Effectiveness of Passive Chest Physiotherapy in Prevention of Ventilator Associated Pneumonia in Sepsis
Article Information
Nida Rizvi1*, Syed Muhammad Fahad2, Syed Hasan Abbas Rizvi3, Faizan Saeed Syed2, Syed Ali Farooq Zaidi2, Adnan Anwar4, Muhammad Ali5
1Trainee Physiotherapist, Liaquat National School of Physiotherapy, Karachi, Pakistan
2Senior Physiotherapist, Liaquat National School of Physiotherapy, Karachi, Pakistan
3Prinicipal, Associate Professor, Liaquat National School of Physiotherapy, Karachi, Pakistan
4Assistant Professor, Al Tibri Medical College, Karchi, Pakistan
5Assistant Professor, Liaquat National School of Physiotherapy, Karachi, Pakistan
*Corresponding author: Nida Rizvi, Trainee Physiotherapist, Liaquat National School of Physiotherapy, Karachi, Pakistan
Received: 05 May 2020; Accepted: 11 May 2020; Published: 15 June 2020
Citation: N, Fahad SM, Rizvi SHA, Syed FS, Zaidi SAF, et al. Effectiveness of Passive Chest Physiotherapy in Prevention of Ventilator Associated Pneumonia in Sepsis. Archives of Physiotherapy and Rehabilitation 3 (2020): 041-052.
View / Download Pdf Share at FacebookAbstract
Background: Around 19 million cases of sepsis are reported annually, with 5 million deaths are estimated to be recorded in middle and low income countries due to sepsis. Ventilator Associated Pneumonia is most common risk factor associated with sepsis. Passive chest physiotherapy involves various techniques including Percussions, Compression and Manual Hyperinflation Technique for external manipulation; they basically dislodge chest secretions by applying kinetic energy to chest wall.
Objective: To evaluate effectiveness of passive chest physiotherapy in prevention of ventilator associated pneumonia in sepsis.
Methodology: This was a Quasi Experimental Study conducted in Liaquat National Hospital from February October with non probability convenient based sampling. Total 60 intubated patients diagnosed with sepsis on the basis of American college of chest physicians and society of critical care principle or conditions that could lead to sepsis like impaired immune system, infection, renal failure, burn, Urinary Tract Infection,exposure to invasive devices were included in this study. Excluded were those with pulmonary embolism, pulmonary edema, clotting disorders, osteoporosis of ribs, lung contusion,emphysema, Intracranial pressure greater than 20mmHg, hemodynamically unstable patients, cardiac problems, skin infections . Ethical Approval was taken from Institutional Review Board of Liaquat National School Of Physiotherapy. Passive chest physiotherapy was administered to patient twice daily (11:00 am and 3:30 pm) in 10 days. Patients were given standard care as per ICU protocol in the form of nursing, pharmacology as prescribed by physician/Surgeon throughout intervention period. Acute Physiology, Age, Chronic Health Evaluation II (APACHE II) and Clinical Pulmonary Infection Scoring (CPIS) were used as assessment tools. Data was analyzed using spss 22.0.
Keywords
Effectiveness; Passive Chest Physiotherapy; Physiotherapy; Prevention; Ventilator; Ventilator Associated Pneumonia; Sepsis
Effectiveness articles, Passive Chest Physiotherapy articles, Physiotherapy articles, Prevention articles, Ventilator articles, Ventilator Associated Pneumonia articles, Sepsis articles
Article Details
Abbreviations:
APACHE II- Acute Physiology, Age, Chronic Health Evaluation II; APACHE- Acute Physiology, Age, Chronic Health Evaluation; CPIS- Clinical Pulmonary Infection Scoring; VAP- Ventilator Associated Pneumonia; CMV- Continous Mandatory Ventilation; PCV- Pressure Control Ventilation; SIMV- Synchronized Intermittent Mandatory Ventilation; MHT- Manual Hyperinflation Technique; Na- Sodium; k- Pottasium; Fio2- Fraction Of Inspired Oxygen; Aado2- Alveolar Arterial Oxygen Gradient; PaO2- Partial Pressure of Oxygen; WBC- White Blood Cell; Hct- Hematocrit; LAMA- Leaving Against Medical Advice; mmHg- Millimetre of mercury; mmol/L- Milimoles per litre; mm3- Milimeter per cube; °C- Degree Celsius
1. Introduction
Around the world 19 million cases of sepsis are reported, with 5 million deaths are estimated to be in middle and low income countries due to sepsis [1]. 95% deaths are occurring in low and middle income countries due to maternal sepsis [2]. Sepsis by definition is a ‘life-threatening organ dysfunction caused by a dysregulated host response to infection’ [3]. American college of Chest Physicians and society of critical care medicine established standard principle in classification of sepsis on basis of their symptoms in which Systemic Inflammatory response is define as Core Body temperature > 38°c or < 36 °c, Heart Rate ≥ 90 bpm, Respiratory Rate ≥ 20/min (or PaCO2 <32 mmHg),White blood cells ≥ 12,000/μl or ≤ 4000/μl or >10% immature forms, Sepsis is define on at least 2 or more systemic inflammatory response criteria with underlying infection, Severe sepsis involve sepsis with organ damage, Septic shock involve sepsis with persistent or refractory low blood pressure [4-6]. Proper management of patients diagnosed with sepsis can only be done by knowing rate of mortality [7]. Severity and mortality of Patient admitted in Intensive care unit (Icu) with sepsis can be analyzed by scale i. e. Acute Physiology, Age and Chronic Health Evaluation II (APACHE II) introduced by Knaus et al. in 1985 which was considered as modification of Acute Physiology, Age and Chronic Health Evaluation (APACHE) by removing infrequently used variables like lactate, osmolality [8]. Respiratory Tract Infections frequently leads to sepsis [9]. Other sources of sepsis include urinary tract, abdomen, invasive devices, central nervous system, endocarditis [10].
Ventilator Associated Pneumonia (VAP) is considered as common risk factor frequently associated with intubated sepsis patients [11]. It is common problem in patient intubated for more than 48 hours. Estimated occurrence of ventilator associated pneumonia is around 9-27% of all mechanically ventilated patients [12]. VAP leads to difficulty in weaning off leading to increase financial and medical resources burden. Common risk factors that increase chances of VAP are classified into modifiable factors and non-modifiable factors. Modifiable factors include Prolong Supine Positioning, abdominal distention, colonization in ventilator circuit, low pressure in endotracheal tube cuff circuit while nonmodifiable factors include gender, immunocompromised, history of trauma or disease and old age (over 60 years) [13, 14]. Clinical diagnosis of Ventilator Associated Pneumonia is often difficult due to decreased sensitivity and specificity. Based on 6 parameters, In 1992 Clinical Pulmonary infection score was evolved [14]. As discussed above that any patient intubated for more than 48 hours can develop Ventilator Associated Pneumonia so prevention of ventilator associated pneumonia begins with decreasing time of mechanical ventilation which can only be decreased by using strategies that includes use of Noninvasive positive pressure ventilator [15, 16], avoiding reintubation, early tracheostomy [17] and preventive measures which includes elevation of bed to 45 degree, antimicrobial coated endotracheal tube, endotracheal suctioning [15] . Patients intubated for prolong time are with impaired level of consciousness and absence of cough reflex which shows significant reduction in airway clearance [18]. Passive Chest physiotherapy is commonly used to promote airway clearance, to overcome ventilation perfusion mismatch in mechanically ventilated patient [19, 20]. Passive Chest physiotherapy uses manual techniques that are responsible for sputum clearance and help in preventing lung from atelectasis, air way obstruction, and hyperinflation. Passive Chest Physiotherapy is also responsible for removing infected secretions by decreasing rate of proteolytic tissue damage [21]. Passive chest physiotherapy involves various techniques for external manipulation of thorax. They basically dislodge chest secretions by applying kinetic energy to chest wall [22]. Passive Chest Physiotherapy plays significant role in ICU patients but there was very low data regarding prevention of ventilator associated pneumonia in sepsis patients through passive chest physiotherapy so this study was conducted to assess efficacy of Passive Chest Physiotherapy in Prevention of Ventilator Associated Pneumonia in Sepsis Patients.
2. Methodology
This was a Quasi Experimental study conducted in Liaquat National Hospital from February to October 2019 with convenient based non probability sampling technique. Total 60 patients were included in this study. All those patients intubated for more than 48 hours, diagnosed with sepsis on the basis of American college of chest physicians and society of critical care principle [6] or conditions that leads to sepsis including Urinary Tract Infection, burns,invasive devices, Immunocompromised patients, Acute Kidney Injury, Chronic Kidney disease, End Stage Renal Disease, Diabetic Ketoacidosis, Neurological cases, Poisoning, Post-surgical complications were included in this study while those who suffered from undrained pneumothorax, Pulmonary embolism, pulmonary edema, clotting disorders, osteoporosis of ribs, lung contusion, emphysema, Intra cranial pressure greater than 20 mm hg, hemodynamically unstable patients, myocardial infarction, irregular arrhythmias, hemodialysis, recent open heart surgery, open wounds or skin infections were excluded from this study. Ethical Approval was taken from Institutional Review Board of Liaquat National School Of Physiotherapy before commencement of this study.
Patients included in this study were served with positive pressure ventilator including Continous Mandatory Ventilation (CMV), Pressure Control Ventilation (PCV) and Synchronized Intermittent Mandatory Ventilation (SIMV). Informed consent form was signed by patient’s relative. Informed consent form consisted of purpose of the study as well as description of procedure, All risk and benefits were mentioned in informed consent form . After taking informed consent form from patient’s relative, baseline assessment was done which included Gender, age, diagnosis, comorbid and mode of ventilator used. Acute Physiological Age Chronic Health Evaluation II (APACHE II) And Clinical Pulmonary Infection Scoring (CPIS) scales were used as assessment tools [23]. Acute Physiological Age Chronic Health Evaluation II also known as APACHE II was used for measuring mortality rate of patients [7, 24]. Ayazogu TA in his study showed that sensitivity and specificity of APACHE II for predicting mortality rate was 100% and 86. 6% respectively [25]. APACHE II was based on 12 variables including mean arterial blood pressure, heart rate, temperature, oxygenation, respiratory rate, arterial PH, serum sodium, potassium and creatinine, hematocrit, white blood cell count, and GCS and chronic health, age score. Each variable was ranked from 0-4. APACHE II score ranged from 0-71. Score of 25% represents mortality 50% and score of over 35% represents mortality 80%. APACHE II was calculated during first 24 hours in ICU to predict mortality rate of patients admitted in ICU [26]. APACHE II scoring has been shown in Table 1. Clinical Pulmonary Infection Scoring also known as CPIS scoring was used as diagnostic tool for confirmation of ventilator associated pneumonia with sensitivity of 79% and specificity of 75% as shown in Swoboda SM et al. study [27]. CPIS scoring scale was based on 6 parameters including Temperature, WBC count, tracheal secretions, pulmonary radiography, oxygenation, tracheal culture. Score greater than 6 considered as Likelihood of Ventilator associated pneumonia [14]. CPIS scoring has been shown in Table 2. All 60 patients received same treatment i. e. Passive Chest Physiotherapy. Total days of treatment session were 10 days and twice daily i. e. 11:00 am and 3:30 PM. CPIS scoring was taken in all 10 days to measure difference before initiation of passive chest physiotherapy and at end of passive chest physiotherapy session. Standard care in terms of nursing, drugs, therapies as implemented by doctor was strictly followed throughout the intervention. The treatment of patient was left entirely on decision of senior intensivist or doctor/surgeon. Passive Chest Physiotherapy administered to patients was as follow:
- Manual Hyperinflation Technique (MHT): It uses technique that delivers deep breaths to patient mechanically ventilated by rebreathing bag [27]. Mapleson Water Circuit of 2L was used. Slow deep inspiration and inspiratory hold at full inspiration was done with both hands to improve collateral ventilation. MHT was carried out twice daily at a rate of 8-13 breaths per minute during 20 minutes session
- Suctioning: Duration of endotracheal suctioning was limited to 15 seconds [28]. Quickly and gently catheter was passed down tube until obstruction was felt and catheter was withdraw 2cm prior to negative pressure, withdrawing of catheter was done with twisting motion while suctioning intermittently. 1-2 ml of normal saline was used to enhance aspiration of dry secretions. Size of Suction catheter used were 14 and 16. Specimen from Lower respiratory tract was collected in sterile mucous extractor for culture testing. After end of suctioning, bed was elevated to 45 degree to improve ventilation for minimum 30 minutes [29].
- Percussions: Percussions are defined as rhythmically striking patient’s chest with cupped hand over area of secretion. The patient was position in supine and therapist hands were placed on patient’s chest, Shoulder, elbows and wrist were straight to apply percussion in wavy motion. Percussions duration used was 5 minutes on each lobe twice daily [30].
- Compressions: Chest compressions are mainly used in mobilization of secretions in central airway from periphery. Patient was positioned supine and therapist placed his fingers over intercostal spaces and shoulder, elbow, wrists were kept straight and compression force was applied at the end of inspiration and start of expiration. Compressions were performed three times on each lobe [30].
Data was analyzed using SPSS 22. 0. Descriptive Statistics was reported. Paired t-test was used to assess the significance. P value of <0. 05 was set as significant level.
|
Physiologic Variable |
Point Score |
|||||||||||
|
+4 |
+3 |
+2 |
+1 |
0 |
+1 |
+2 |
+3 |
+4 |
||||
|
Temperature |
>41 |
39- 40. 9 |
- |
38. 5- 38. 9 |
36-38. 4 |
34-35. 9 |
32- 33. 9 |
30- 31. 9 |
<29. 9 |
|||
|
Mean Arterial Pressure (mmHg) |
>160 |
130- 159 |
110- 129 |
- |
70-109 |
- |
50-60 |
- |
<49 |
|||
|
Heart Rate |
>180 |
140- 179 |
110- 139 |
- |
70-109 |
- |
55-69 |
40-54 |
<39 |
|||
|
Respiratory Rate |
>50 |
35-49 |
- |
25-34 |
12-24 |
10-11 |
6-9 |
- |
<5 |
|||
|
Oxygenation : a) Fio2 >0. 5 (Use AaDo2) b) Fio2 <0. 5 (Use PaO2) |
>500 |
350- 499 |
200- 349 |
- |
<200 |
- |
- |
- |
- |
|||
|
- |
- |
- |
- |
>70 |
61-70 |
- |
55-60 |
<55 |
||||
|
Arterial pH |
>7. 7 |
7. 6- 7. 69 |
- |
7. 5- 7. 59 |
7. 33- 7. 49 |
- |
7. 25- 7. 32 |
7. 15- 7. 24 |
<7. 15 |
|||
|
Serum Na (mMol/L) |
>180 |
160- 179 |
155- 159 |
150- 154 |
130- 149 |
- |
120- 129 |
111- 119 |
<110 |
|||
|
Serum K (mMol/L) |
>7 |
6-6. 9 |
- |
5. 5- 5. 9 |
3. 5-5. 4 |
3-3. 4 |
2. 5- 2. 9 |
- |
<2. 5 |
|||
|
Serum Creatinine (mg/dl) |
>3. 5 |
2-3. 4 |
1. 5-1. 9 |
- |
0. 6-1. 4 |
- |
<0. 6 |
- |
- |
|||
|
Hct (%) |
>60 |
- |
50-59. 9 |
46- 49. 9 |
30-45. 9 |
- |
20- 29. 9 |
- |
<20 |
|||
|
WBC (in 1000S) |
>40 |
- |
20-39. 9 |
15- 19. 9 |
3-14. 9 |
- |
1-2. 9 |
- |
<1 |
|||
|
Glasgow Coma Scale (GCS) SCORE= MINUS ACTUAL GCS |
||||||||||||
Table 1: APACHE II Scoring Scale.
|
CPIS Points |
0 |
1 |
2 |
|
Tracheal Secretions |
Rare |
Abundant |
Purulent |
|
Leukocyte Count (mm3) |
>4,000 and <11000 |
||
|
Temperature °C |
>36. 5 or <38. 4 |
>38. 5 or <38. 9 |
>39 or <36 |
|
Pao2/FIO2 ratio (mmHg) |
>240 or ARDS |
- |
<240 or no ARDS |
|
Chest Radiograph |
No Infiltrates |
Diffused Infiltrates Infiltrates |
Localized |
|
Culture of Tracheal Aspirate |
Negative |
- |
Positive |
Table 2: Clinical Pulmonary Infection Scoring.
3. Result
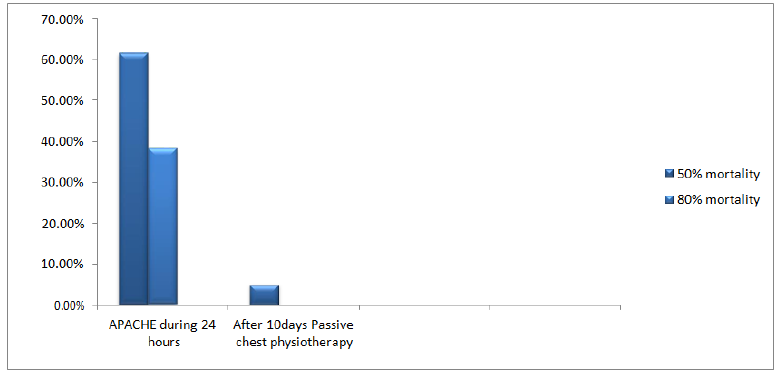
Total 60 patients fulfilled inclusive criteria. Baseline Assessment was measured shown in Table 3. APACHE II was measured during first 24 hours in ICU stay for predicting mortality. Predicted mortality has been Sho-
wn in Table 4. CPIS the main outcome variable was measured before initiation of passive chest physiotherapy and after 10th day of passive chest physiotherapy which showed that chances of ventilator associated pneumonia was 32 (53. 3%) before initiation of passive chest physiotherapy while on 10th day chances of ventilator associated pneumonia decreased to 2 (3. 3%). Passive Chest Physiotherapy was statistically significant in decreasing chances of ventilator associated pneumonia, shown in table 5. On 10th day
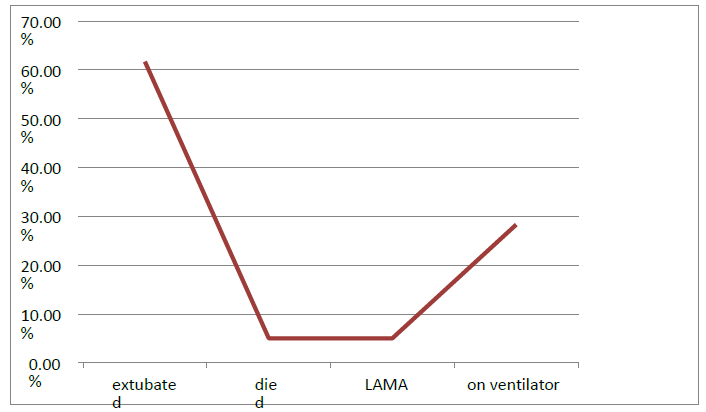
after passive chest physiotherapy out of 60 patients 37 (61. 7%) were extubated, died patients were 3 (5%), Leaving against Medical authority (lama) were 3 (5%) and 17 (28. 3%) were on ventilator at 10 day shown in Graph 1. Mortality rate was found to be decreased on 10th day after passive chest physiotherapy (0. 05 ± 0. 22). Mortality rate has been shown in table 6 and graph 2.
|
Variables |
Mean ± S. D / n (%) |
|
|
Age (years) |
41. 58 ± 12. 93 |
|
|
Gender |
Male |
38 (63. 3%) |
|
Female |
22 (36. 7%) |
|
|
Comorbid |
Hypertension (HTN) |
11 (18. 3%) |
|
Diabetes |
8 (13. 3%) |
|
|
No Known Comorbid |
19 (31. 7%) |
|
|
More than 1Comorbid |
22 (36. 7%) |
|
|
Type Of ICU Stay |
Medical Icu |
18 (31%) |
|
Surgical Icu |
10 (17. 2%) |
|
|
Nephrology Icu |
11 (19. 2%) |
|
|
Chest Icu |
11 (19. 2%) |
|
|
Neurology Icu |
4 (6. 9%) |
|
|
Cardiac Icu |
4 (6. 9%) |
|
|
Mode Of Ventilator |
CMV |
34 (58. 6%) |
|
SIMV |
17 (29. 3%) |
|
|
PCV |
7 (12. 1%) |
|
|
APACHE II |
1. 38 ±0. 49 |
|
{Data are presented as mean?±?SD or number (%)}
Table 3: Characteristics Of Baseline Assessment.
|
Variable |
n% |
|
0% mortality |
37 (61. 7%) |
|
80% mortality |
23(38. 3%) |
{Data are presented as number (%)}
Table 4: Frequency of Mortality Rate using APACHE II.
|
Variable |
CPIS Score Mean ± S. D |
P-Value |
|
|
Passive Chest Physiotherapy |
Before passive chest physiotherapy |
1. 53 ± 0. 50 |
0. 03 |
|
10 Days after Passive Chest Physiotherapy |
1. 28 ± 0. 78 |
||
{Data are presented as mean±SD}
Table 5: Descriptive statistics for Clinical Pulmonary Infection Scoring.
|
on ventilator |
|
LAMA |
|
died |
|
extubated |
|
0.00% |
|
10.00% |
|
20.00% |
|
30.00% |
|
40.00% |
|
50.00% |
|
60.00% |
|
70.00% |
|
Variable |
Mean +- S. D |
p-value |
|
APACHE II during first 24 hours |
1. 38 ± 0. 49 |
0. 00 |
|
Mortality Rate On 10th day after Passive Chest Physiotherapy |
0. 05 ± 0. 22 |
{Data are presented as mean?±SD}
Table 6: Descriptive Statistics Of Mortality Rate.
5. Discussion
This was a quasi-experimental study designed to assess the impact of passive chest physiotherapy in prevention of ventilator associated pneumonia in sepsis. We included patients diagnosed with sepsis or condition that could lead to sepsis, with intubation more than 48 hours Patients included in this study were all treated with passive chest physiotherapy twice daily in total 10 days. This study revealed that mortality rate was significantly decreased at 10th day after passive chest physiotherapy i. e. 3 (5%). Nakagawa NK et al. in their study revealed that immobility in intensive care leads to impaired mucocilliary clearance [31]. Castro et al. [32] in their study showed that Passive Chest physiotherapy included body positioning, percussions and suctioning was significantly effective in decreasing duration of mechanically ventilated patients and decreasing chances of respiratory infections. In our study chances of ventilator associated pneumonia was significantly decreased to 2% (0. 03). Wang TH et al. [33] in their study showed that intensive chest physiotherapy was effective in preventing reintubation (0. 01) and was effective in decreasing rapid shallow breathing index while in our study we found that 31 (61. 7%) were extubated after 10 days passive chest physiotherapy. Grap M et al. [34] in their study revealed that 30 to 45 degree of bed elevation was effective in early preventive measure of ventilator associated pneumonia. Yang M et al. [22] in their study showed that APACHE was useful in predicting mortality of patients diagnosed with ventilator associated pneumonia (0. 00) and CPIS was also found to be useful in diagnosing ventilator associated pneumonia (0. 02). We observed that passive chest physiotherapy was effective in decreasing mortality rate of patients diagnosed with sepsis (0. 00). dos Santos RS et al. [35] in their study showed that passive chest physiotherapy was effective in decreasing lactate (0. 00) and increasing PaO2 (0. 03) after 15 minutes in Septic Shock Patients. Pattanshetty RB et al. [36]. in their study showed that multimodality passive chest physiotherapy twice daily including Manual Hyper Inflation and suctioning was effective in prevention of ventilator associated pneumonia (0. 00) and weaning was successful in 62% patients in the control group receiving Manual Hyperinflation and suctioning. Limitations of this current study were quite few which were that we used convenience based sampling from only 1 hospital, which may not be representative of the entire population . No blinding was held during the entire course of the study.
5. Conclusion
Results of this study showed that passive chest physiotherapy was effective in preventing Ventilator Associated Pneumonia in Sepsis Patient; there was significant decrease in mortality rate after passive chest physiotherapy when compared with before initiation of passive chest Physiotherapy. Further Studies in term of Large Sample size are required to confirm the effectiveness of passive chest physiotherapy in prevention of VAP in Sepsis Patients. Furthermore, this study can be helpful for Physiotherapists to carry out their responsibilities in the ICU in a more professional manner in future. Several patients in the Intensive Care Unit (ICU) suffer from sepsis, which leads to ventilator associated pneumonia among them. By using Passive Chest Physiotherapy we can reduce patients' dependency on ventilators and help in their early discharge from hospitals, help reduce patients' dependency on medicines to a great extent, and bring down the rate of mortality in sepsis, which is quite high in the country.
Conflict of Interest
Author had no conflict of interest
Funding
No funding Received.
Acknowledgment
We are grateful to Dr Zunaira Rais , Dr SM Nadeem Khursheed and Ms Farah deeba who provided their expertise that were very helpful for data collection in this research. We would like to show our gratitude to Mr Sohail Muneer, Mr Farhat Fawad, Mr Amjad Hussain and Ms Sana Noman for sharing their pearls of wisdom with us during critical review of this research.
References
- Fleischmann C, Scherag A, Adhikari NK, et al. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am J Respir Crit Care Med 193 (2016): 259-272.
- Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. The Lancet Global Health 2 (2014): e323-e333.
- Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315 (2016): 801-810.
- Mandell GL, Bennett JE, Dolin R Philadelphia. In Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 6th edition. Elsevier Churchill Livingston (2005): 3661-3664.
- Shankar-Hari M, Phillips GS, Levy ML, et al. Developing new definition and assessing new clinical criteria for septic shock: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315 (2016): 775-787.
- Sen P, Demirdal T, Nemli SA, et al. Diagnostic and prognostic value of new bioscore in critically ill septic patients. Archives of physiology and biochemistry (2019): 1-6.
- Giamarellos-Bourboulis EJ, Norrby-Teglund A, Mylona V, et al. Risk assessment in sepsis: a new prognostication rule by APACHE II score and serum soluble urokinase plasminogen activator receptor. Critical care 16 (2012): R149.
- Naved SA, Siddiqui S, Khan FH. APACHE-II score correlation with mortality and length of stay in an intensive care unit. Journal of the College of Physicians and Surgeons Pakistan 21 (2011): 4.
- Esper AM, Moss M, Lewis CA, et al. The role of infection and comorbidity: Factors that influence disparities in sepsis. Crit Care Med 34 (2006): 2576.
- Mayr FB, Yende S, Linde-Zwirble WT, et al. Infection rate and acute organ dysfunction risk as explanations for racial differences in severe sepsis. JAMA 303 (2010): 2495-2503.
- Raghuram A, Gnoni M, Wiemken TL, et al. Sepsis in Patients with Ventilator Associated Pneumonia due to Methicillin-Resistant Staphylococcus aureus: Incidence and Impact on Clinical outcomes. The University of Louisville Journal of Respiratory Infections 1 (2017): 3.
- Resende MM, Monteiro SG, Callegari B, et al. Epidemiology and outcomes of ventilator-associated pneumonia in northern Brazil: an analytical descriptive prospective cohort study. BMC infectious diseases 13 (2013): 119.
- Hunter JD. Ventilator associated pneumonia. Bmj 344 (2012): e3325.
- Michetti CP, Prentice HA, Rodriguez J, et al. Supine position and nonmodifiable risk factors for ventilator-associated pneumonia in trauma patients. The American Journal of Surgery 213 (2017): 405-412.
- Keyt H, Faverio P, Restrepo MI. Prevention of ventilator-associated pneumonia in the intensive care unit: a review of the clinically relevant recent advancements. The Indian journal of medical research 139 (2014): 814.
- Hess DR. Noninvasive positive-pressure ventilation and ventilator-associated pneumonia. Respir Care 50 (2005): 924-931.
- Ledgerwood LG, Salgado MD, Black H, et al. Tracheotomy tubes with suction above the cuff reduce the rate of ventilator-associated pneumonia in intensive care unit patients. Ann Otol Rhinol Laryngol 122 (2013): 3-8.
- Spapen HD, De Regt J, Honoré PM. Chest physiotherapy in mechanically ventilated patients without pneumonia-a narrative review. J Thorac Dis 9(2017): E44.
- Pisi G, Chetta A. Airway clearance therapy in cystic fibrosis patients. Acta Biomed 80 (2009): 102-106.
- Makhabah DN, Ambrosino N. Airway clearance in the intensive care unit. EMJ Respir 1 (2013): 135-139.
- Holland AE, Button BM. Is there a role for airway clearance techniques in chronic obstructive pulmonary disease? Chron Respir Dis 3 (2006): 83-91.
- Yang M, Yan Y, Yin X, et al. Chest physiotherapy for pneumonia in adults. Cochrane Database of Systematic Reviews (2010).
- Niu T, Luo Q, Li Y, et al. Comparison of Tigecycline or Cefoperazone/Sulbactam therapy for bloodstream infection due to Carbapenem-resistant Acinetobacter baumannii. Antimicrobial Resistance & Infection Control 8 (2019): 52.
- Nair R. A study of acute physiological and chronic health evaluation (apache) index in critically ill patients. Paripex-Indian Journal Of Research 8 (2019).
- Polderman KH, Girbes AR, Thijs LG, et al. Accuracy and reliability of APACHE II scoring in two intensive care units: problems and pitfalls in the use of APACHE II and suggestions for improvement. Anaesthesia 56 (2001): 47-50.
- Taylor SL, Morgan DL, Denson KD, et al. A comparison of the Ranson, Glasgow, and APACHE II scoring systems to a multiple organ system score in predicting patient outcome in pancreatitis. The American journal of surgery 189 (2005): 219-222.
- Swoboda SM, Dixon T, Lipsett PA. Can the clinical pulmonary infection score impact ICU antibiotic days?. Surg Infect (Larchmt) 7 (2006): 331-339.
- Pedersen CM, Rosendahl-Nielsen M, Hjermind J, et al. Endotracheal suctioning of the adult intubated patient-what is the evidence?. Intensive Crit Care Nurs 25 (2009): 21-30.
- Bakhtiari S, Yazdannik A, Abbasi S, et al. The effect of an upper respiratory care program on incidence of ventilator-associated pneumonia in mechanically ventilated patients hospitalized in intensive care units. Iran J Nurs Midwifery Res 20 (2015): 354.
- Kisner C, Colby LA. Therapeutic exercises 5th edition. Jaypee Punlishers (2007).
- Nakagawa NK, Franchini ML, Driusso P, et al. Mucociliary clearance is impaired in acutely ill patients. Chest 128 (2005): 2772-2777.
- Castro AA, Calil SR, Freitas SA, et al. Chest physiotherapy effectiveness to reduce hospitalization and mechanical ventilation length of stay, pulmonary infection rate and mortality in ICU patients. Respiratory medicine 107 (2013): 68-74.
- Wang TH, Wu CP, Wang LY. Chest physiotherapy with early mobilization may improve extubation outcome in critically ill patients in the intensive care units. The clinical respiratory journal 12 (2018): 2613-2621.
- Grap MJ, Munro CL, Unoki T, et al. Ventilator-associated pneumonia: the potential critical role of emergency medicine in prevention. The Journal of emergency medicine 42 (2012): 353-362.
- dos Santos RS, Donadio MV, da Silva GV, et al. Immediate effects of chest physiotherapy on hemodynamic, metabolic, and oxidative stress parameters in subjects with septic shock. Respir Care 59 (2014): 1398-1403.
- Pattanshetty RB, Gaude G. Effect of multimodality chest physiotherapy in prevention of ventilator-associated pneumonia: a randomized clinical trial. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine 14 (2010): 70.
Article Views: 1421
Journal Statistics




Discover More: Recent Articles