Effect of Perceived Pandemic Stress and Sleep Variation on Menstrual Cycle Occurrence, its Severity and Premenstrual Syndrome: A Cross Sectional Study
Article Information
Abhishek Dhawan1*, Jeeja Hernole2
1Consultant Scientist, Research Department Agricultural Development Trust, Baramati, India
2Research Scholar, Department of Biotechnology, Visvesvaraya Technological University, Karnataka, India
*Corresponding author: Abhishek Dhawan, Consultant Scientist, Research Department Agricultural Development Trust, Baramati, India
Received: 28 October 2020; Accepted: 10 November 2020; Published: 17 November 2020
Citation:
Abhishek Dhawan, Jeeja Hernole. Effect of Perceived Pandemic Stress and Sleep Variation on Menstrual Cycle Occurrence, its Severity and Premenstrual Syndrome: A Cross Sectional Study. Journal of Women’s Health and Development 3 (2020): 437-445.
View / Download Pdf Share at FacebookAbstract
Background: Global health crisis, the 2020 pandemic situation has affected the lives of human beings on the physical and mental front. Women and their menstrual and endocrinological health has been severely affected due to imposed pandemic stress. This study attempted to evaluate this effect on women (n=59) during the lockdown and correlate their imposed stress, changed work and sleep pattern on their reproductive health.
Result: The study directs that variation in sleep affected the onset of menstrual cycles in all (n=59) women in terms of early or delay occurrence, where sleep delay and elevated stress are directly proportional to the variation in menstrual cycle experience and PMS. Frustration in women increased with the degree of irritation; moreover, the combined effect of frustration levels and sleep variation was observed on menstrual cycles and PMS.
Conclusion: From the study we can find a direct correlation between variation in sleep time in terms of delay and elevated frustration during lockdown directly affected irregularity of menstrual cycle onset and had prevalent effect on severity of premenstrual syndrome which is indicative of adverse effect of pandemic on women health.
Keywords
Menstrual cycle, Sleep, Lockdown, Stress, Premenstrual syndrome, Depression
Menstrual cycle articles Menstrual cycle Research articles Menstrual cycle review articles Menstrual cycle PubMed articles Menstrual cycle PubMed Central articles Menstrual cycle 2023 articles Menstrual cycle 2024 articles Menstrual cycle Scopus articles Menstrual cycle impact factor journals Menstrual cycle Scopus journals Menstrual cycle PubMed journals Menstrual cycle medical journals Menstrual cycle free journals Menstrual cycle best journals Menstrual cycle top journals Menstrual cycle free medical journals Menstrual cycle famous journals Menstrual cycle Google Scholar indexed journals Sleep articles Sleep Research articles Sleep review articles Sleep PubMed articles Sleep PubMed Central articles Sleep 2023 articles Sleep 2024 articles Sleep Scopus articles Sleep impact factor journals Sleep Scopus journals Sleep PubMed journals Sleep medical journals Sleep free journals Sleep best journals Sleep top journals Sleep free medical journals Sleep famous journals Sleep Google Scholar indexed journals Lockdown articles Lockdown Research articles Lockdown review articles Lockdown PubMed articles Lockdown PubMed Central articles Lockdown 2023 articles Lockdown 2024 articles Lockdown Scopus articles Lockdown impact factor journals Lockdown Scopus journals Lockdown PubMed journals Lockdown medical journals Lockdown free journals Lockdown best journals Lockdown top journals Lockdown free medical journals Lockdown famous journals Lockdown Google Scholar indexed journals Stress articles Stress Research articles Stress review articles Stress PubMed articles Stress PubMed Central articles Stress 2023 articles Stress 2024 articles Stress Scopus articles Stress impact factor journals Stress Scopus journals Stress PubMed journals Stress medical journals Stress free journals Stress best journals Stress top journals Stress free medical journals Stress famous journals Stress Google Scholar indexed journals Premenstrual syndrome articles Premenstrual syndrome Research articles Premenstrual syndrome review articles Premenstrual syndrome PubMed articles Premenstrual syndrome PubMed Central articles Premenstrual syndrome 2023 articles Premenstrual syndrome 2024 articles Premenstrual syndrome Scopus articles Premenstrual syndrome impact factor journals Premenstrual syndrome Scopus journals Premenstrual syndrome PubMed journals Premenstrual syndrome medical journals Premenstrual syndrome free journals Premenstrual syndrome best journals Premenstrual syndrome top journals Premenstrual syndrome free medical journals Premenstrual syndrome famous journals Premenstrual syndrome Google Scholar indexed journals Depression articles Depression Research articles Depression review articles Depression PubMed articles Depression PubMed Central articles Depression 2023 articles Depression 2024 articles Depression Scopus articles Depression impact factor journals Depression Scopus journals Depression PubMed journals Depression medical journals Depression free journals Depression best journals Depression top journals Depression free medical journals Depression famous journals Depression Google Scholar indexed journals mental articles mental Research articles mental review articles mental PubMed articles mental PubMed Central articles mental 2023 articles mental 2024 articles mental Scopus articles mental impact factor journals mental Scopus journals mental PubMed journals mental medical journals mental free journals mental best journals mental top journals mental free medical journals mental famous journals mental Google Scholar indexed journals physical health articles physical health Research articles physical health review articles physical health PubMed articles physical health PubMed Central articles physical health 2023 articles physical health 2024 articles physical health Scopus articles physical health impact factor journals physical health Scopus journals physical health PubMed journals physical health medical journals physical health free journals physical health best journals physical health top journals physical health free medical journals physical health famous journals physical health Google Scholar indexed journals endocrine articles endocrine Research articles endocrine review articles endocrine PubMed articles endocrine PubMed Central articles endocrine 2023 articles endocrine 2024 articles endocrine Scopus articles endocrine impact factor journals endocrine Scopus journals endocrine PubMed journals endocrine medical journals endocrine free journals endocrine best journals endocrine top journals endocrine free medical journals endocrine famous journals endocrine Google Scholar indexed journals PMS articles PMS Research articles PMS review articles PMS PubMed articles PMS PubMed Central articles PMS 2023 articles PMS 2024 articles PMS Scopus articles PMS impact factor journals PMS Scopus journals PMS PubMed journals PMS medical journals PMS free journals PMS best journals PMS top journals PMS free medical journals PMS famous journals PMS Google Scholar indexed journals
Article Details
1. Introduction
The global health crisis that emerged during the covid-19 pandemic has negatively impacted the overall health index most profoundly women's mental and physical health. In India, march onwards lockdown was imposed and the succeeding "unlock" limited the intra and extra movement of individuals. For both working and nonworking women, situations such as continually being with family members, limited movement in the outside world, and work from home imposed stress at different levels. The perceived stress affected the mental as well as physical health of the women. Stress induces stressors, the endocrine factors that impede the regulation of body systems such as the menstrual cycle, which eventually disrupts the body's normal functioning. Stress not only affects the endocrinological and reproductive factors but also it involves the physiological factors [1].
Menstrual cycle (MC) related problems are prevalent in Indian women of all reproductive age groups [2-4]. Common problems associated with the menstrual cycle are irregular periods, menstrual flow changes, and premenstrual syndrome, including migraine, sleepiness, fatigue, pelvic pain, bloating, etc. [5]. There are series of studies which report that an abnormal menstrual cycle may lead to the occurrence of severe multidimensional health conditions such as infertility, diabetes, cardiovascular disease, obesity, breast cancer and may also affect the mental health by causing depression, anxiety, tiredness, insomnia among women [6, 7]. This might profoundly impact the overall health of women and result in productivity loss in day-to-day activities, school, and workplace [8-10]. Various factors affect the menstrual cycle, such as physiological, medical, and lifestyle, including day to day stress [11].
This research has tried to correlate the pandemic stress effect on women's reproductive health involving the menstrual cycle and premenstrual syndrome (PMS). We devised a study to understand how the pandemic and lockdown stages have affected women's health due to stress, change in schedules, and other stressors concerning female reproductive factors. Also, the study aimed to find the correlation between reported intrinsic factors and its effects, if any, are interlinked to impact menstrual cycle [12].
2. Methodology
The study was based on a survey analysis method [13]. The questionnaire was made using Google forms and circulated for getting the responses from women of different ages and marital status. The research was survey based and does not involve experiments on humans or human tissue. The written consent and approval was taken from the participants as per relevant guidelines and regulations. The total number of responses received were n=59 after error correction and removal of ambiguous answers. The questionnaire form had 17 questions as per given in the supplemental file. The questions were related to sleep timing, wake timings, experienced frustration level, menstrual cycle occurrence timings, PMS occurrence, PMS severity, Self-reported sleep quality, and reasons, making them frustrated, as given in Table 1.
|
Question |
Options for Selection |
|
Marital Status |
Married, Unmarried, Single |
|
If you Experience delay or change in the menstrual cycle, what was it? |
Early, Mild delay between 1-2 days, Delay between 2-5 or more, Normal cycle |
|
How severe are your mood swings/PMS in these few months as compared to normal? |
No Mood swings or PMS, Mildly sever, Moderately severe, Severe |
|
What was the change in your sleeping time? |
Slept more than 2 hour late, Slept one to two hour late, Slept half to one hour late, Slept as normal one |
|
What was the change in your waking time? |
Woke more than 2 hour late, Woke one to two hour late, Woke half to one hour late, Woke as normal one |
|
How much more frustrated you are as compared to normal days? |
Select on scale of 1 to 10, 1 being normal and 10 being worst |
|
What are the things that make you more irritated these days, Select as many as you can? (Multiple selection allowed) |
Constantly being with partners, Increased workload, Unable to move out, Health concern, Can't tell |
|
Did you feel depressed? |
Sometimes, Once a week, Mostly, Never |
|
What specific menstrual or PMS changes you noticed? |
Self reported answers |
Table 1: Survey questions and answer selection choices given in survey questions.
The questionnaire was designed to extract specific information relevant to the research focus and make analysis and find the interlinked factors amongst lockdown, change in schedules, stress, and menstrual cycle. The form was shared using social media platforms, and consent was taken before participants filled out the sheet. The data was collected in an excel sheet for analysis using statistical methods.
2.1 Observation
All women included were in their reproductive stage of life in age range 20 to 54 years. 69.49% were married (n=41), 22.03% were unmarried (n=13) and 8.47% single (n=5). Noteworthy, 100% women experienced changes in their menstrual cycle (n=59). 25.42% experienced early (n=15), 49.16% had mild delay between 1-2 days (n=29), 25.42% experienced delay between 2-5 or more days (n=15) (Table 2).
|
Irregularity of Menstrual cycle occurrence |
||
|
Early Experience = 15 |
Mild Delay = 29 |
Moderate Delay = 15 |
|
25.42% |
49.16% |
25.42% |
Table 2: Observation of menstrual irregularity from study.
Most of the Women experienced variation in sleep timings and had changed either sleep or wake timings or both.
18.64% of women slept at usual time and woke up at usual time (SNWN, n=11), 22.04% slept late and woke up
usual time, being sleep deprived (SLWN, n=13), 10.16% slept at usual time and woke up late, being overslept (SNWL, n=6), and 49.15% slept late and woke up late, change in sleep time (SLWL, n=29) (Table 3).
|
Sleep and wake time |
|||
|
SN and WN = 11 |
SL and WN = 13 |
SN and WL = 6 |
SL and WL = 29 |
|
18.64% |
22.04% |
10.16% |
49.15% |
Table 3: Observation of sleep and wake delays.
These women reported their sleep quality on scale of 1 to 10 (normal to severe) compared to normal days, 20 women rated sleep normal to mild (rating 1 to 3), 30 women rated sleep moderately disturbed (rating 4 to 7) and 9 reported their sleep severely changed (rating 8 to 10). Women reported their frustration on the scale of 1 to 10 (normal to severe), 9 women had normal to moderate level (rating 1 to 3), 30 had moderate level (rating 4 to 7), and 20 had severe level (rating 8 to 10) of frustration. 13.55% Women never experienced depression (n=8), 40 women were depressed sometimes (n=40), 3.38% experienced depression once a week (n=2) , and 15.25% experienced depression most of the time (n=9) (Table 4).
|
Depression |
|||
|
Never Felt = 8 |
Sometimes = 40 |
Once week = 2 |
Mostly felt = 9 |
|
13.55% |
67.79% |
3.38% |
15.25% |
Table 4: Observation of reported depression.
3. Results
3.1 Effect of changes in sleep time on menstrual cycle
The statistical and correlative difference in two distant categories of women who reported mostly depressed (n=9) and never depressed (n=8) were filtered from the complete data (n=59). These women’s sleep data was correlated with the menstrual cycle and PMS. In the most depressed women group (Table 5), the occurrence frequency of individuals who slept two or more hours late was highest, followed by mild sleep delay and normally slept. Vice-versa in the never depressed group (Table 6), it was observed that the frequency of individuals who slept normally was highest, followed by mild sleep delay, and people slept two or more hours late.
|
Mostly depressed reported stats |
|||
|
Cycle occurrence |
2-5 Days Delay = 56% |
1-2 Day delay = 22% |
Early Experience = 22% |
|
PMS Severity |
Mild PMS = 44% |
Moderate PMS = 44% |
Severe PMS = 12% |
|
Sleep Delay |
2 hour of late = 56% |
1 hour of late = 22% |
Normal Sleep=22% |
Table 5: Statistical analysis and correlation between Cycle occurrence, PMS and Sleep delay in mostly depressed women.
|
Never depressed reported stats |
|||
|
Cycle occurrence |
2-5 Days Delay = 00% |
1-2 Day delay = 89% |
Early Experience = 11% |
|
PMS |
Mild PMS = 88% |
Moderate PMS = 12% |
Severe PMS = 0% |
|
Sleep |
2 hour of late = 12% |
1 hour of late = 38% |
Normal Sleep = 50% |
Table 6: Statistical analysis and correlation between Cycle occurrence, PMS and Sleep delay in mostly depressed women.
Variation in sleep time affected the occurrence of the menstrual cycle and PMS. As shown in Graph 1 (2 hours late, 1 hour late, and normal), the frequency of sleep variation is directly proportional to variation in menstrual cycle experience (2-5 delay, 1-2 delay, and early experience). The mostly depressed group had maximum participants in Moderate delay while the never depressed group maximum participants in mild delay and no participants in moderate delay.
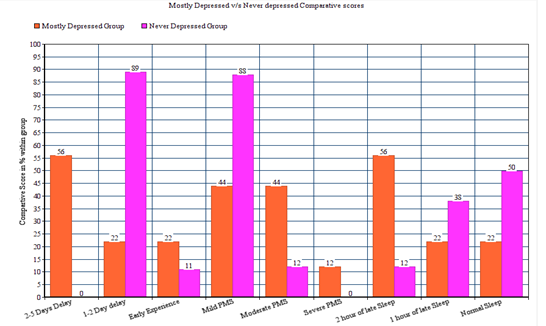
Graph 1: comparative analysis of menstrual cycle analysis in never felt depressed v/s mostly felt depressed group.
3.2 Frustration increased with the degree of reason selection
The participants had to rate their frustration levels and choose prescribed reason/s for their irritation. The study shows that the degree of frustration is directly proportional to the number of reasons participants selected that irritated them. To estimate the degree of frustration, the mean threshold was calculated by taking the average of frustration rating belonging to a particular degree of irritation. Here, we observed that the degree of frustration is directly proportional to the degree of irritation or increased number of reasons as seen in (Table 7).
|
No.of Reasons |
One reason n=26 |
Two reasons n=21 |
Three or more n=12 |
|
Mean Frustration |
5.5 |
6.14 |
7.25 |
|
1 to 5 |
n=13 |
n=9 |
n=3 |
|
6 to 10 |
n=13 |
n=12 |
n=9 |
Table 7: Statistical analysis and correlation between No. of reasons selected, mean frustration score and bound.
Also the internal correlation between upper bound (6 - 10 out of 10 rating) and lowerbound (1 - 5 out of 10 rating) scales is distinctive. As the number of reasons increased in selection, shifts in intensity from lower bound score to upper bound increased.
3.3 Combined relation of sleep delay and mean frustration on menstrual cycle occurrence
Combined effect of sleep delay with stress is an important aspect of this study as both factors seem to be in sync with each other as we saw in observation. The relative progressive delay in sleep time has coincided with the elevation in mean frustration score among the same group (Table 8). As the sleep delay increases in hours the mean frustration score is also increased as compared to normal. And in the same group the comparative ratio of mild v/s moderate delay invariant of early experienced participants has also changed consistently in accordance with normal scores. As the sleep time delayed the mild cases lowered and moderate cases raised within the intragroup (Graph 2).
|
Sleep Delay |
Normal time of sleep (n=17) |
Half to one Hour (n=16) |
One to two hour (n=10) |
Two or more hour (n=16) |
|
Mean Frustration |
5.29 |
6.06 |
6.9 |
6.43 |
|
Median |
5 |
5.5 |
7.5 |
6.5 |
|
Early in % |
21.42 |
37.5 |
10 |
25 |
|
Mild in % |
71.42 |
43.75 |
50 |
37.5 |
|
Moderate in % |
7.14 |
18.75 |
40 |
37.5 |
Table 8: Statistical analysis and correlation between Sleep timing slots, average frustration and combined effect on menstrual cycle.
In the group that slept late for more than two hours has slight reduction in mean frustration score as compared to previous group indicating this group may have entered the resistance phase (Herrera et al., 2016) due to chronic stress exposure.
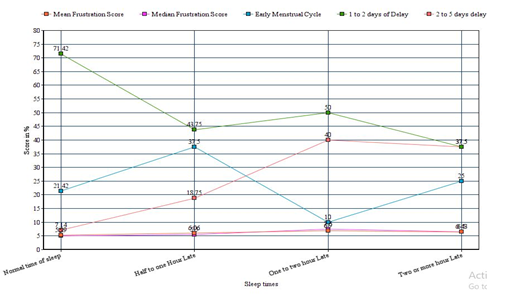
Graph 2: Correlation between Sleep timing slots, average frustration and combined effect on menstrual cycle.
4. Discussion
Our study shows a significant correlation of timing sleep and frustration magnitude with menstrual cycle occurrence and irregularity. Studies [14] have shown variation and change in the quality of sleep, and sleep time affects experience, emergence, and physical parameters of the Menstrual cycle and PMS. Sleep is regulated by the optimum levels of circulating endocrine factors such as cortisol, melatonin, and estrogen, which favors the undisturbed sleep that refers to the quality of sleep, and in turn, maintain the hormonal cycles [15-17]. Sleep hour variation and delay or sleep restriction deregulate these endocrine factors' secretion or equilibrium [18, 19]. Cortisol has diurnal behavior. It is tentatively low at nights and elevated in morning [20]. Delay in sleep, and elevated stress and stressors promote cortisol dysregulation and a change in cortisol awakening response (CAR) [21]. Change in cortisol behavior results in the irregularity of the menstrual cycle, increased prevalence of PMS. Long-term exposure to adverse changes in sleep patterns and stress may result in cortisol affecting other physiological parameters and hormones of the body [1] and the body’s mechanisms to counteract stress [22]. High frustration and depression may result in estrogen imbalance, a primary factor of feminine physiology, further supporting and triggering irregularity in the menstrual cycle and elevating the severity of mood swings. This may also result in more accumulation of stress. As per previous literature, CAR response was low in the women in the follicular phase having sleep variation [18], Whereas in normal conditions without any sleep variation, the CAR was elevated in the follicular stage [23]. There is a significant correlation between deprived sleep, high levels of endocrine factors, and irregular menstrual cycles [24]. In addition to this, the estrogen levels affect the sleep as well as the menstrual cycle [25]. Altogether, a disrupted Sleep-wake cycle, elevated stress, and hormonal secretion may lead to the menstrual cycle's demodulation.
4.1 Declarations
- Ethics approval and consent to participate: The studies involving human participants for "Effect of perceived pandemic stress and sleep variation on menstrual cycle occurrence, its severity and premenstrual syndrome: a cross sectional study" were taken with written consent before participation. The participants of the survey have provided their written informed consent to participate in the survey with their own will.
- Consent for publication: Publisher the permission of the Authors 1,2 to publish the Work in respected journal.
- Availability of data and materials: The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
- Conflict of Interest: The author declares that the research was conducted in the absence of any commercial or financial relationships construed as a potential conflict of interest. Author declares that he has no conflict of interest.
- Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
- Authors' contributions: Both the Authors 1,2 have contributed in data collection, survey and analysis of the study.
References
- Nagma S, Kapoor G, Bharti R, Batra A, Batra A, Aggarwal A, et al. To evaluate the effect of perceived stress on menstrual function. Journal of clinical and diagnostic research: JCDR 9 (2015): QC01.
- Thakre S B, Thakre S S, Ughade S, Thakre A D. Urban-rural differences in menstrual problems and practices of girl students in Nagpur, India. Indian pediatrics 49 (2012): 733-736.
- Dambhare D G, Wagh S V, Dudhe J Y. Age at menarche and menstrual cycle pattern among school adolescent girls in Central India. Global journal of health science 4 (2012): 105.
- Omidvar S, Amiri F N, Bakhtiari A, Begum K. A study on menstruation of Indian adolescent girls in an urban area of South India. Journal of family medicine and primary care 7 (2018): 698.
- Clayton A H. Symptoms related to the menstrual cycle: diagnosis, prevalence, and treatment. Journal of Psychiatric Practice® 14 (2008): 13-21.
- Case A M, Reid R L. Menstrual cycle effects on common medical conditions. Comprehensive therapy 27 (2001): 65-71.
- Berga S L. The Menstrual Cycle and Related Disorders. Female Reproductive Dysfunction (2020): 23-37.
- Nappi R E, Lete I, Lee L K, Flores N M, Micheletti M C, Tang B. Real-world experience of women using extended-cycle vs monthly-cycle combined oral contraception in the United States: the National Health and wellness survey. BMC women's health 18 (2018): 22.
- Schoep M E, Adang E M, Maas J W, De Bie B, Aarts J W, Nieboer T E. Productivity loss due to menstruation-related symptoms: a nationwide cross-sectional survey among 32 748 women. BMJ open 9(2019): e026186.
- Swani R. Labor Resilience: Paid Menstrual Leave and Women’s Economic Empowerment in India. International Journal of Social Science and Economic Research 5 (2020).
- Bae J, Park S, Kwon J W. Factors associated with menstrual cycle irregularity and menopause. BMC women's health 18 (2018): 36.
- Jehan S, Auguste E, Hussain M, Pandi-Perumal S R, Brzezinski A, Gupta R, et al. Sleep and premenstrual syndrome. Journal of sleep medicine and disorders 3 (2016).
- Hayes B E, Hayes B E. Measuring customer satisfaction: Survey design, use, and statistical analysis methods. Milwaukee^ eWisconsin Wisconsin: ASQC Quality Press (1998).
- Baker F C, Kahan T L, Trinder J, Colrain I M. Sleep quality and the sleep electroencephalogram in women with severe premenstrual syndrome. Sleep 30 (2007): 1283-1291.
- Parry B L, Martínez L F, Maurer E L, López A M, Sorenson D, Meliska C J. Sleep, rhythms and women's mood. Part II. Menopause. Sleep medicine reviews 10 (2006): 197-208.
- Touitou Y, Reinberg A, Touitou D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: Health impacts and mechanisms of circadian disruption. Life sciences 173 (2017): 94-106.
- Bush B, Hudson T. The role of cortisol in sleep. Natural Medicine Journal 2 (2010): 2010-2016.
- Omisade A, Buxton O M, Rusak B. Impact of acute sleep restriction on cortisol and leptin levels in young women. Physiology & behavior 99 (2010): 651-656.
- LeRoux A, Wright L, Perrot T, Rusak B. Impact of menstrual cycle phase on endocrine effects of partial sleep restriction in healthy women. Psychoneuroendocrinology 49 (2014): 34-46.
- Bao A M, Ji Y F, Van Someren E J, Hofman M A, Liu R Y, Zhou J N. Diurnal rhythms of free estradiol and cortisol during the normal menstrual cycle in women with major depression. Hormones and behavior, 45 (2004): 93-102.
- Elder G J, Wetherell M A, Barclay N L, Ellis J G. The cortisol awakening response–applications and implications for sleep medicine. Sleep medicine reviews 18 (2014): 215-224.
- Jarcho M R, Slavich G M, Tylova-Stein H, Wolkowitz O M, Burke H M. Dysregulated diurnal cortisol pattern is associated with glucocorticoid resistance in women with major depressive disorder. Biological psychology 93 (2013): 150-158.
- Wolfram M, Bellingrath S, Kudielka B M. The cortisol awakening response (CAR) across the female menstrual cycle. Psychoneuroendocrinology 36 (2011): 905-912.
- Shreeve N, Cagampang F, Sadek K, Tolhurst M, Houldey A, Hill C M, et al. Poor sleep in PCOS; is melatonin the culprit. Hum Reprod 28 (2013): 1348-1353.
- Morssinkhof M W L, van Wylick D W, Priester-Vink S, van der Werf Y D, den Heijer M, van den Heuvel O A, et al. Associations between sex hormones, sleep problems and depression: A systematic review. Neuroscience & Biobehavioral Reviews (2020).


 Impact Factor: * 1.1
Impact Factor: * 1.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 