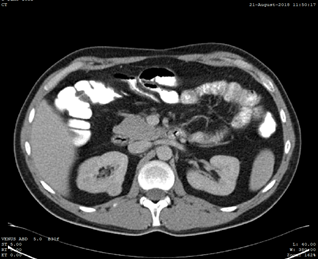
Figure 3: Computed tomography of the abdomen showing a renal mass of 3 cm diameter, occupying the upper part of the right kidney.
3. Discussion
Patients with CD seem to be at a relatively increased risk for development of RCC. In a population-based study in Chinese patients with IBD So et al, found that patients with CD had a higher risk of RCC (SIR 6.89; 95% CI, 2.22-21.37), compared with the general population [8]. Similarly, Wauters et al. [9] in a retrospective study including both, patients with IBD and RCC and patients with rheumatoid arthritis and RCC, found seven patients with renal cell carcinoma who were exposed to anti-TNF-a treatment. Compared to the group of patients with RCC without exposure to anti-TNF-a agent treatment, they were younger at age of diagnosis and they had received immunosuppressives more frequently. However the standardized incidence ratios for IBD-RCC were not increased after anti-TNF exposure. Derikh et al found that pancolitis, penetrating CD, IBD related surgery, male gender, and older age at IBD onset were independent risk factors for RCC development. Also IBD patients had lower N-stage, lower M-stage, and underwent more frequently surgical treatment for RCC compared to the general population, thus having better survival rate [5].
It is of interest that most of the relevant studies suggest that immunosuppressive and anti-TNFα therapy does not adversely affect disease free and overall survival in IBD patients following RCC diagnosis, meaning that treatment with biologic agents might be started or continued after RCC diagnosis in patients with low stage RCC [9]. The explanation could probably related to the fact that TNF-α can act as an autocrine tumor growth factor and that its presence is usually associated with poor prognosis. So despite concerns regarding a possible carcinogenic effect of treatment with anti-TNF-a factors, these agents have been previously considered as a therapeutic strategy for RCC, although other studies did not describe beneficial effect of anti-TNFα therapy in metastatic RCC [10].
Concerning IBD patients with malignant disease in their past history we suggest that they should be managed jointly with the oncologist. Moreover, some factors including location, histology, and prognosis of the tumor, as well time from diagnosis and severity of the underlying inflammatory disorder, should be taken into account concerning the decision of restarting treatment with anti-TNF agent or not. However, mesalazine, corticosteroids, antibiotics, enteral and parenteral nutrition and surgery should freely continue [11].
In conclusion, RCC may develop in patients with IBD treated with biologic anti-TNF-α agents. The diagnosis of RCC is usually incidental on routine abdominal imaging especially in young patients with IBD. Because the exact influence of anti-TNF-α biologic agents is largely unclear for now, the continuation of treatment might be a possible option.
References
- Satsangi J, Marshall J, Roskell D, Jewell D. Ulcerative colitis complicated by renal cell carcinoma: a series of three patients. Gut 38 (1996): 148-150.
- Plaisier PW. Ulcerative colitis and renal cell carcinoma. Gut 38 (1996): 936.
- Casellas F, Sardi J, Malagelada JR. Renal cell carcinoma and ulcerative colitis. Rev Esp Enferm Dig 94 (2002): 107-108.
- Pedersen N, Duricova D, Elkjaer M, et al. Risk of extra-intestinal cancer in inflammatory bowel disease: meta-analysis of population-based cohort studies. Am J Gastroenterol 105 (2010): 1480-1487.
- Derikx LA, Nissen LH, Drenth JP, et al. Dutch Initiative on Crohn and Colitis; PALGA Group; IBD/RCC Group. Better survival of renal cell carcinoma in patients with inflammatory bowel disease. Oncotarget 6 (2015): 38336-38347.
- Axelrad JE, Lichtiger S, Yajnik V. Inflammatory bowel disease and cancer: The role of inflammation, immunosuppression, and cancer treatment. World J Gastroenterol 22 (2016): 4794-4801.
- Beaugerie L, Carrat F, Colombel JF, et al. Peyrin-Biroulet L for the CSG. Risk of new or recurrent cancer under immunosuppressive therapy in patients with IBD and previous cancer. Gut 63 (2014): 1416-1423.
- So J, Tang W, Leung WK, et al. Cancer risk in 2621 Chinese patients with Inflammatory Bowel Disease: A population-based cohort study. Inflamm Bowel Dis 23 (2017): 2061-2068.
- Wauters L, Billiet T, Papamichael K, et al. Incidence of renal cell carcinoma in inflammatory bowel disease patients with and without anti-TNF treatment. Eur J Gastroenterol Hepatol 29 (2017): 84-90.
- Larkin JM, Ferguson TR, Pickering LM, et al. A phase I/II trial of sorafenib and infliximab in advanced renal cell carcinoma. British J Cancer 103 (2010): 1149-1153.
- Cosnes J. What should be done in inflammatory bowel disease patients with prior malignancy? Dig Dis 35 (2017): 50-55.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
