Frequency of Confirmed Congenital Renal Malformations in Neonates with Antenatal Diagnosis of Renal Anomalies Presenting in Neonatal Intensive Care Unit of a Tertiary Care Setting of a Low Income Country
Article Information
Qurat-Ul-Ain Siddique1, Abid Ali Jamali2*, Sanober Fatima1, Jai Parkash3
1FCPS Resident, Department of Pediatric Medicine, National Institute of Child Health, Karachi, Pakistan
2Fellow PEM, Department of Emergency Medicine, Aga Khan University Hospital, Karachi, Pakistan
3Associate Professor, Head of Department of Neonatal Intensive Care Unit, National Institute of Child Health, Karachi, Pakistan
*Corresponding Author: Abid Ali Jamali, Fellow PEM, Department of Emergency Medicine, Aga Khan University Hospital, Karachi, Pakistan
Received: 29 January 2022; Accepted: 17 February 2022; Published: 8 March 2022
Citation:
Qurat-Ul-Ain Siddique, Abid Ali Jamali, Sanober Fatima, Jai Parkash. Frequency of Confirmed Congenital Renal Malformations in Neonates with Antenatal Diagnosis of Renal Anomalies Presenting in Neonatal Intensive Care Unit of a Tertiary Care Setting of a Low Income Country. Journal of Pediatrics, Perinatology and Child Health 6 (2022): 129-136.
View / Download Pdf Share at FacebookAbstract
Introduction: Approximately 20 to 30% of all anomalies identified in the prenatal period are congenital anomalies of the kidney and urinary tract (CAKUT). Widespread antenatal screening has resulted in increased detection of anomalies of the kidneys and urinary tract. There are limited studies on the postnatal confirmation of these antenatally detected renal malformations. Moreover, there is no local data available in this regard. So, we conducted the study so that we can obtain local data as well as we can plan management and prevention protocols for such chronically, and sometimes critically, ill neonates.
Materials and Methods: It was a cross-sectional study conducted at the neonatal intensive care unit (NICU) at the National Institute of Child Health, Karachi during 2017-2018. The sample size was 100 cases. The sampling technique was non-probability consecutive sampling. All neonates aged 1-28 days of either gender admitted in NICU with antenatal diagnosis of congenital renal anomalies on anomaly scan were included in the study. Preterm neonates (gestational age below 34 weeks) and neonates having siblings with similar congenital problems were excluded.
Results: The mean age of the neonates in our study was 10.17 ± 9.30 days and the mean gestational age at birth was 36.65 ± 1.16 weeks. The majority of the neonates, that is 65%, were males while 35% were females. Sixty-six per cent (66%) neonates were ≤10 days of age while 34% were >10 days of age. Fifty five% of the neonates were ≤36 weeks of gestation at birth while 45% were >36 weeks of gestation at birth. Frequency of postnatally confirmed congenital renal malformation was observed in 78 (78%) neonates. Neonates whose age at presentation was >10 days were slightly more likely to have confirmed congenital renal malformation as compared to neonates with ≤10 days of age, which is 85.3 % vs 74.2 % (p-value 0.
Keywords
Confirmed Congenital Renal Malformation; Antenatal Diagnosis; Neonatal Intensive Care Unit
Confirmed Congenital Renal Malfor-mation articles; Antenatal Diagnosis articles; Neonatal Intensive Care Unit articles
Article Details
1. Introduction
Kidney and/or lower urinary tract anomalies that are present at birth in a newborn are generally termed congenital renal malformations. Fetal kidneys can be visualized at 12 weeks, and by 25 weeks, the renal cortex and medulla are distinctly demonstrated on ultrasonography. Approximately 20 to 30% of all anomalies identified in the prenatal period are con-genital anomalies of the kidney and urinary tract (CAKUT). Congenital renal malformations can sometimes present in childhood or adulthood if not picked prenatally or in neonatal age [1]. Widespread antenatal screening has resulted in increased detec-tion of anomalies of the kidneys and urinary tract [2]. Currently majority of the congenital renal malfor-mations, including CAKUT, are detected antenatally with the use of high sensitivity fetal ultrasonography [3]. Gestational age based parameters for expected length (appropriate growth) are also available. In the prenatal period, congenital abnormalities of the kid-neys and urinary tract (CAKUT) are the most comm-on sonographically identified malformations. Obstru-ctive uropathies account for the majority of cases [4].
As compared to earlier scanning, mid-trimester ultra-sonographic scanning increases the detection rates of congenital renal malformations. Many of these urolo-gic abnormalities would manifest later in life as pye-lonephritis, hypertension or end-stage renal disease, if not detected by prenatal ultrasound and subseq-uently manage [5]. There are limited studies on the post-natal confirmation of antenatally detected renal malformations. It is suggested that sonographically detected antenatal renal abnormalities should be evaluated by a post-natal sonogram at 4–6 weeks of age and if the 6-week aged scan is normal then further evaluation can safely be limited. Congenital renal formations are among the most common cause of chronic kidney disease (CKD) in children. Although CKD occurs less often in children than adults, still children account for about 2% of all patients with ESRD [6]. Mild forms of congenital kidney disease that appear relatively benign during the childhood may progress to ESRD later in adult life [7]. Literature has shown that the incidence of confirmed congenital renal malformations is high among neonates who had an antenatal diagnosis of a renal anomaly during the fetal stage (inside the womb) [8-10]. But later study reported the frequency is little lower than previous which showed ambiguity that antenatal diagnosis might have flaws in diagnosis. Moreover, there is no local data available in this regard. So, we conducted the study so that we can gain local data as well as we can plan mana-gement and prevention protocols for such critically ill neonates.
2. Materials and Methods
It was a cross-sectional study conducted at the neonatal intensive care unit (NICU) at the National Institute of Child Health (NICH), Karachi during 2017-2018. The study was waived for ethical approval from the Ethical Review Committee (ERC) of NICH. The sample size of 100 cases is calculated with 95% confidence level, 8.5% margin of error and taking an expected percentage of confirm renal malformation i.e. 77.1% in neonates presenting with antenatal diagnosis of congenital renal anomalies admitted in NICU. The sampling technique was non- probability consecutive sampling. All neonates aged 1-28 days of either gender admitted in NICU with antenatal diagnosis of congenital renal ano-malies on anomaly scan were included in the study. Preterm neonates (gestational age below 34 weeks) and neonates having siblings with similar congenital problems were excluded.
2.1 Data collection procedure
Hundred neonates who fulfilled inclusion criteria were enrolled from the NICU of the National Institute of Child Health, Karachi. Informed consent and demographic details (name, age, and gender) were obtained. Then all neonates underwent renal ultrasonography by a single senior radiologist having 4 years of experience. If there was hypoplastic kidney, cystic dysplastic kidney, multicystic dyspl-astic kidney, aplastic, hydronephrosis or abnormally shaped bladders from midway prenatal compensatory hypertrophy on ultrasound, then congenital renal malformation was confirmed. All this information was recorded on predesigned Performa.
2.2 Data analysis
All data were entered and analyzed in SPSS version 20.0. The quantitative variables i.e. age and gesta-tional age at birth were presented in the form of mean ± standard deviation. The qualitative variable i.e. gender and confirm congenital renal malformation was presented in the form of frequency and per-centage. Data was stratified for gestational age at birth, age and gender. Chi- square was applied to compare stratified groups taking p-value≤0.05 as significant.
3. Results
The mean age of the neonates in our study was 10.17 ± 9.30 days and the mean gestational age at birth was 36.65 ± 1.16 weeks Table 1. The majority of the neonates, that is 65%, were males while 35% were females. Sixty-six per cent (66%) neonates were ≤10 days of age while 34% were >10 days of age. Regarding the gestational age of the neonates, we found that 55% of the neonates were ≤36 weeks of gestation at birth while 45% were >36 weeks of gestation at birth Table 2. The frequency of post-natally confirmed congenital renal malformation was observed in 78 (78%) neonates Figure 1. Neonates whose age at presentation was >10 days were slightly more likely to have confirmed congenital renal malformation as compared to neonates with ≤10 days of age, which is 85.3 % vs. 74.2 % (p-value 0.206). In our study males and females were found to have almost equal postnatally confirmed congenital renal malformations (78.5 % in males and 77.1% in females) (p-value 0.879). Postnatally confirmed congenital renal malformations were observed more commonly in neonates who were >36 weeks of gestational age (80%) as compared to those ≤36 weeks of gestational age (76.4%) (p-value 0.662) Table 3.
|
Variable |
Mean ± SD |
Minimum |
Maximum |
|
Age of the patients, days (n=100) |
10.17 ± 9.30 |
1 |
28 |
|
Gestational age at birth, weeks (n=100) |
36.65 ± 1.16 |
34 |
38 |
Table 1: Mean Age and Gestational Age at Birth of the Patients (n=100).
|
Gender |
|
|
Male |
65 |
|
Females |
35 |
|
Age |
|
|
≤ 10 days |
66 |
|
>10 days |
34 |
|
Gestational Age |
|
|
≤36 weeks |
55 |
|
>36 weeks |
45 |
Table 2: Demographic Factors of the Patients (n=100).
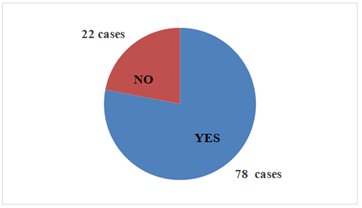
Figure 1: Confirm Congenital Renal Malformation.
|
Variables |
Confirm Congenital renal malformation |
Total |
p-value |
||
|
Yes |
No |
||||
|
Age |
≤10 days |
49 (74.2) |
17 (25.8) |
66 (100) |
0.206 |
|
>10 days |
29 (85.3) |
5 (14.7) |
34 (100) |
||
|
Total |
78 (78) |
22 (22) |
100 (100) |
||
|
Gender |
Male |
51 (78.5) |
14 (21.5) |
65 (100) |
0.879 |
|
Female |
27 (77.1) |
8 (22.9) |
35 (100) |
||
|
Total |
78 (78) |
22 (22) |
100 (100) |
||
|
gestational age |
≤36 weeks |
42 (76.4) |
13 (23.6) |
55 (100) |
0.662 |
|
>36 weeks |
36 (80) |
9 (20) |
45 (100) |
||
|
Total |
78 (78) |
22 (22) |
100 (100) |
||
Table 3: Comparison of Confirmed Congenital Renal Malformation With Respect to Age, Gender and Gestational Age (n=100).
4. Discussion
Among all sonographically detected antenatal mal-formations, congenital abnormalities of the kidneys and the urinary tract are the most common. Obstructive uropathies account for the majority of cases [4]. Renal tract malformations can be familial, and specific mutations of genes involved in renal tract development can sometimes be found in affected individuals [1]. Widespread antenatal screen-ing has resulted in increased detection of anomalies of the kidneys and urinary tract [2]. In most countries around the world, it has become a routine to get at least two ultrasonic examinations during pregnancy to monitor fetal development and identify any possible structural malformation. The diagnosis and prognosis of CAKUT have improved significantly in children secondary to gestational ultrasonography. Nowadays 80% to 90% of cases of obstructive uropathies can be detected by gestational ultrasono-graphy. The renal malformation detection sensitivity was observed up to 81.2% in a European study conducted in 12 countries [11]. Postnatal confir-mation of antenatally identified congenital renal malformations was observed in 78% of neonates. Our data is almost comparable to the study from India (Maharashtra) by Saha et al. where 77.1% of neonates admitted in NICU with a history of antenatal renal malformations were confirmed post-natally to have renal malformations on ultrasono-graphy [5]. Although a similar type of study conduted at Jeddah by Bondagji NS concluded that 90.1% of neonates admitted in NICU with a history of the antenatal renal anomaly on ultrasonography were confirmed to have renal malformations postnatally [12].
In our study males were predominantly affected as compared to female neonates with a male to female ratio of 1.8:1. Choi H A et al. also reported in their study that males were predominantly affected than females [13]. Most of the patients presented in NICU before 10th day of life and the mean age at presentation was 10.17 days (range 1-28 days). Gestational age was ranged from 34 to 38 weeks with a mean of 36.65 weeks. Sanghvi et al. also found nearly similar data pretending to the gestational age and they reported the mean 37.1 weeks gestational age at delivery (range 34—40 weeks) [14]. Studies show that the highest yield is obtained if an ultrasonic examination is performed in the third trimester of pregnancy. Positive predictive value (PPV) for APD values >7 mm in the third trimester 69% vs. 49% for APD > 4 mm in the second trimester [15]. Depending on the diagnostic criteria, fetal disease incidence varies from 1% to 5% of pregnancies. It is more frequent in boys (3 to 4/1) predominantly unilateral, and only 20% of cases will have postnatal clinical significance. Hydronephrosis classification as prop-osed by the SFU (based on the degree of pelvical-yceal dilation and parenchyma integrity), is another ultrasonographic finding that is important for the diagnosis and prognosis of children with CAKUT. This classification system was actually designed for post-natal scans but studies have shown that if applied properly to ante-natal scans, the children with grades 3 and 4 of hydronephrosis have an increased risk of the need for surgery and renal function deterioration [16].
Certain studies have shown that good gestational ultrasonography not only help in diagnosing congen-ital renal malformations antenatally but are also very helpful in determining the prognosis of children with CAKUT along with the anticipation of renal function deterioration, like (a) 1/3rd of the cases having single kidney were found to have associated CAKUT [17, 18], (b) the probability of CKD at 2 years of age is 15% when hydronephrosis is associated with other anomalies, as compared to only approximately 2% with isolated hydronephrosis [19], and (c) the risk of renal function deterioration is 9.4-fold higher in cases with bilateral hydronephrosis as compared to unilateral hydronphrosis [20]. We believe that, even with the methodological limitations of the reviewed studies, the suggestions can help pediatricians to establish clinical hypotheses for the early diagnosis of abnormalities of the genitourinary tract develop-ment, by using clinical data and information from the gestational ultrasonography, without resorting to expensive and invasive methods. We believe that the occurrence of any of the clinical signs and symptoms listed here should be considered as an indication to investigate the children regarding the possibility of CAKUT, as there is very limited prospective data to evaluate which of these findings are more important to identify the risk.
5. Conclusion
The frequency of confirmed congenital renal mal-formation was found higher in neonates presenting with antenatal diagnosis of renal anomalies presen-ting in the neonatal intensive care unit.
Declarations
Ethics approval
This study was waived for ethical approval from ethical review committee of National Institute of Child Health Karachi.
Consent for publication
Informed consent obtained from parents/guardians.
Accordance
All methods were performed in accordance with the relevant guidelines and regulations
Availability of data and materials
Most of the data generated or analyzed during this study are included in this article. Limited data can be provided in person on request to the main author.
Competing interests
The authors declare that they have no competing interests.
Funding
This study was not funded by any institution or organization.
Authors' contributions
QS was the main author who collected data from neonates’ parents/guardians and analyzed and interpreted that data. AJ was a major contributor in writing the manuscript along with study design. SF helped in collecting data and interpreting patient’s reports and ultrasounds. JP helped in study design and he supervised whole study i.e. from data collection to writing manuscript. All authors read and approved the final manuscript.
Acknowledgements
References
- Kerecuk L, Schreuder MF, Woolf AS. Renal tract malformations: perspectives for neph-rologists. Nat Clin Pract Neph 4 (2008): 312-325.
- Sinha A, Bagga A, Krishna A, et al. Revised guidelines on management of antenatal hydronephrosis. Indian pediatrics 50 (2013): 215-231.
- Livera LN, Brookfield DS, Egginton JA, et al. Antenatal ultrasonography to detect fetal renal abnormalities: a prospective screening programme. BMJ 298 (1989): 1421-1423
- Hindryckx A, De Catte L. Prenatal diagnosis of congenital renal and urinary tract malfor-mations. Facts, Views & Vision in ObGyn 3 (2011): 165-174.
- Saha A, Batra P, Chaturvedi P, et al. Antenatal detection of renal malformations. Indian Pediatr 46 (2009): 346.
- Warady BA, Chadha V. Chronic kidney disease in children: the global perspective. Pediatr Nephrol 22 (2007): 1999-2009
- Ingelfinger JR, Kalantar-Zadeh K, Schaefer F. World Kidney Day Steering Commit-tee. Averting the legacy of kidney disease: focus on Kidney Int 89 (2016): 512-518
- Gunn TR, Mora JD, Pease P. Antenatal diagnosis of urinary tract abnormalities by ultrasonography after 28 weeks' gestation: incidence and outcome. American journal of obstetrics and gynecology 172 (1995): 479-486.
- Hobbins JC, Grannum PA, Berkowitz RL, et al. Ultrasound in the diagnosis of congenital anomalies. American journal of obstetrics and gynecology 134 (1979): 331-345.
- Zerin JM, Ritchey ML, Chang AC. Incidental vesicoureteral reflux in neonates with antenatally detected hydronephrosis and other renal abnormalities. Radiology 187 (1993): 157-160.
- Wiesel A, Queisser-Luft A, Clementi M, et al. Prenatal detection of congenital renal malformations by fetal ultrasonographic examination: an analysis of 709,030 births in 12 European countries. Eur J Med Genet 48 (2005): 131-144.
- Bondagji NS. Antenatal diagnosis, prevalence and outcome of congenital anomalies of the kidney and urinary tract in Saudi Arabia. Urol Ann 6 (2014): 36-40.
- Choi H, Lee D, Shin S, et al. The Prenatal and Postnatal Incidence of Congenital Anomalies of the Kidneys and Urinary Tract (CAKUT) Detected by Ultrasound. Childhood Kidney Diseases 20 (2016): 29-32.
- Sanghvi K, Merchant R, Gondhalekar A, et al. Antenatal diagnosis of congenital renal malformations using ultrasound. Journal of Tropical Pediatrics 44 (1998): 235-240.
- Warady B, Chadha V. Chronic kidney disease in children: the global perspective. Pediatr Nephrol 22 (2007): 1999-2009.
- Timberlake MD, Herndon CD. Mild to moderate postnatal hydronephrosis grading systems and management. Nat Rev Urol 10 (2013): 649-656.
- Westland R, Schreuder MF, Ket JC, et al. Unilateral renal agenesis: a systematic review on associated anomalies and renal injury. Nephrol Dial Transplant 28 (2013): 1844-1855.
- Westland R, Schreuder MF, van Goudoever JB, et al. Clinical implications of the solitary functioning kidney. Clin J Am Soc Nephrol 9 (2014): 978-986.
- Quirino IG, Diniz JS, Bouzada MC, et al. Clinical course of 822 children with prenatally detected nephrouropathies. Clin J Am Soc Nephrol 7 (2012): 444-451.
- Quirino IG, Dias CS, Vasconcelos MA, et al. A predictive model of chronic kidney disease in patients with congenital anomalies of the kidney and urinary tract. Pediatr Nephrol 29 (2014): 2357-2364.


 Impact Factor: * 3.8
Impact Factor: * 3.8 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 