Hepatic Inflammatory Pseudotumor: Know It to Recognize It
Article Information
Viviana Congedo1, Adele Fornelli2, Laura Mastrangelo3, Giulia Bandini1, Andrea Domanico1, Esterita Accogli1*
1Ultrasound Diagnostic Centre, Medical Department, Maggiore Hospital, Bologna, Italy
2Pathological Anatomy Department, Maggiore Hospital, Bologna, Italy
3Surgical Department A, Maggiore Hospital, Bologna, Italy
*Corresponding Authors: Dr. Esterita Accogli, Ultrasound Diagnostic Centre, Medical Department, Maggiore Hospital, Bologna, Italy
Received: 31 January 2020; Accepted: 10 February 2020; Published: 10 March 2020
Citation: Viviana Congedo, Adele Fornelli, Laura Mastrangelo, Giulia Bandini, Andrea Domanico, Esterita Accogli. Hepatic Inflammatory Pseudotumor: Know It to Recognize It. Archives of Clinical and Medical Case Reports 4 (2020): 200-205.
View / Download Pdf Share at FacebookAbstract
Inflammatory pseudotumor of the liver (IPTL) is a rare benign lesion that can mimic hepatic malignant neoplasms. A 79-year-old woman, in follow-up care for a left breast cancer, was referred to our Ultrasound Diagnostic Centre for a hepatic mass of unknown nature, displayed on PET-CT, CT and Abdominal Ultrasonography (US). The patient presented with abdominal pain and low-grade fever, increased values of C-Reactive Protein (CRP) and gamma-glutamyl transpeptidase (γGT). Abdominal US confirmed the presence of a heterogeneous polycyclic mass 4.0 × 3.7 cm in size, sub-capsular, localized in the segment VI, isoechoic in arterial phase and hypoechoic in portal and late phase on contrast-enhanced ultrasound (CEUS). A liver biopsy revealed the presence of chronic inflammatory cells without evidence of malignancy. As the patient did not respond to medical therapy, she underwent hepatic segmentectomy and cholecystectomy. At histology, the specimen showed acute and chronic inflammation with xanthogranulomatous features.
Keywords
Hepatic Inflammatory Pseudotumor; Ultrasound; Ceus
Hepatic Inflammatory Pseudotumor articles, Ultrasound articles, Ceus articles
Hepatic Inflammatory Pseudotumor articles Hepatic Inflammatory Pseudotumor Research articles Hepatic Inflammatory Pseudotumor review articles Hepatic Inflammatory Pseudotumor PubMed articles Hepatic Inflammatory Pseudotumor PubMed Central articles Hepatic Inflammatory Pseudotumor 2023 articles Hepatic Inflammatory Pseudotumor 2024 articles Hepatic Inflammatory Pseudotumor Scopus articles Hepatic Inflammatory Pseudotumor impact factor journals Hepatic Inflammatory Pseudotumor Scopus journals Hepatic Inflammatory Pseudotumor PubMed journals Hepatic Inflammatory Pseudotumor medical journals Hepatic Inflammatory Pseudotumor free journals Hepatic Inflammatory Pseudotumor best journals Hepatic Inflammatory Pseudotumor top journals Hepatic Inflammatory Pseudotumor free medical journals Hepatic Inflammatory Pseudotumor famous journals Hepatic Inflammatory Pseudotumor Google Scholar indexed journals Pseudotumor articles Pseudotumor Research articles Pseudotumor review articles Pseudotumor PubMed articles Pseudotumor PubMed Central articles Pseudotumor 2023 articles Pseudotumor 2024 articles Pseudotumor Scopus articles Pseudotumor impact factor journals Pseudotumor Scopus journals Pseudotumor PubMed journals Pseudotumor medical journals Pseudotumor free journals Pseudotumor best journals Pseudotumor top journals Pseudotumor free medical journals Pseudotumor famous journals Pseudotumor Google Scholar indexed journals Hepatic Inflammatory articles Hepatic Inflammatory Research articles Hepatic Inflammatory review articles Hepatic Inflammatory PubMed articles Hepatic Inflammatory PubMed Central articles Hepatic Inflammatory 2023 articles Hepatic Inflammatory 2024 articles Hepatic Inflammatory Scopus articles Hepatic Inflammatory impact factor journals Hepatic Inflammatory Scopus journals Hepatic Inflammatory PubMed journals Hepatic Inflammatory medical journals Hepatic Inflammatory free journals Hepatic Inflammatory best journals Hepatic Inflammatory top journals Hepatic Inflammatory free medical journals Hepatic Inflammatory famous journals Hepatic Inflammatory Google Scholar indexed journals Ceus articles Ceus Research articles Ceus review articles Ceus PubMed articles Ceus PubMed Central articles Ceus 2023 articles Ceus 2024 articles Ceus Scopus articles Ceus impact factor journals Ceus Scopus journals Ceus PubMed journals Ceus medical journals Ceus free journals Ceus best journals Ceus top journals Ceus free medical journals Ceus famous journals Ceus Google Scholar indexed journals Scrotal ultrasound articles Scrotal ultrasound Research articles Scrotal ultrasound review articles Scrotal ultrasound PubMed articles Scrotal ultrasound PubMed Central articles Scrotal ultrasound 2023 articles Scrotal ultrasound 2024 articles Scrotal ultrasound Scopus articles Scrotal ultrasound impact factor journals Scrotal ultrasound Scopus journals Scrotal ultrasound PubMed journals Scrotal ultrasound medical journals Scrotal ultrasound free journals Scrotal ultrasound best journals Scrotal ultrasound top journals Scrotal ultrasound free medical journals Scrotal ultrasound famous journals Scrotal ultrasound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals ultrasound articles ultrasound Research articles ultrasound review articles ultrasound PubMed articles ultrasound PubMed Central articles ultrasound 2023 articles ultrasound 2024 articles ultrasound Scopus articles ultrasound impact factor journals ultrasound Scopus journals ultrasound PubMed journals ultrasound medical journals ultrasound free journals ultrasound best journals ultrasound top journals ultrasound free medical journals ultrasound famous journals ultrasound Google Scholar indexed journals myofibroblastic tumor articles myofibroblastic tumor Research articles myofibroblastic tumor review articles myofibroblastic tumor PubMed articles myofibroblastic tumor PubMed Central articles myofibroblastic tumor 2023 articles myofibroblastic tumor 2024 articles myofibroblastic tumor Scopus articles myofibroblastic tumor impact factor journals myofibroblastic tumor Scopus journals myofibroblastic tumor PubMed journals myofibroblastic tumor medical journals myofibroblastic tumor free journals myofibroblastic tumor best journals myofibroblastic tumor top journals myofibroblastic tumor free medical journals myofibroblastic tumor famous journals myofibroblastic tumor Google Scholar indexed journals tumor articles tumor Research articles tumor review articles tumor PubMed articles tumor PubMed Central articles tumor 2023 articles tumor 2024 articles tumor Scopus articles tumor impact factor journals tumor Scopus journals tumor PubMed journals tumor medical journals tumor free journals tumor best journals tumor top journals tumor free medical journals tumor famous journals tumor Google Scholar indexed journals Surgery articles Surgery Research articles Surgery review articles Surgery PubMed articles Surgery PubMed Central articles Surgery 2023 articles Surgery 2024 articles Surgery Scopus articles Surgery impact factor journals Surgery Scopus journals Surgery PubMed journals Surgery medical journals Surgery free journals Surgery best journals Surgery top journals Surgery free medical journals Surgery famous journals Surgery Google Scholar indexed journals
Article Details
1. Introduction
Inflammatory pseudotumor (IPT) is a rare benign condition which can mimic malignant tumors and is composed predominantly of inflammatory cells with variable amounts of fibrosis [1]. The most frequent site of involvement is the lung, but it can also occur in the liver and other organs [2]. IPTL has no specific clinical, radiologic, laboratory and histopathological findings, therefore an accurate differential diagnosis is essential to rule out other entities, such as inflammatory myofibroblastic tumor or sclerosing IgG4-related disease, and to plan treatment and to establish prognosis. Infectious and inflammatory causes, resulting for instance from rupture of the bile duct and extravasation of bile into the tissue, have been proposed, but in most of the cases etiology remains unknown3.
2. Case Report
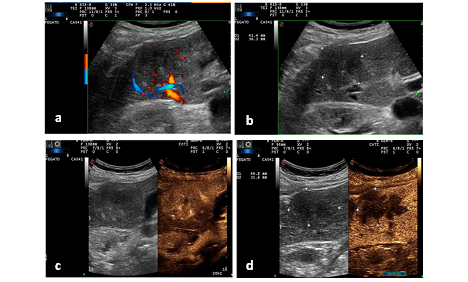
A 79-year-old woman presented to our Ultrasound Diagnostic Centre for an hepatic mass found on PET-CT, CT and Ultrasound Study (US), performed for recent onset of anorexia, low-grade fever and pain in the right hypochondrium. The patient was in follow-up care for a left breast cancer, treated at first with superior external quadrantectomy, and then with radical mastectomy and hormone therapy. Ten years later, a lymph node recurrence occurred and was treated with axillary node dissection. Before coming to our Centre, the patient performed PET-CT, US and CT that revealed the presence of a sub-capsular hepatic lesion in the segment VI and laboratory tests that revealed a γGT level fivefold greater than the upper cut-off, increased CRP (15 mg/dl) and negativity of tumor markers, hepatotropic viruses and autoimmunity markers. A first ultrasound-guided percutaneous liver biopsy was performed which histologically consisted of hepatic parenchyma with chronic inflammatory infiltrate, without evidence of malignancy. For the persistence of abdominal pain and worsening blood tests, the patient was referred to our Ultrasound Diagnostic Centre. The abdominal US confirmed the presence of a well-defined heterogeneous polycyclic mass, measuring 4.0 x 3.7 cm in size, sub-capsular, localized in the segment VI. CEUS was performed: the lesion appeared isoechoic in arterial phase, with wash-out in portal and late phase, suggestive also for secondary hepatic nodules (Figure 1).
We performed a second ultrasound-guided percutaneous liver biopsy that revealed hepatic parenchyma with fibrosis and chronic inflammation. Therefore, a medical therapy with antibiotic, steroid and nonsteroidal anti-inflammatory drugs (NSAIDs) was administered, with temporary clinical and laboratory success. For the re-occurrence of symptoms and for the inhaltered size and CEUS pattern of the lesion, the patient underwent surgical resection of the hepatic lesion (Figure 2) and cholecystectomy.
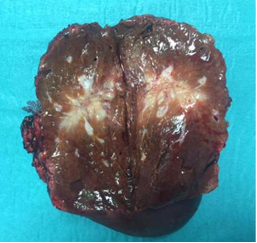
Figure 2: Surgical resection of hepatic lesion.
At macroscopic examination the lesion showed irregular margins and measured 4.5 cm in greatest axis. Histologically, multiple granulomas with central stellate suppurative necrosis, surrounded by palisading histiocytes and multinucleated giant cells, were present. These features were suggestive of infectious etiology, but histochemical stains (Silver, PAS, Giemsa and Zhiel Neelsen) failed to reveal any causative organism. The gallbladder showed features of chronic lithiasic cholecystitis.
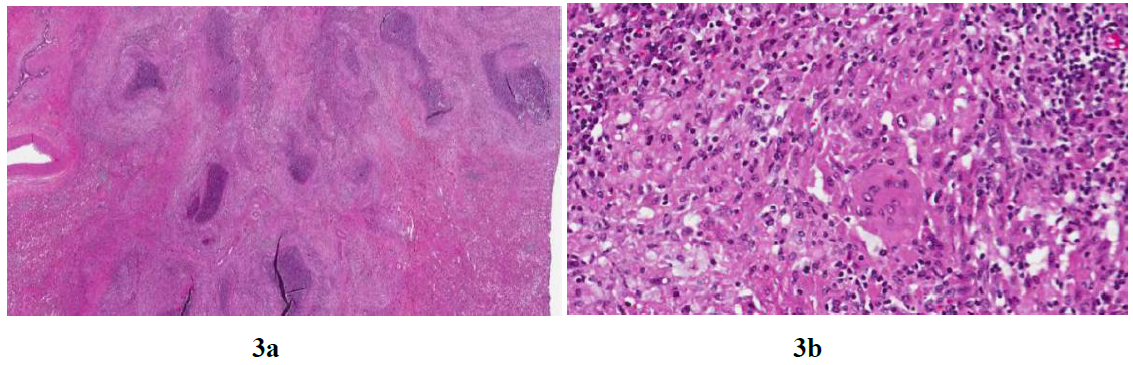
Figure 3: Histology of the surgical specimen. 3a The lesion is composed of multiple confluent granulomas with central suppurative necrosis (H&E, 20x). 3b At high power, the viable tissue is composed of lymphocytes, plasmacells and histiocytes, some of which are multinucleated (H&E, 200X).
3. Discussion
IPT is a rare benign condition which was first described in the lung in 1939 [4]. It is a mass-forming lesion of unknown etiology which is composed of acute and chronic inflammatory cells with various degree of fibrosis [5]. It can also occur in extra-pulmonary sites, including orbit, spleen, intestines, pancreas, liver, kidneys, urinary bladder, omentum, central nervous system, major salivary glands, larynx, ovaries, breasts, lymph nodes, skin and soft tissues [3, 6, 7]. Given the lack of uniform diagnostic criteria, the exact incidence of IPTL is unknown. Since its first description in 1953 by Pack and Backer [1], many other cases have been reported [7] some of them encompassing inflammatory myofibroblastic tumors which are true neoplastic lesions associated with anaplastic lymphoma kinase traslocation (ALK-1), that can recur and rarely metastasize [8].
According to Agaimy et al, IPTL mainly occurs in childhood and early adulthood, with a male-to-female ratio ranging from 1:1 to 3,5:1 [9] and it is more common in non-European populations [10]. Etiology is unknown, but a role is probably played by biliary obstruction, chronic cholangitis and primary sclerosing cholangitis [7, 11], gut infectious bacteria, such as actinomyces, bacteroides, Escherichia coli, Klebsiella, enterococcus, gram-positive cocci and beta-hemolytic streptococci, that provoke an inflammatory response, which sometimes decreases or completely resolves upon administration of antibiotics or NSADs [12, 13]. Other causes of IPTL could be vascular diseases, trauma and surgical-related infections and EBV-positive infection [1-14].
Recognition of IPTL is important because it can mimic hepatic malignancies, either primary (hepatocellular carcinoma and cholangiocarcinoma) or metastatic, and specific granulomatous lesions, such as sarcoidosis and tuberculosis. Correct diagnosis is difficult for the lack of a specific clinical presentation and laboratory or radiologic findings, leading differential diagnosis with other focal hepatic lesions the major problem [18]. The most frequent symptoms are abdominal pain and constitutional symptoms such as fever, malaise, fatigue and weight loss. Rarely patients present myalgia, jaundice and gastrointestinal upset [7, 12]. Only 9% of patients are asymptomatic. Laboratory tests can display an elevation of white blood cell counts (WCCs) and of acute-phase reactant inflammatory markers such as erythrocyte sedimentation rate (ESR) and CRP in 37% of patients, altered liver function tests in approximately 15% of patients [19]. US and CT scans are not specific, for the variable patterns of echogenicity or contrast enhancement and for the evidence of liver mass mimicking malignant lesion [18].
There are no typical histological features of IPTLs, but in a recent study Makhlouf et al described 145 cases of IPTL and identified five main histological subgroups: plasma cell-rich, mixed inflammatory cell, granulomatous with or without eosinophils and predominantly purulent. None of their cases stained positively for infectious agents and immunostaining found no evidence of lymphomas, IgG4-related disease or ALK-1 positive myofibroblastic tumors. Follow up data revealed no patients with subsequent evidence of neoplasms, recurrences or metastases [17]. Therefore it appears that IPTL is mainly a diagnosis of exclusion, both clinically and histologically. In our case, tumoral, infectious and granulomatous causes and IgG 4-related disease were ruled out and IPTL was associated with chronic lithiasic cholecystitis.
The natural clinical course of IPTL is spontaneous regression without intervention [12, 20], but treatment is often necessary. Although management options include conservative (antibiotics, NSADs and steroids) or surgical approaches, the treatment of choice is still surgical resection, especially for patients with severe symptoms or an indeterminate diagnosis [21, 22]. In addition, surgical resection avoids recurrence of lesion [3] and permits histological study of surgical specimen, determining a final diagnosis. In example, medical therapy with antibiotics, NSADs and steroids was administered to our patient, without clinical and radiological benefit. Therefore, patient underwent surgical resection, with resolution of clinical signs and symptoms.
4. Conclusion
Our case report of IPTL was associated with chronic lithiasic cholecystitis, in a patient where medical history, non-specific symptoms and imaging pointed towards an hepatic malignancy. Clinicians have to think about IPTL when hepatic mass is detected on radiological studies, but there are clinical signs, symptoms and laboratory tests suggesting inflammation. In addition, in this context diagnosis of IPTL was supported by negativity of tumor and autoimmunity markers, of hepatotropic viruses and by histopathological presence of inflammation cells, in absence of tumor cells.
The authors state that they have no Conflict of Interest (COI).
References
- Pack GT, Baker HW. Total Right Hepatic Lobectomy:Report Of A Case. Ann Surg 138 (1953): 253-258.
- Melloni G, Carretta A, Ciriaco P, et al. Inflammatory pseudotumor of the lung in adults. Ann Thorac Surg 79 (2005): 426-432.
- Zhang Y, Lu H, Ji H, et al. Inflammatory pseudotumor of the liver: A case report and literature review. Intractable Rare Dis Res 4 (2015): 155-158.
- Copin MC, Gosselin BH, Ribet ME. Plasma cell granuloma of the lung: difficulties in diagnosis and prognosis. Ann Thorac Surg 61 (1996): 1477-1482.
- Menias CO, Surabhi VR, Prasad SR, et al. Mimics of Cholangiocarcinoma: Spectrum of Disease. RadioGraphics 28 (2008): 1115-1129.
- Coffin CM, Humphrey PA, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor: a clinical and pathological survey. Semin Diagn Pathol 15 (1998): 85-101.
- Goldsmith PJ, Loganathan A, Jacob M, et al. Inflammatory pseudotumours of the liver: a spectrum of presentation and management options. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 35 (2009): 1295-1298.
- Gleason BC, Hornick JL. Inflammatory myofibroblastic tumours: where are we now? J Clin Pathol 61 (2008): 428-437.
- Agaimy A, Märkl B. Inflammatory angiomyolipoma of the liver: an unusual case suggesting relationship to IgG4-related pseudotumor. Int J Clin Exp Pathol 6 (2013): 771-779.
- Lévy S, Sauvanet A, Diebold M-D, et al. Spontaneous regression of an inflammatory pseudotumor of the liver presenting as an obstructing malignant biliary tumor. Gastrointest Endosc 53 (2001): 371-374.
- Bae SK, Abiru S, Kamohara Y, et al. Hepatic Inflammatory Pseudotumor Associated with Xanthogranulomatous Cholangitis Mimicking Cholangiocarcinoma. Intern Med 54 (2015): 771-775.
- Al-Hussaini H. Hepatic inflammatory pseudotumor presenting in an 8-year-old boy: A case report and review of literature. World J Gastroenterol 21 (2015): 8730.
- Ntinas A, Kardassis D, Miliaras D, et al. Inflammatory pseudotumor of the liver: a case report and review of the literature. J Med Case Reports 5 (2011): 196.
- Sanders BM, West KW, Gingalewski C, et al. Inflammatory pseudotumor of the alimentary tract: clinical and surgical experience. J Pediatr Surg 36 (2001): 169-173.
- You Y, Shao H, Bui K, et al. Epstein-Barr virus positive inflammatory pseudotumor of the liver: report of a challenging case and review of the literature. Ann Clin Lab Sci 44 (2014): 489-498.
- Zen Y, Fujii T, Sato Y, et al. Pathological classification of hepatic inflammatory pseudotumor with respect to IgG4-related disease. Mod Pathol Off J U S Can Acad Pathol Inc 20 (2007): 884-894.
- Balabaud C, Bioulac-Sage P, Goodman ZD, et al. Inflammatory pseudotumor of the liver: a rare but distinct tumor-like lesion. Gastroenterol Hepatol 8 (2012): 633-634.
- Kitajima K, Shiba H, Nojiri T, et al. Intrahepatic cholangiocarcinoma mimicking hepatic inflammatory pseudotumor. J Gastrointest Surg Off J Soc Surg Aliment Tract 11 (2007): 398-402.
- Torzilli G, Inoue K, Midorikawa Y, et al. Inflammatory pseudotumors of the liver: prevalence and clinical impact in surgical patients. Hepatogastroenterology 48 (2001): 1118-1123.
- Ishida H, Tatsuta M, Furukawa H, et al. Multiple inflammatory pseudotumors mimicking liver metastasis from colon cancer: report of a case. Surg Today 30 (2000): 530-533.
- Kaneko K, Ando H, Watanabe Y, et al. Aggressive preoperative management and extended surgery for inflammatory pseudotumor involving the hepatic hilum in a child. Surgery 129 (2001): 757-760.
- Chablé-Montero F, Angeles-Ángeles A, Albores-Saavedra J. Inflammatory myofibroblastic tumor of the liver. Ann Hepatol 11 (2012): 708-709.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
