Glandular Odontogenic-The Multifaceted Cyst of the Jaw: An Unusal Case Report
Article Information
Jaya Singh1*, Shruti Singh2, Diksha Singh3, Shaleen Chandra4, Tanveer Fatima5, Manjit Kour5, Nikhil Gupta5
1Senior Resident, Department of Oral Pathology and Microbiology, King George’s Medical University, Lucknow, India
2Senior Resident, Department of Oral Pathology and Microbiology, King George’s Medical University, Lucknow, India
3Associate Professor, Department of Oral Pathology and Microbiology, King George’s Medical University, Lucknow, India
4Professor and Head, Department of Oral Pathology and Microbiology, King George’s Medical University, Lucknow, India
5Junior Resident, Department of Oral Pathology and Microbiology, King George’s Medical University, Lucknow, India
*Corresponding Author: Dr. Jaya Singh, Senior Resident, Department of Oral Pathology and Microbiology, King George’s Medical University, Lucknow, India
Received: 12 June 2020; Accepted: 17 June 2020; Published: 13 July 2020
Citation: Jaya Singh, Shruti Singh, Diksha Singh, Shaleen Chandra, Tanveer Fatima, Manjit Kour, Nikhil Gupta. Glandular Odontogenic-The Multifaceted Cyst of the Jaw: An Unusal Case Report. Archives of Clinical and Medical Case Reports 4 (2020): 682-689.
View / Download Pdf Share at FacebookAbstract
Glandular odontogenic cysts is one of the infrequent neoplasms seen in the oral cavity. They are developmental in origin with unpredictable and aggressive behavior. They are most commonly found in the anterior region of mandible having a predilection for the middle age group. These cysts have striking histologic features even though they have certain overlapping characteristics with other neoplasms. It is very important for us to cognize these unique differentiating features for a conclusive diagnosis. This paper reviews a case of Glandular odontogenic cyst which presented in our department and also elucidates the clinical, radiographical and histological criteria needed to diagnose the same.
Keywords
Glandular odontogenic; Multifaceted Cyst; Neoplasms
Glandular odontogenic articles, Multifaceted Cyst articles, Neoplasms articles
Glandular odontogenic articles Glandular odontogenic Research articles Glandular odontogenic review articles Glandular odontogenic PubMed articles Glandular odontogenic PubMed Central articles Glandular odontogenic 2023 articles Glandular odontogenic 2024 articles Glandular odontogenic Scopus articles Glandular odontogenic impact factor journals Glandular odontogenic Scopus journals Glandular odontogenic PubMed journals Glandular odontogenic medical journals Glandular odontogenic free journals Glandular odontogenic best journals Glandular odontogenic top journals Glandular odontogenic free medical journals Glandular odontogenic famous journals Glandular odontogenic Google Scholar indexed journals odontogenic articles odontogenic Research articles odontogenic review articles odontogenic PubMed articles odontogenic PubMed Central articles odontogenic 2023 articles odontogenic 2024 articles odontogenic Scopus articles odontogenic impact factor journals odontogenic Scopus journals odontogenic PubMed journals odontogenic medical journals odontogenic free journals odontogenic best journals odontogenic top journals odontogenic free medical journals odontogenic famous journals odontogenic Google Scholar indexed journals Multifaceted Cyst articles Multifaceted Cyst Research articles Multifaceted Cyst review articles Multifaceted Cyst PubMed articles Multifaceted Cyst PubMed Central articles Multifaceted Cyst 2023 articles Multifaceted Cyst 2024 articles Multifaceted Cyst Scopus articles Multifaceted Cyst impact factor journals Multifaceted Cyst Scopus journals Multifaceted Cyst PubMed journals Multifaceted Cyst medical journals Multifaceted Cyst free journals Multifaceted Cyst best journals Multifaceted Cyst top journals Multifaceted Cyst free medical journals Multifaceted Cyst famous journals Multifaceted Cyst Google Scholar indexed journals Neoplasms articles Neoplasms Research articles Neoplasms review articles Neoplasms PubMed articles Neoplasms PubMed Central articles Neoplasms 2023 articles Neoplasms 2024 articles Neoplasms Scopus articles Neoplasms impact factor journals Neoplasms Scopus journals Neoplasms PubMed journals Neoplasms medical journals Neoplasms free journals Neoplasms best journals Neoplasms top journals Neoplasms free medical journals Neoplasms famous journals Neoplasms Google Scholar indexed journals odontogenic epithelium articles odontogenic epithelium Research articles odontogenic epithelium review articles odontogenic epithelium PubMed articles odontogenic epithelium PubMed Central articles odontogenic epithelium 2023 articles odontogenic epithelium 2024 articles odontogenic epithelium Scopus articles odontogenic epithelium impact factor journals odontogenic epithelium Scopus journals odontogenic epithelium PubMed journals odontogenic epithelium medical journals odontogenic epithelium free journals odontogenic epithelium best journals odontogenic epithelium top journals odontogenic epithelium free medical journals odontogenic epithelium famous journals odontogenic epithelium Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Pathogenesis articles Pathogenesis Research articles Pathogenesis review articles Pathogenesis PubMed articles Pathogenesis PubMed Central articles Pathogenesis 2023 articles Pathogenesis 2024 articles Pathogenesis Scopus articles Pathogenesis impact factor journals Pathogenesis Scopus journals Pathogenesis PubMed journals Pathogenesis medical journals Pathogenesis free journals Pathogenesis best journals Pathogenesis top journals Pathogenesis free medical journals Pathogenesis famous journals Pathogenesis Google Scholar indexed journals epithelium articles epithelium Research articles epithelium review articles epithelium PubMed articles epithelium PubMed Central articles epithelium 2023 articles epithelium 2024 articles epithelium Scopus articles epithelium impact factor journals epithelium Scopus journals epithelium PubMed journals epithelium medical journals epithelium free journals epithelium best journals epithelium top journals epithelium free medical journals epithelium famous journals epithelium Google Scholar indexed journals
Article Details
1. Introduction
The cysts developing from the odontogenic epithelium are referred to as odontogenic cysts. It may be both developmental and inflammatory in origin. Glandular odontogenic cysts (GOC) are developmental in origin with aggressive nature. It is generally accepted to be odontogenic in nature, but it shows glandular and salivary features owing to its pluripotentiality [1]. GOC was first described as Sialo-odontogenic cyst by Padayachee and Van Wyk in 1987 [2]. It was further described as a distinct clinicopathological entity by Gardner et al in the year 1988 [3]. In the year 1992 GOC was put under the entity of a developmental odontogenic cyst by WHO. The term ‘polymorphous odontogenic cyst’ was given to GOC by High et al in 1996 owing to its aggressive behavior [4]. It appears as an asymptomatic swelling in the anterior mandibular region [1]. GOC can present as unilocular or multilocular well defined radiolucent lesions [5], also may sometimes have scalloped borders. GOC often gets misdiagnosed because of its overlapping features with other odontogenic cysts like lateral periodontal cyst (LPC) or botryoid cyst and central low-grade Mucoepidermoid carcinoma (CMEC) [6].
2. Case Report
A 19-year-old male reported with a chief complaint of a swelling in the left side of neck for 9 months. The swelling was slowly growing which gradually increased to the present size. The patient had no significant family and medical history. There was extraoral swelling seen in the left neck in the submandibular region and the lymph nodes were non-palpable. On extraoral examination the unilateral swelling was approximately 5.0 x 4.0 x 4.0 cm in size, of the same color as that of the skin (Figure 1a). On palpation, the lesion was non-tender and firm in consistency with regular smooth borders and no discharge on compression. No significant intraoral abnormalities were present (Figure 1b). The lesion was surgically excised and sent for histopathological examination. A provisional diagnosis of Ranula was given. The radiographic examination revealed a unilocular radiolucency extending from first mandibular molar to the developing third molar (Figure 2).
On gross examination, one soft tissue specimens were received collectively measuring 5.5x 3.5x 3 cm in size, grayish brown in color, irregular shape in surface and firm in consistency. There was a bluish cystic sac attached to soft tissue mass seemed to be filled with some cystic fluid. The cystic sac appeared bluish in color. The soft tissue specimen was sectioned into two halves and both the bits were kept for routine processing (Figure 3a and 3b). The histopathological examination reveals cystic area lined by pseudostratified ciliated columnar epithelium of varying thickness. Few areas showed stratified squamous epithelial lining. The superficial epithelial cells lining the cystic cavity were cuboidal in shape resembling hobnail cells. Few clear cells were also noted in the epithelium. The epithelial connective tissue interface was flat. The underlying connective tissue stroma was fibrous with regularly arranged collagen fiber bundles. Few blood vessels and inflammatory cells chiefly composed of neutrophils were seen too (Figure 4a-c).

Figure 1: 1a) Showing extraoral swelling in the left submandibular region; 1b) Showing normal intraoral findings.

Figure 2: Orthopantogram showing a unilocular radiolucency in the left angle of mandible region.
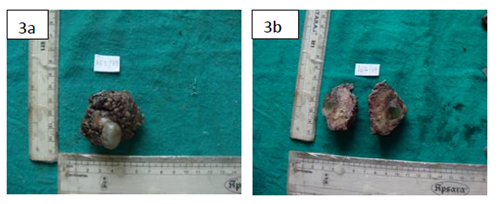
Figure 3: 3a) Showing the received gross specimen 3b) Showing the cut surface of the specimen.
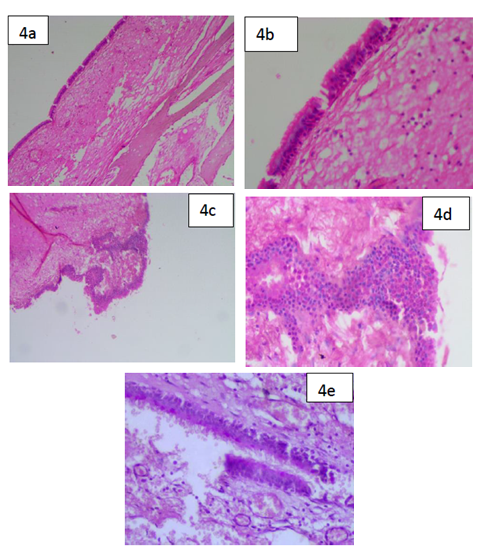
Figure 4: 4a) (H & E, ×4) Squamous epithelial lining with flat interface with the connective tissue; 4b) (H & E, ×10) Squamous epithelial lining with flat interface with the connective tissue showing microcystic spaces; 4c) (H & E, ×4) Cystic lining with epithelial plaques/theques; 4d) (H & E, ×40) Cystic lining with epithelial plaques/theques showing hobnail cells; 4e) (H & E, x10) PAS positive epithelial lining showing the presence of mucous producing cells.
3. Discussion
Glandular odontogenic cyst is an infrequent cyst of the jaw with less than 300 cases described till date. It has a slight male predilection, commonly seen in middle age group with an increased preponderance for the anterior lower jaw [7]. GOC is not a very common lesion with a recurrence rate of 21 % to 55%[8]. This high rate of recurrence can be attributed to the aggressive nature of the tumor [8]. Imaging analysis is helpful for the diagnosis of glandular odontogenic cyst, the locularity, radiodensity, and border characteristics of glandular odontogenic cyst are important in differentiating it with other odontogenic cysts [9]. Although, GOCs do not exhibit any striking clinical and radiographic features, their peculiar histopathologic features which should be analyzed in depth before diagnosing any such neoplasm [10]. Kaplan et al formulated a set of major and minor criterions for the diagnosis of GOC [11, 12]. They proposed that to conclude to a diagnosis all the major criteria should be fulfilled, and the minor ones may aid in the same.
Fowler et al did not think that all the major criteria needed to be met to conclude to a diagnosis. They set aside a set of 10 distinguishing features, out of which the presence of 7 features was said to conclude to a conclusive diagnosis [13]. They also proposed that the presence of five or less features could be mimicking GOC like cyst [13]. Due to overlapping clinical and histopathologic features, Glandular Odontogenic Cyst should be differentiated from Lateral Periodontal Cyst, Botryoid Odontogenic Cyst, low grade Central Mucoepidermoid Carcinoma and Dentigerous Cyst with mucous metaplasia to conclude to a definitive diagnosis [14].
|
Kaplan et al. [11, 12] |
|
|
Major Criteria |
Minor Criteria |
|
Squamous epithelial lining, with a flat interface with the connective tissue wall, lacking basal palisading |
Papillary proliferation of the lining epithelium |
|
Epithelium exhibiting variations in thickness along the cystic lining with or without epithelial ‘spheres’ or ‘whorls’ or focal luminal proliferation |
Ciliated cells |
|
Cuboidal eosinophilic cells or ‘hob-nail’ cells |
Multicystic or multiluminal architecture |
|
Mucous (goblet) cells with intraepithelial mucous pools, with or without crypts lined by mucous- producing cells. |
Clear or vacuolated cells in the basal or spinous layers. |
|
Intraepithelial glandular, microcystic or duct-like structures. |
|
Table 1: Major and Minor criteria laid down by Kaplan et al.
|
Fowler et al. [13] |
|
Surface eosinophilic cuboidal cells, also called “hobnail cells” |
|
Intraepithelial microcysts or duct-like spaces |
|
Apocrine snouting of hobnail cells |
|
Clear or vacuolated cells |
|
Variable thickness of the cyst lining |
|
Papillary projections or “tufting” into the cyst lumen |
|
Mucous goblet cells |
|
Epithelial spheres or plaque-like thickenings |
|
Cilia on the surface of eosinophilic cuboidal cells |
|
Multiple compartments |
Table 2: Diagnostic criteria laid down by Fowler et al.
|
Sl. No. |
Lesion |
Common Features |
Differentiating Features |
|
1 |
Lateral Periodontal Cyst |
1) Focal Epithelial Thickening 2) Glycogen rich epithelial cells |
1) Ciliated epithelium 2) Duct like spaces with mucous cells |
|
2 |
Botryoid Odontogenic Cyst |
1) Focal Epithelial Thickening 2) Glycogen rich epithelial cells |
1) Ciliated epithelium 2) Duct like spaces with mucous cells |
|
3 |
Low-grade Central Muco-epidermoid Carcinoma |
1) Mucous and Clear cells |
1) No Cellular atypia 2) Presence of Epithelial plaques |
|
4 |
Dentigerous cyst with mucous metaplasia |
1) Reduced enamel epithelium |
1) Ciliated epithelium 2) Presence of Epithelial plaques |
Table 3: Differential Diagnosis of Glandular Odontogenic Cyst.
The present case fulfills all the major criteria laid down by Kaplan et al and few of the minor criteria’s as well. It showed squamous epithelial lining of varied thickness with flat connective tissue interface, epithelial plaques, hobnail cells, goblet cells and intraepithelial microcystic spaces. It also exhibited areas of ciliated epithelium with vacuolated cells in the spinous layer. Due to similar features of GOC with the above-mentioned lesions, immunohistochemical evaluation might also aid in diagnosing this cyst. The epithelium of GOCs show strong positivity of cytokeratin 19 in the entire thickness of the epithelium confirming its odontogenic origin [15]. Ki 67 can aid in differentiating it from CMEC [12]. The immunohistochemical expression of Mammary Serine Protease Inhibitor (MASPIN) was seen significantly higher in CMEC than GOC [16]. Most cases of glandular odontogenic cyst have been treated by enucleation or curettage. However, this cyst shows a propensity for recurrence, which is observed in approximately 30% of all cases [1]. Treatment by enucleation or curettage might be the reason for high recurrence rate. The surgical treatment of large lesions should include enucleation with peripheral ostectomy for unilocular cases and marginal resection or partial jaw resection in multilocular cases [7, 17]. Follow-up should be continued for at least 3 years [6].
4. Conclusion
Dental surgeons could help better in diagnosing a lesion in the oral cavity with such diverse and overlapping features. Even though GOCs are rare with very low recurrence and good survival rate, these lesions also need timely and precise diagnosis. Understanding of the clinical presentation and specific diagnostic features will lead to early detection. This case report elucidates the importance of the histologic diagnosis of any neoplasm apart from their routine clinical and radiographic diagnosis. Also, how the differential diagnosis of a neoplasm plays a role in concluding to a diagnosis. Although GOC has low incidence and transform into malignancy rarely, owing to its aggressive behavior, a long-term follow up is advised.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/ their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
References
- Textbook of Oral and Maxillofacial Pathology. Neville 3rd Philadelphia: wb saunders company (2002).
- Padayachee A, Van Wyk CW.Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumor: sialo-odontogenic cyst? Journal of Oral Pathology 16 (1987): 499-504.
- Gardner DG, Kessler HP, Morency R, Schaner DL.The glandular odontogenic cyst: an apparent entity. Journal Oral Pathology 17 (1988): 359-366.
- High AS, Main DM, Khoo SP, et al. The polymorphous odontogenic cyst. Journal of Oral Pathology and Medicine 25 (1996): 25-31.
- Noffke C, Raubenheimer EJ. The glandular odontogenic cyst: clinical and radiological features; review of the literature and report of nine cases. Dentomaxillofacial Radiology 31 (2002): 333.
- Shah M, Kale H, Ranginwala A, Patel G. Glandular odontogenic cyst: A rare entity. Journal of Oral Maxillofacial Pathology 18 (2014): 89-92.
- Khadar Shaik, Vijay Reddy, Ramesh and Haripriya Chari. A case report of glandular odontogenic cyst of mandible. Oral Health and Care 3 (2018): 1-4.
- Kaplan I, Gal G, Anavi Y. Glandular odontogenic cyst: Treatment and Recurrence. Journal of Oral and Maxillofacial Surgery 63 (2005): 435-441.
- Ogura I, Tsuchimochi, Ono J, et al. Glandular odontogenic cyst: a report of four cases. Oral Science International 14 (2017): 43-49.
- Yanduri S, Deepa KK, Kumar BV, et al. Glandular odontogenic cyst: Analysis of clinicopathological features of five cases. Indian Journal of Oral Health Research 3 (2017): 40-4
- Kaplan I, Anavi Y, Hirshberg A. Glandular odontogenic cyst: A challenge in diagnosis and treatment. Oral Diseases 14 (2008): 575-581.
- Kaplan I, Anavi Y, Manor R, et al. The use of molecular markers as an aid in the diagnosis of glandular odontogenic cyst. Oral Oncology 41 (2005): 895-902.
- Fowler CB, Brannon RB, Kessler HP, et al. Glandular odontogenic cyst: Analysis of 46 cases with special emphasis on microscopic criteria for diagnosis. Head and Neck Pathology 5 (2011): 364-3
- Urs AB, Kumar P, Augustine J, et al. Glandular odontogenic cyst: Series of five cases. Journal of Oral and Maxillofacial Pathology 21 (2017): 239-243.
- Mascitti M, Santarelli A, Sabatucci A, et al. Glandular odontogenic cyst: Review of literature and report of a new case with cytokeratin-19 expression. Open Dent Journal 8 (2014): 1-12.
- Vered M, Allon I, Buchner A, et al. Is maspin immunolocalization a tool to differentiate central low-grade mucoepidermoid carcinoma from glandular odontogenic cyst? Acta Histochemistry 112 (2010): 161.
- Sharma J, Raina AB, Varshney A, et al. Glandular odontogenic cyst: An unusual entity. Indian Journal of Pathology and Microbiology 62 (2019): 345-346.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
