Foreign Body Imaging-Experience with 6 Cases of Retained Foreign Bodies in the Emergency Radiology Unit
Article Information
Muniraju Maralakunte MD1, Uma Debi MD1*, Lokesh Singh MD1, Himanshu Pruthi MD1, Vikas Bhatia MD, DNB DM1, Gita Devi MD1, Sandhu MS MD1
2Department of Radio diagnosis, PGIMER, Chandigarh, India
*Corresponding Author: Dr. Uma Debi, Radiodiagnosis and Imaging, PGIMER, Chandigarh, India
Received: 22 June 2020; Accepted: 14 August 2020; Published: 21 September 2020
Citation: Muniraju Maralakunte, Uma Debi, Lokesh Singh, Himanshu Pruthi, Vikas Bhatia, Gita Devi, Sandhu MS. Foreign Body Imaging-Experience with 6 Cases of Retained Foreign Bodies in the Emergency Radiology Unit. Archives of Clinical and Medical Case Reports 4 (2020): 952-968.
View / Download Pdf Share at FacebookAbstract
Introduction: Retained foreign bodies are the external objects lying within the body, which are placed with voluntary or involuntary intentions. The involuntarily or accidentally, and complicated cases with the retained foreign body may come to the emergency services, which may require rapid and adequate imaging assessment.
Materials and methods: We share our experience with six different cases with retained foreign bodies, who visited emergency radiological services with acute presentation of symptoms. The choice of radiological investigation considered based on the clinical presentation of the subjects with a retained foreign body.
Conclusion: Patients with the retained foreign body may present acute symptoms to the emergency medical or surgical services, radiologists play a central role in rapid imaging evaluation. Radiological investigation plays a crucial role in identification, localization, characterization, and reporting the complication of the retained foreign bodies, and in many scenarios, radiological investigations may expose the unsuspected or concealed foreign bodies in the human body. Ultimately radiological services are useful rapid assessment tools that aid in triage and guide in the medical or surgical management of patients with a retained foreign body.
Keywords
Imaging of foreign body; Retained foreign body; Emergency radiology; Trichobezoar with intussusception; Scalpel in pleura; Handle shower in rectum; Gun shot injury; Air way foreign body
Imaging of foreign body articles, Retained foreign body articles, Emergency radiology articles, Trichobezoar with intussusception articles, Scalpel in pleura articles, Handle shower in rectum articles, Gun shot injury articles, Air way foreign body articles
Imaging of foreign body articles Imaging of foreign body Research articles Imaging of foreign body review articles Imaging of foreign body PubMed articles Imaging of foreign body PubMed Central articles Imaging of foreign body 2023 articles Imaging of foreign body 2024 articles Imaging of foreign body Scopus articles Imaging of foreign body impact factor journals Imaging of foreign body Scopus journals Imaging of foreign body PubMed journals Imaging of foreign body medical journals Imaging of foreign body free journals Imaging of foreign body best journals Imaging of foreign body top journals Imaging of foreign body free medical journals Imaging of foreign body famous journals Imaging of foreign body Google Scholar indexed journals Retained foreign body articles Retained foreign body Research articles Retained foreign body review articles Retained foreign body PubMed articles Retained foreign body PubMed Central articles Retained foreign body 2023 articles Retained foreign body 2024 articles Retained foreign body Scopus articles Retained foreign body impact factor journals Retained foreign body Scopus journals Retained foreign body PubMed journals Retained foreign body medical journals Retained foreign body free journals Retained foreign body best journals Retained foreign body top journals Retained foreign body free medical journals Retained foreign body famous journals Retained foreign body Google Scholar indexed journals Emergency radiology articles Emergency radiology Research articles Emergency radiology review articles Emergency radiology PubMed articles Emergency radiology PubMed Central articles Emergency radiology 2023 articles Emergency radiology 2024 articles Emergency radiology Scopus articles Emergency radiology impact factor journals Emergency radiology Scopus journals Emergency radiology PubMed journals Emergency radiology medical journals Emergency radiology free journals Emergency radiology best journals Emergency radiology top journals Emergency radiology free medical journals Emergency radiology famous journals Emergency radiology Google Scholar indexed journals imaging articles imaging Research articles imaging review articles imaging PubMed articles imaging PubMed Central articles imaging 2023 articles imaging 2024 articles imaging Scopus articles imaging impact factor journals imaging Scopus journals imaging PubMed journals imaging medical journals imaging free journals imaging best journals imaging top journals imaging free medical journals imaging famous journals imaging Google Scholar indexed journals Ultrasonography articles Ultrasonography Research articles Ultrasonography review articles Ultrasonography PubMed articles Ultrasonography PubMed Central articles Ultrasonography 2023 articles Ultrasonography 2024 articles Ultrasonography Scopus articles Ultrasonography impact factor journals Ultrasonography Scopus journals Ultrasonography PubMed journals Ultrasonography medical journals Ultrasonography free journals Ultrasonography best journals Ultrasonography top journals Ultrasonography free medical journals Ultrasonography famous journals Ultrasonography Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals laparoscopy articles laparoscopy Research articles laparoscopy review articles laparoscopy PubMed articles laparoscopy PubMed Central articles laparoscopy 2023 articles laparoscopy 2024 articles laparoscopy Scopus articles laparoscopy impact factor journals laparoscopy Scopus journals laparoscopy PubMed journals laparoscopy medical journals laparoscopy free journals laparoscopy best journals laparoscopy top journals laparoscopy free medical journals laparoscopy famous journals laparoscopy Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Trichobezoar with intussusception articles Trichobezoar with intussusception Research articles Trichobezoar with intussusception review articles Trichobezoar with intussusception PubMed articles Trichobezoar with intussusception PubMed Central articles Trichobezoar with intussusception 2023 articles Trichobezoar with intussusception 2024 articles Trichobezoar with intussusception Scopus articles Trichobezoar with intussusception impact factor journals Trichobezoar with intussusception Scopus journals Trichobezoar with intussusception PubMed journals Trichobezoar with intussusception medical journals Trichobezoar with intussusception free journals Trichobezoar with intussusception best journals Trichobezoar with intussusception top journals Trichobezoar with intussusception free medical journals Trichobezoar with intussusception famous journals Trichobezoar with intussusception Google Scholar indexed journals Scalpel in pleura articles Scalpel in pleura Research articles Scalpel in pleura review articles Scalpel in pleura PubMed articles Scalpel in pleura PubMed Central articles Scalpel in pleura 2023 articles Scalpel in pleura 2024 articles Scalpel in pleura Scopus articles Scalpel in pleura impact factor journals Scalpel in pleura Scopus journals Scalpel in pleura PubMed journals Scalpel in pleura medical journals Scalpel in pleura free journals Scalpel in pleura best journals Scalpel in pleura top journals Scalpel in pleura free medical journals Scalpel in pleura famous journals Scalpel in pleura Google Scholar indexed journals
Article Details
1.Introduction
Foreign bodies are external objects lying within the human body, which are placed voluntarily or involuntarily. Aspiration, ingestion, self-insertion, trauma (particularly penetrating trauma), and iatrogenic placement are the multiple ways reported in the literature, to reach various locations of the human body. The most retained foreign bodies consist of voluntarily placed external objects including the catheters, intravascular coils, implants, prosthesis, stents, grafts, pacemakers, orthopedic nails or wires, and hemostatic sponges, where-as children are the most reported vulnerable group for involuntary foreign body insertion. The presentation of the subjects varies based on the nature of the object retained, the patients with airway foreign body will seek immediate emergency services, subjects with retained self-insertion of objects with sexual intention may present with a delayed course of time and embarrassment; where-as asymptomatic body packers may be brought by the police guards for a body checkup. Of course, the medical devices left in the body with beneficial intention may be followed for their functioning, or to assess the complications if any arises in the course of follow-up, while the unintentional medical foreign bodies will invite medico-legal notices to the physician. Radiological investigation plays a crucial role in identification, localization, characterization, and reporting the complication of the retained foreign bodies, and in many scenarios, radiological investigations may expose the unsuspected or concealed foreign bodies in the human body. Radiography identify the high attenuation objects readily, where-as ultrasonography can identify the wooden and glass objects at accessible sites. Computed tomography clearly characterizes most of the objects with accurate localization and also provides information regarding the secondary effects resulted from it, and also, with the possibility of multiple windowing facilities and multiplanar reconstruction, CT scan plays a superior role in the evaluation of foreign bodies. Magnetic resonance imaging (MRI) is limited to evaluate the the MRI compatible foreign bodies especially like wooden material, glass, or textiloma (gossypiboma). In this article, imaging features of six different cases with the retained foreign bodies in the pleural cavity (unintentional iatrogenic), recto-sigmoid colon (auto-erotism), complicated trichobezoar (psychiatric issue), a bullet in the neck (penetrating trauma), needle breakage (IV drug abuse) and air-way (accidental aspiration), who reported to the emergency radiological services are reported along with their management.
2. Case Series
2.1 Case 1
A 60-year-old chronic smoker patient presented with a history of breathlessness for 1 week. There was associated fever and cough present. The breathlessness was gradual with maintained blood pressure and arterial saturation. On examination increased respiratory rate (28/minute) and orthopnea noted. The chest radiograph suggested pneumothorax right side. Because of dyspnea, a chest tube was inserted in 5th intercostal space; however, the patient's condition deteriorated in a few hours even after supplementation of 50% oxygen via nasal cannula. Non-contrast CT chest was done immediately, which revealed a metallic object with streak artifact along the pericardial pleural reflection at 9th dorsal vertebra (right para-vertebral location). The metallic object was difficult to characterize on an axial scan, on close inspection of CT scanogram, a metallic foreign body (scalpel) was identified, and the same was confidently visualized on CT volume rendered images (Figure 1). A chest tube was seen coursing through the right lung parenchyma with its tip mal-positioned into the right lower lung parenchyma. Mild pleural effusion (+15HU) was seen right side. The background lungs showed diffuse emphysematous changes. Mild subcutaneous emphysematous changes also noted at the chest tube insertion site. The patient was immediately referred to the cardiothoracic department. Urgent thoracoscopy was done under general anesthesia with subsequent videoscope assisted removal of the foreign body through grasper. The post-operative period was uneventful and the patient was further managed successfully for pneumonia and discharged home later.
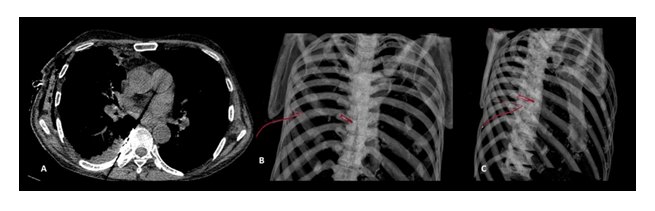
Figure 1: Non-contrast CT chest imaging of 60-year-old male patient revealing metallic object with streak artefacts at right paravertebral space on axial scan (A), volume rendering coronal (B) and oblique (C) images showing blade in right paravertebral space, and a chest tube entering into thoracic cavity.
2.2 Case 2
A 32-year-old, married, male, presented with a history of abdominal pain, obstipation, and abdominal distension for 2 days. On detailed probing of history, he revealed concealment of toilet shower handle (train toilet) insertion through anorectal path 2 days back, which he was unable to retrieve. The patient admitted his bisexual desires. Abdominal examination revealed tenderness with guarding, on auscultation hyper-peristaltic bowel sounds were heard. The rest of the systemic examination was normal and vital signs were stable. Immediate X-ray was taken, and it showed 12 cm radio-opaque foreign body in the recto-sigmoid region. Abdominal sonography revealed the presence of a foreign body in the pelvis with posterior acoustic shadowing and free fluid in the abdomen.
Further CT abdomen was advised to know the exact size, shape, and any associated complications. Non-contrast CT abdomen demonstrated hyperdense metallic foreign body conformation consistent with shower handle in the recto-sigmoid colon (Figure 2). There was no direct breach in the bowel wall and no pneumo-peritoneum. Rectal examination revealed patent sphincters with visualization of the lower end of a shower at anus opening. Intraoperatively, the rectosigmoid wall was gangrenous, segmental resection of the rectosigmoid colon with the removal of metallic foreign body was achieved with a subsequent ileostomy. The postoperative period was uneventful. The patient was counseled for bowel re-anastomosis at a later date and was educated about healthy sexual practices.
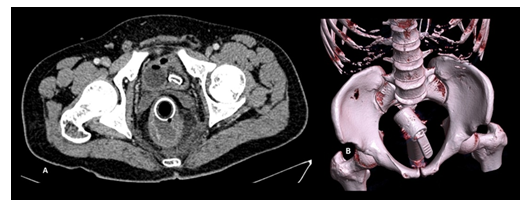
Figure 2: A 32-year-old, male with self-insertion of shower handle into the rectum, axial contrast-enhanced pelvic sections (A) showing a round hollow metallic object and its handle in bowel lumen, with thickening and stratification of the recto-sigmoid colon with soft tissue streaking in mesorectal space (A) and volume rendering oblique image showing shower handle in pelvic cavity (B).
2.3 Case 3
A 28-year-old primigravida with 32 weeks of gestation presented with vague abdominal pain, multiple episodes of vomiting, and constipation for 3 days. She denied a history of fever, vaginal discharge, or blurring of vision. Vitals were stable. On examination, the abdomen was firm and nontender with gravid uterus limiting the further clinical evaluation. There was mild pallor noted. Antenatal ultrasound was advised for fetal well-being along with maternal abdominal sonographic evaluation. On Ultrasound, most of the abdomen was obscured by the gravid uterus, and a live single fetus was seen. The stomach and a few bowel loops in the left iliac fossa were dilated and showed the presence of intraluminal echogenic contents which could not be ascertained any significance at the time of sonography, a few small bowel loops were also seen showing gross mural edematous changes. Her condition was progressively deteriorated; after a day of admission, she developed uterine contractions with the expulsion of a stillborn fetus. The patient persistently complained of abdominal distension and non-passage of stools. Postpartum bedside abdominal radiograph revealed abnormal bowel shadows and dilated segments at places with mottled lucency at the gastric shadow. CECT abdomen with intravenous and oral contrast examination was considered for further evaluation, which revealed intragastric (intraluminal) well defined heterogeneous mass with entrapment of food debris and air. Similar masses were seen in small bowel loops in the left abdomen (ileum). There was associated long segment duodenojejunal and jejuno-jejunal intussusception with edematous thickening of involved bowel walls and small bowel obstruction (Figure 3). The large bowel loops were collapsed and there was no pneumoperitoneum. Findings were suggestive of bezoar with associated long segment small bowel intussusception. The history of trichotillomania was confirmed by the patient's mother. The patient was taken up for surgery, an exploratory laparotomy was done, intussusception was identified and the visualized jejunal loops were unhealthy. The resection of the jejunal loops was done with the extraction of intragastric and small bowel contents, and subsequent end to end jejuno-jejunal anastomosis was done. On examination, trichobezoar was confirmed. The post-operative period was uneventful, the patient was referred to the psychiatry department for the treatment of trichophagia.
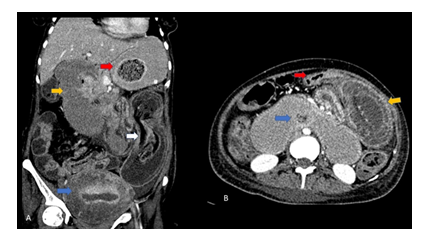
Figure 3: A 28-year-old, pregnant subject presented with intestinal obstruction and spontaneous expulsion of the fetus. The Contrast enhanced CT coronal reformation (A) showing an intragastric well-circumscribed in-homogenous mass consisting of ‘mottled gas pattern’ (red arrow) suggestive of Trichobezoar, with dilated duodenum (yellow arrow), jejuno-jejunal intussusception ( white arrow) and bulky & heterogenous uterus consistent with post-partum status (blue arrow). Axial CECT (B) showing presence of collapsed jejunal segment within the dilated duodenal loop (blue arrow) and bowel within bowel with significantly edematous jejunal bowel loops as well as mesentery within the lumen (yellow arrow) suggestive of long segment duodenojejunal and jejuno-jejunal intussusception, and collapsed ileal loop (red arrow).
2.4 Case 4
A 28-year-old patient presented with alleged firearm injury to the right neck. Entry wound with palpable crackles noted in the anterior lower neck and no exit was found. Vital signs were stable. The patient denied any history of loss of consciousness, respiratory difficulty, and hematemesis after gun-shot injury. NCCT neck with subsequent CT angiography of neck and brain was considered, which revealed a bullet in right para-vertebral space at non-fractured 6th dorsal (D6) vertebra (Figure 4). The right carotid and jugular vessels were away from the bullet, and the extracranial and intracranial course of the carotid arteries showed normal caliber and contrast opacification. Soft tissue tract with scattered air foci seen along the bullet trajectory path. No injury to the airway or esophagus was seen. Local exploratory dissection was done and a bullet was removed. The postoperative period was uneventful and the patient was discharged after 5 days.
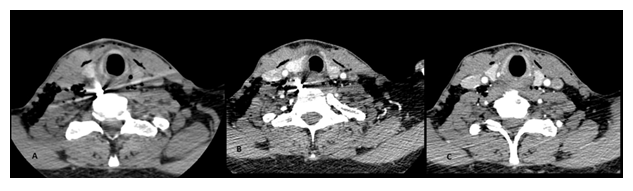
Figure 4: An adult male presented with fire arm injury to the right neck underwent CT neck examination (plain CT followed by neck angiography). Axial image of non-contrast CT (4A) revealing a high density metallic object within the right prevertebral space with surrounding mild hematoma at C6 vertebra, and subsequent neck angiography showing anterolateral location of the right great vessels of neck (4B), and normal contrast opacification of right carotid and vertebral arteries cephalad to the C5 vertebra (4C).
2.5 Case 5
A 30-year-old, male presented to the trauma center with a history of chronic intravenous drug abuse, presently being anxious about the needle breakage in the right inguinal region after intravenous shot of morphine. On local examination, a needle was not visible outside, there were multiple small punctate marks seen on the right groin suggestive of multiple needle pricks. On palpation asymmetrical swelling noted in the right groin, the needle could not be palpated. The right lower limb arterial pulse was palpable, with no edematous changes seen in the right foot and no neurological deficits documented. Sonological evaluation was requested as an initial evaluation of the right groin swelling, which revealed the presence of linear echogenic content in the groin region with surrounding heterogeneous echotexture. On doppler evaluation, the right lower limb arterial tree showed normal luminal caliber, color uptake, and spectral waveforms. The right femoral venous system was attenuated with few echogenic intraluminal contents that were seen suggestive of thrombosis. The tip of the needle could not be localized with certainty.
Further, lower limb CT angiography was considered, which revealed horizontally traversing metal foreign body in the right groin with partial extension into the proximal part superficial femoral vein with resultant venous attenuation (Figure 5). There was surrounding abnormal soft tissue haziness and fat streaking suggestive of inflammatory changes. A foreign body was retrieved on local surgical exploration without any complication. The patient was referred to the rehabilitation Centre.
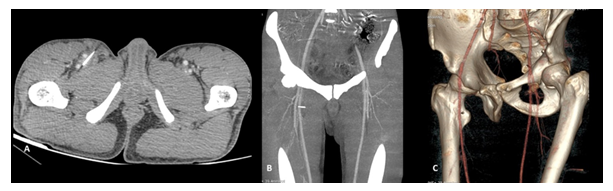
Figure 5: A young adult-male drug abuser presented to emergency services with history needle breakage while injecting recreation drug on right groin, axial sections of CT angiography of the lower limbs showing presence of linear metallic object in the subcutaneous location of right groin with its tip external to the superficial and deep femoral arteries (A), coronal MIP reconstruction (B) and oblique volume rendered images (C) revealing broken needle coursing between the right superficial and deep femoral arteries.
2.6 Case 6
A 2-year-old boy was brought to pediatric emergency services with a referral slip describing the condition as unresolved pneumonia for 4 days and worsening oxygen saturation since morning. The child was showing labored breathing and decreased breath sounds heard on auscultation right side and the pulse oximetry showed decreased oxygen saturation (~85%). Condition of the child deterioration suddenly and saturation did not improve with oxygen nasal supplementation, and immediate intubation was done. Despite the intubated status, the child became cyanotic and the heart rate was reduced. After a few minutes, the child threw 2 episodes of seizures. The child was immediately rushed into the CT room, and a non-contrast CT head and chest were acquired. NCCT head revealed symmetrical bilateral cerebral hypodensity with relatively high/ maintained attenuation of the cerebellum, suggestive of global cerebral ischemia with "white cerebellum sign" (Figure 6). The examination of the chest CT in the lung window showed the presence of soft-tissue attenuation content plugging the carina and straddling along the proximal right main bronchus (Figure 6). There was no hyperinflation of the lung was seen suggestive of near-complete tracheal occlusion with resultant acute severe cerebral ischemic injury. Immediately, the child was taken up for bronchoscopic retrieval of the tracheal foreign body, which was completed successfully with the removal of organic material. The ventilation and cardiovascular status of the child were improved, however, neurological deficits persisted at the time of discharge, and was referred to a pediatric neurologist follow up (Table 1).
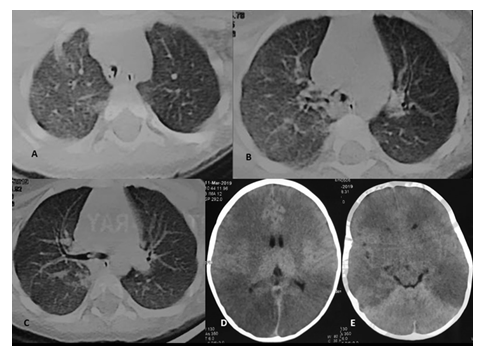
Figure 6: A 2-year-old, male child with history of aspiration of almond nut and respiratory distress and altered sensorium after intubation of child, NCCT chest and head was acquired immediately, lung window axial cuts showing lumen of endotracheal tube above the level of carina (A), soft tissue attenuation foreign body at carina (B) straddling into the right main bronchus (C). NCCT axial cuts of brain demonstrating diffuse, symmetrical, bilateral hypodensity at supratentorial section (D) and white cerebellum sign at infratentorial axial section (E) suggestive of acute profound cerebral ischemia.
Abbervations: NCCT: Non Contrast Computed Scan; US: Ultrasound; CTA: Computed Tomography Angiography; D9: Dorsal ninth vertebra; ICD: InterCostal Drainage;
VATS: Video Assisted Thoacoscopic Surgery
Table 1: Summary of the cases.
3. Discussion
Retained foreign bodies are reported in literature organized into sections pertaining to the specific location and intention with which the objects inserted into the body. No study describing the experience of the radiologist in the emergency unit has been described in literature till date, we report and discuss 6 different cases who presented to emergency services with acute presentation including intestinal obstruction, airway obstruction, and suspected vascular injury. The choice of imaging in the evaluation of the retained foreign bodies depends upon the clinical presentation and route of insertion. The imaging plays a pivotal role in accurate localization, characterization, and assessment of the secondary effects. Rapid assessment with radiography is the most widely radiological tool and may be sufficient in most of the scenarios, sonography with or without a doppler study is used for assessment of the accessible sites with suspected vascular injury by the retained foreign bodies. CT imaging takes a superior role by virtue of its multiple window alteration and multiplanar reconstruction capabilities, which aids in improving the conspicuity of the object, localization, and accurate assessment of the associated complications like inflammatory changes, obstruction, and perforation, active contrast extravasation and other serious issues. MRI is helpful in assessing brain and musculoskeletal foreign bodies in selected case scenarios. Rapid and accurate objective evaluation is the cornerstone in the management of emergency cases, and radiological investigation achieves that and further directs the clinical team for accurate medical or surgical management of the subjects with retained foreign bodies with the acute presentation. The specific clinical, imaging and management points pertaining to the above-described cases are described below.
Chest tube insertion is an essential skill employed in emergency services to manage pleural collections. The reported rate of complications related to chest insertion varies from 5 to 10% [1]. Pneumothorax, chest tube malposition, infection, chest tube kink, and dislodgement are common complications reported [2]. Foreign bodies in pleura have been rarely reported, scalpel displacement into the pleural cavity is a unique complication with only a few incidents to be reported literature. The pleural foreign body must be tried for removal even in asymptomatic cases, especially if the object is sharp, to avoid complications associated with further advancement of it into the mediastinum. However, a small, bunt, clean objects located in the periphery are well-tolerated usually and can be left behind if extraction is difficult [3, 4]. Sharp foreign bodies like a scalpel can easily pierce the visceral pleura causing direct injury to adjacent vital mediastinal structures viz. aorta, heart, coronary arteries, tracheobronchial tree, and esophagus. Imaging plays a vital role in describing the character, size, and shape of the foreign body and deciding the management protocol. X-ray is the initial investigation revealing pneumothorax, pleural effusion, or surgical emphysema. However, a few foreign bodies like glass pieces may be missed on a radiograph, and CT Chest better depicts the character, position, number, and also associated complications. In case of associated esophageal injury, there may be pneumo-mediastinum, pleural effusion, haemo-thorax, and pneumo-mediastinum as an indirect sign. Aortic injuries and associated hemorrhage are easily diagnosed with cross-section examination. Thus imaging helps in diagnosing the complications and thereby guiding the approach for management and prognosis in stable patients. Minimally invasive surgery is the treatment of choice, however, consent must be obtained for open thoracotomy in case needed for a difficult or complicated case. Surgery is done under general anesthesia either through videoscope (Video-Assisted Thoracoscopic Surgery) or open thoracotomy after collapsing the affected lung and inserting a PVC double-lumen tube [5].
The rectal foreign body is not an uncommon presentation in the ER with a recent increase in incidence [6]. It may be in the form of concealment (body packing), sexual auto-erotism as in our case, for a therapeutic purpose like constipation, accidental, or traumatic. Sexual autoerotism is the most common cause, although least reported [7]. Thus, it is prudent for clinicians to have a high degree of suspicion and take detailed history and examination for signs of perforation or obstruction requiring emergent surgical evaluation and treatment. Rectal examination to be performed only after the characterization of the foreign body and its location on imaging. Special care should be taken to examine the sphincteric patency. Variable material of rectal foreign bodies is reported including organic matter, plastics, rubber, vibrators, and dildos [8]. Plain radiograph of abdomen delineates shape, size, orientation, and site along with grave complication of the peritoneal breach, while sonography reveals the free fluid or other associated complications. CT abdomen and pelvis further confirm the exact location with the help of multiplanar reconstructions, and associated complications like bowel thickening, pneumoperitoneum, etc. The majority of rectal foreign bodies can be removed through a trans-anal approach if objects are small and blunt. Forceps and vacuum devices have also been used to retrieve the objects. In case of unsuccessful evacuation attempts, laparoscopy is advised under general anesthesia to remove the foreign body by gently milking it down the rectoanal region, if possible. The bowel resection and enteric diversion procedures are carried out if the gangrenous changes or bowel mural breach is encountered [8, 9]. Post evacuation flexible recto-sigmoidoscopy to be carried out to rule out the breach in recto-sigmoid wall and mucosa.
A bezoar is a mass of ingested material that gets trapped in the gastrointestinal tract. Bezoars can phytobezoars, Lacto-bezoars, or any indigestible material that is ingested [10]. Trichobezoar is the most common type of bezoar and is made up of human hair and found in the stomach [11]. Trichophagia is seen almost exclusively in young aged females with psychiatric issues [12]. Continued hair ingestion leads to impaction in the gut, the intragastric acidic contents denature the hair protein and supply the bezoar its black color [13]. Decomposition and fermentation of fat in bezoar adds to the peculiar odor, and affect the person's breath [14]. Mostly, trichobezoars limits to stomach but may extend into the small bowel and even colon called Rapunzel syndrome [15, 16]. As bezoars are seen in young females of the reproductive group, pregnancy may be associated requiring laparoscopic removal in emergency [17]. Imaging plays a key role in diagnosing the condition as it presents with vague symptoms. Xray abdomen may show the abnormal gas pattern. Ultrasound abdomen is the initial modality for suspecting the condition. There are intra-bowel masses/contents with intense shadowing seen (18). Differentiating bezoar from food debris is a must with "grimy shadowing" in later on ultrasound [19, 20]. Gastric outlet obstruction and gastric pneumatosis are serious complications. The cross-sectional examination helps to better delineate and characterize the bezoar. On CT, a cellular intraluminal mass with concentric whorls of different densities with enmeshed pockets of air in it resembling "compressed concentric jewelry" like appearance [19]. Complication includes perforation, peritonitis, intussusception, obstructive jaundice, protein-losing enteropathy, pancreatitis, and even death. Recent recommendation for bezoar treatment includes observation, dissolution, fragmentation, and laparotomy and gastrotomy [21]. Surgery is the mainstay of treatment. Gastric bezoars can be retrieved endoscopically or via multiple enterotomies however, it is imperative to do a radical exploration of the rest of the bowel. Other methods like a modified needle(bezotome) and a modified lithotripter (bezotriptor) have been successfully used. The affected person's psychological problems must be dealt with properly with annual follow up [22].
Gunshot injuries are commonly encountered in medico-legal cases in the ER. Morbidity and mortality of gunshot injuries depend on various factors like the type of firearm, type of bullet, projectile path, mechanism of injury, and associated complications. Patients with gun-shot injuries should get attention particularly for the examination of entry and exit wound sites. The entry wound is characterized by beveled edges and nearby track of gas, metal, and blood products. Clinical examination, analysis of drainage material from the chest tube, and examination of the chest radiograph will determine whether the patient needs a thoracotomy. Imaging plays a vital role in planning and prognostication of injury. Xray of the affected area must be ordered in two perpendicular axes. If a bullet is not visualized inside the body then exit wound must be inspected which may be far from entry wound and requires further imaging in stable patients but emergent exploration is advised in unstable patients. CT scan of the affected area helps in 3D reconstruction and volume rendering for better characterization of bullet and its track. Bullet fragments are also searched extensively due to the ricochet mechanism. Other associated vascular and non-vascular complications can also be easily diagnosed by CT angiography. Bullet wounds below the nipple line should raise suspicion of the diaphragm or abdominal injuries [23]. Laparotomy is required if peritoneal penetration is suspected [24, 25]. Only 15-20% of urban gunshot wounds to the chest require open thoracotomy [26]. Chest wounds are often treated adequately with tube thoracostomy, airway management, and blood transfusion. Whenever a bullet wound traverses the midline of the neck or mediastinum, perforation of the esophagus or aortic injury should be suspected [27]. DSA is sometimes used in case of vascular injury confirmation. MRI is mostly contraindicated in patients due to the ferromagnetic property of bullets or its fragment leading to further displacement and injury.
Intravenous (IV) drug users' injuries are commonly seen in the emergency department. Detailed history for needle breakage must always be sought due to grave complications of intravascular embolization. Also, complications like arterial injury, hemorrhage, or aneurysm may be associated. Thus foreign bodies must be removed at all costs. Imaging in stable patients confirms and delineates the foreign body along with any complication. Xray of the affected part is the initial investigation depicting radiopaque foreign bodies like needle or glass pieces. CECT examination better localizes the intravascular foreign body and associated vascular complication if any. DSA is both diagnostic as well as therapeutic in intravascular foreign body cases where it may be removed through endovascular intervention. However, if the foreign body has an extravascular component or associated thrombosis, an open explorative procedure must be followed (as in our case). There is an advantage of minimal invasiveness with a primary success rate of 90% [28]. Combined interventional repositioning and surgical extraction may be required in cases of large foreign bodies in noncritical vascular areas [29, 30].
Foreign body aspiration and ingestion are commonly encountered in children. There may be delayed in diagnosis due to inappropriate history, failure to articulate and vague symptoms like unexplained fever, cough, and stridor leading to an increase in complications with time [31]. Clinical investigation in the form of detailed history taking, thorough physical examination, and stabilization of patients is the primary role in decision making for further management. Imaging plays a secondary role though must be followed in a stable patient [32]. Foreign bodies inhaled are usually nuts, small toys, wood pieces, or cork. The most commonly ingested foreign body is the coin. It is important to recognize the proper location of the coin in the esophagus or trachea. Sudden onset breathlessness with stridor indicates upper laryngeal obstruction and obviates immediate removal by various maneuvers or endoscopically. Chest radiography-AP Chest Xray (including neck and abdomen) is the initial and main diagnostic tool followed by NCCT Chest in unclear or complicated cases. However, it is to be kept in mind that only 10% of foreign bodies are radioopaque. Chest Xray (AP and Lateral views) completely delineates the end on and in profile appearance of the coin. If a foreign body is small, it passes below the trachea into lower respiratory tracts where they may remain asymptomatic and invisible on Chest Xray/CT but asymmetric obstruction may show secondary imaging signs in form of ipsilateral hyper-inflation, increased lung volume due to air trapping. Further infection or impaction may lead to other symptoms like unexplained fever, cough, or weight-loss [33]. Chest Xray in the expiratory phase better contrasts the asymmetric translucency. A retained foreign body may cause atelectasis, mediastinal shift, and consolidation [34]. Flexible bronchoscopy has been considered a safe and efficient tool in the extraction of tracheal foreign bodies in children [35]. The organic foreign body must be crumped by forceps and extracted followed by washing and irrigation of bronchial trees. Small pieces and secretions must be suctioned out [36]. Airway obstruction causing acute hypoxic injury may lead to global cerebral ischemia. NCCT head screening in suspicious cases must be done immediately for early intervention and prevention of complications.
4. Conclusion
Imaging plays a crucial role in the evaluation of the retained foreign bodies, the localization and characterization of the foreign bodies with their associated imaging features help in triage and accurate management of the patients in the emergency department. With adequate history and clinical examination, it is essential to carry out the most suitable imaging evaluation to answer the clinical queries and manage the case rapidly, especially when patients present with altered sensorium, intestinal obstruction, or airway occlusion to the emergency radiological services. This article illustrates our experience with the myriad of retained foreign body cases we encountered and helps the practicing radiologists to be familiar with the imaging features and complications of retained foreign bodies.
Financial Disclosure
None.
Conflicts of Interests
None.
Acknowledgements
None.
Sources of support
None.
References
- Mao M, Hughes R, Papadimos TJ, et al. Complications of chest tubes: A focused clinical synopsis. Curr Opin Pulm Med 21 (2015): 376-386.
- Collop NA, Kim S, Sahn SA. Analysis of tube thoracostomy performed by pulmonologists at a teaching hospital. Chest 112 (1997): 709-713.
- Brewer III LA. Wounds of the chest in war and peace, 1943-1958. Ann Thorac Surg 7 (1969): 387-408.
- Brewer III LA, Mulder GA. Trauma to the chest. In Ed.: Shields TW. General Thoracic Surgery. Lea and Febiger, Philadelphia, PA (1972): 90.
- Weissberg D, Weissberg-Kasav D. Foreign bodies in pleura and chest wall. Ann Thorac Surg 86 (2008): 958-961.
- Kurer MA, Davey C, Khan S, et al. Colorectal foreign bodies: a systematic review. Colorectal Dis 12 (2010): 851-861.
- Koomstra JJ, Weersma RK. Management of rectal foreign bodies: Description of a new technique and clinical practice guidelines. World J Gastroenterol 14 (2008): 4403-4406.
- Akhtar MA, Arora PK. Case of unusual foreign body in rectum. Saudi J Gastroenterol 15 (2009): 131-132.
- Singaporewalla RM, Tan DEL, Tan TK. Use of endoscopic snare to extract a large rectosigmoid foreign body with review of literature. Surg Lapaprosc Endosc Percutan Tech 17 (2007): 145-148.
- Goldberg JE, Steele SR. Rectal foreign bodies. Surg Clin N Am 90 (2010): 173-184.
- Carr JR, Sholevar EH, Baron DA. Trichotillomania and trichobezoar: a clinical practice insight with report of illustrative case. J Am Osteopath Assoc 106 (2006): 647-652.
- Sehgal VN, Srivastava G. Trichotillomania ± trichobezoar: revisited. J Eur Acad Dermatol Venereol 20 (2006): 911-915.
- Sharma V, Sahi RP, Misra NC. Gastro-intestinalbezoars. J Indian Med Assoc 89 (1991): 338-339.
- Sidhu BS, Singh G, Khanna S. Trichobezoar. J Indian Med Assoc 91 (1993): 100-101.
- Vaughan ED Jr, Sawyers JL, Scott HW Jr. The Rapunzel syndrome. An unusual complication of intestinal bezoar. Surgery 63 (1968): 339-343.
- Naik S, Gupta V, Rangole A, et al. Rapunzel syndrome reviewed and redefined. Dig Surg 24 (2007): 157-161.
- Meyer-Rochow GY, Grunewald B. Laparoscopic removal of a gastric trichobezoar in a pregnant woman. Surg Laparosc Endosc Percutan Tech 17 (2007): 129-132.
- Ahmad Z, Sharma A, Ahmed M, et al. Trichobezoar Causing Gastric Perforation: A Case Report. Iran J Med Sci 41 (2016): 67-70.
- Newman B, Girdany BR. Gastric trichobezoars: sonographic and computed tomographic appearance.Pediatr Radiol 20 (1990): 526-527.
- Kaushik NK, Sharma YP, Negi A, et al. Images- Gastric trichobezoar. Indian J Radiol Imaging 9 (1999): 137-139.
- Nirasawa Y, Mori T, Ito Y, et al. Laparoscopic removal of a large gastric trichobezoar. J Pediatr Surg 33 (1998): 663-665.
- Kishor Taori, Amol Deshmukh, Jawahar Rathod, et al. Rapunzel syndrome: A trichobezoar extending into the ileum. Appl Radiol (2008).
- Pery M, Rosenberger A, Kleinhaus U. Injuries of the abdomen. Acta Radiol Suppl (Stockh) 367 (1986): 65-72.
- Feliciano DV, Burch JM, Spjut-Patnnely V, et al. Abdominal gunshot wounds: an urban trauma center’s experience with 300 consecutive patients. Ann Surg 208 (1988): 362-370.
- Moore JB, Moore EE, Thompson JS. Abdominal injuries associated with penetrating trauma in the lower chest. Am J Surg 140 (1980): 724-730.
- Kish G, Kozloff L, Joseph WL, et al. Indicationsforearly thoracotorny in the management of chest trauma. Ann Thorac Surg 22 (1976): 23-28.
- Pass U, LeNarz LA, Schreiber JT, et al. Management of esophageal gunshot wounds. Ann Thorac Surg 44 (1987): 253-256.
- Surov A, Buerke M, John E, et al. Intravenous port catheter embolization: mechanisms, clinical features, and management. Angiology 59 (2008): 90-97.
- Wolf F, Schernthaner RE, Dirisamer A, et al. Endovascular management of lost or misplaced intravascular objects: experiences of 12 years. Cardiovascular and interventional radiology 31 (2008): 563-568.
- Karanikas ID, Polychronidis A, Vrachatis A, et al. Removal of knotted intravascular devices. Case report and review of the literature. European journal of vascular and endovascular surgery: the official journal of the European Society for Vascular Surgery 23 (2002): 189-194.
- Case 137: Pneumonia and bronchiectasis secondary to unrecognized peanut impaction. Torres de Amorim e Silva CJ, Fink AM Radiology 248 (2008): 1080-1082.
- Ruiz FE. Airway foreign bodies in children. In Ed.: Basow DS. Waltham, Mass (2013).
- Barretto RL, Holinger LD. In Eds.: Cummings CW, Flint PW, Harker LA, et al. Foreign bodies of the airway and esophagus.. Philadelphia: Elsevier Mosby (2005): 43-46.
- Mu LC, Sun DQ, He P. Radiological diagnosis of aspirated foreign bodies in children: review of 343 cases. J Laryngol Otol 104 (1990): 778-782.
- Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12,979 cases. Anesth Analg 111 (2010): 1016-1025.
- Oncel M, Sunam GS, Ceran Sam?. Tracheobronchial aspiration of foreign bodies and rigid bronchoscopy in children. Pediatrics International 54 (2012): 532-535.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
