Hepatic Veno-Occlusive Disease caused by Gynura Segetum: A Case Report
Article Information
Li Ya, Ma Yulin, Li Jialing, Wan Jing*
Department of cardiology, Zhongnan hospital, Wuhan University, Wuhan 430071, China
*Corresponding Author: Wan Jing, Department of cardiology, Zhongnan hospital, Wuhan University, Wuhan 430071, China
Received: 14 January 2019; Accepted: 22 February 2019; Published: 25 February 2019
Citation: Li Ya, Ma Yulin, Li Jialing, Wan Jing. Hepatic Veno-Occlusive Disease caused by Gynura Segetum: A Case Report. Cardiology and Cardiovascular Medicine 3 (2019): 009-014.
View / Download Pdf Share at FacebookAbstract
Objective: To analyze the clinical characteristics of Hepatic venous-occlusive disease induced by Gynura segetum.
Methods: The process of diagnosis and treatment of the patient with Hepatic venous-occlusive disease who are admitted to Zhongnan hospital.
Results: The patient has the following clinical features: he is an old man who has a history of taking Gynura segetum and has abdominal distension, abdominal pain, and ascites. We can diagnosis with the medical history and the auxiliary examination.
Conclusions: Gynura segetum is an important predisposing factor for Hepatic veno-occlusive disease. The clinical manifestations are mainly liver dysfunction and abnormal coagulation function. A detailed medical history and early diagnosis and treatment can contribute to a good prognosis during the clinical work, we should be aware of the correct use of Gynura segetum.
Keywords
Hepatic venous-occlusive disease, Gynura segetum
Article Details
1. Introduction
Hepatic venous-occlusive disease (HVOD), as known as hepatic sinusoidal obstruction syndrome (HSOS), is a disease that has an intrahepatic retrosternal portal hypertension caused by endothelial swelling and fibrosis of central hepatic lobular veins and branches of hepatic venules, which leads to stenosis or even occlusion of the lumen of veins [1]. The clinical manifestations are hyperbilirubinemia, abdominal pain, ascites, and weight gain. The hepatic venous-occlusive syndrome was first reported by Willmot and Robertson in 1920 as a result of taking Senecio tea containing pyrrolidine alkaloids (PA) [2]. In recent years, many cases of HVOD induced by taking Gynura segetum have been reported. Here, we report a case of HVOD that has a history of ingestion of Gynura segetum.
2. Case Presentation
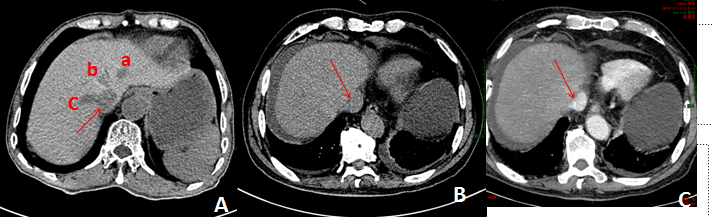
An 83-year-old male was admitted into Zhongnan Hospital of Wuhan University on September 17, 2018, presented with abdominal pain, abdominal distension for 15 days. There was no obvious inducement of abdominal distension or pain 15 days ago. The pain was obvious under the xiphoid and aggravated after eating, accompanying acid regurgitation, nausea. The patient had a long history of taking traditional Chinese medicine such as “Gynura segetum” recently and has a history of polypectomy in 2013. On physical examination: his abdominal protuberance is obvious, mild tenderness in the subxiphoid. At Admission, laboratory tests showed that blood, urine, and feces+occult blood routine were normal. Alanine aminotransferase (ALT): 88 U/L; aspartate transaminase (AST): 162 U/L; total bilirubin (TBIL): 131.4 µmol/L; direct bilirubin (DBIL): 65.6 µmol/L; indirect bilirubin (IDBIL): 65.8 µmol/L, glucose (GLU): 4.08 µmol/L; albumin (ALB): 35.1 g/L; gamma glutamyl transpeptidase (rGGT): 194 U/L; alkaline phosphatase (ALP): 216 U. Renal function, blood lipid, myocardial enzymes, brain natriuretic peptide, and thyroid function were normal. Thrombography: prothrombin time: 19.1 seconds; prothrombin time activity: 42%; Infection indicators: hepatitis B, hepatitis C, HIV, Tuberculosis and syphilis were negative. Tumor markers: alpha-fetoprotein (AFP) was normal. Autoimmune liver disease and liver fibrosis were excluded. Routine and biochemical examination of ascites indicated that the ascites was transudate and bacterial culture was negative. Ascites tumor markers (CEA, AFP, CA199) were negative. Ascites bacterial culture, acid-fast staining, cytological examination of ascites exfoliation were normal. The results of laboratory tests indicated liver injury and abnormal coagulation function. Abdominal CT showed that the volume of the liver was normal, the density of liver parenchyma was normal, and effusion was seen around the liver and in the left thoracic cavity. (Figure 1B) contrast-enhanced CT shows that the diameter of the main portal vein was about 8 mm. The trunk of the portal vein and its branches were clearly displayed. No obvious stenosis, dilation and filling defect was observed. The main trunk and branches of the hepatic vein were not clearly seen. The peritoneal effusion and a small amount of pleural effusion on the left side (Figure 1C).
Figure 1: (A) is the CT of normal person, a means Left hepatic vein, b means Middle hepatic vein, c means Right hepatic vein; (B) and (C) is the CT of this patient, the arrow points to the inferior vena cava, and hepatic veins were not clearly seen, effusion was seen around the liver and in the left thoracic cavity in both (B) and (C).
2.1 Treatment
On the basis of a history of taking Gynura segetum, typical clinical presentation, laboratory tests, the results of CT, the patient was diagnosed with HVOD. For the treatment, glutathione (1.8 g, ivgtt, Qd) and Ademetionine(1.5 g, ivgtt, Qd) for improving the liver functions, cefminox (2.0g, ivgtt, Bid) for the prevention of infection, Furosemide (20 mg, iv, Qd) and spironolactone tablets (20 mg, po, Bid)as diuretics to dehydrate, alprostadil (5 ug, iv, Qd ) for improving the blood circulation, human serum albumin (20 g, ivgtt, Qd) to maintain oncotic pressure several times abdominal paracentesis to control the symptoms of abdominal oppression , lansoprazole (30 mg, ivgtt, Bid)and nutrition support(Vitamins and Amino Acids) were added. Before the day of discharge, the results of laboratory tests showed that Alanine aminotransferase (ALT): 37 U/L; aspartate transaminase (AST): 40 U/L; total bilirubin (TBIL): 35.3 umol/L; direct bilirubin (DBIL): 12.2 umol/L; indirect bilirubin (IDBIL): 23.1 umol/L, gamma glutamyl transpeptidase (rGGT): 60U/L; alkaline phosphatase (ALP): 104 U. Thrombography: prothrombin time: 15.6 seconds; prothrombin time activity: 56%. On 3 November, the patient was discharged.
2.2 Prognosis
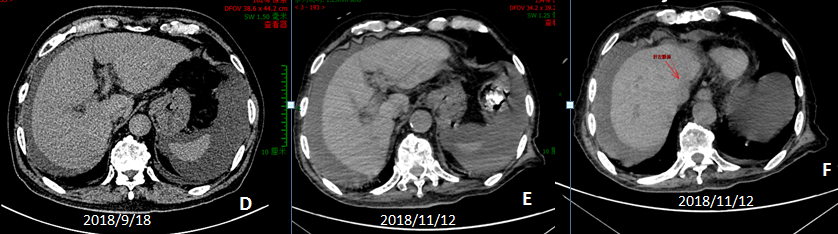
The patient came to our hospital again on November 12, 2018. The results of laboratory tests showed that Alanine aminotransferase (ALT): 16 U/L; aspartate transaminase (AST): 31 U/L; total bilirubin (TBIL):151.6 µmol/L; direct bilirubin (DBIL): 114.4 µmol/L; indirect bilirubin (IDBIL): 37.2 µmol/L, gamma glutamyl transpeptidase (rGGT): 68 U/L; alkaline phosphatase (ALP): 128 U. Thrombography: prothrombin time: 16 seconds; prothrombin time activity: 59%. Abdominal CT showed that the density of the liver was increased and the volume of the liver was slightly reduced, hepatic fissure was widened. The peritoneal effusion increased and the arc-shaped low-density shadow was seen around the liver, but we can see the left hepatic vein (Figure 2). We give the patient symptomatic supportive treatment, now this patient is still alive and follow-up in the outpatient department.
Figure 2: (D) is the previous CT, (D) and (E) are the later CT, (E) compared with (D), we can see the density of the liver was increased and the volume of liver was slightly reduced, the hepatic fissure was widened. The peritoneal effusion increased. But we can see the left hepatic vein (the red arrow).
3. Discussion
Hepatic venous-occlusive disease is an unpredictable disease associated with endothelial cell damage [3]. In a Western country, the hepatic venous-occlusive disease is mainly caused by hematopoietic stem cell transplantation [4], while in China; it is mainly caused by Gynura segetum [5]. The main clinical manifestations of HVOD were abdominal distention, abdominal pain, jaundice, and ascites. Gynura segetum is a widely used traditional Chinese medicine, which contains PA. It has the functions of improving blood circulation, removing blood stasis and pain relief. It is often used in the treatment of trauma, fracture of the bone and joint diseases. In recent years, more and more domestic literature reported that Gynura segetum lead to HVOD, and the more dosage we take, the longer time we take, the more serious the situation was. The mechanism of HVOD caused by Gynura segetum is still unclear. Some researchers suggest that PA can reduce the expression of glutathione (GSH) in sinus endothelial cells [6]. The hepatotoxicity of PA in Gynura segetum was also confirmed in animal experiments [7].
Diagnosis of HVOD is relatively difficult. According to clinical criteria, HVOD has clinically defined as a combination of at least two of the following three criteria: (1) hepatomegaly or pain in the right upper quadrant, (2) jaundice (3) ascites or unexplained weight gain [8]. We can diagnose with a detailed medical history, clinical manifestations and images. Liver biopsy is the gold standard for diagnosis. However, due to severe ascites, poor coagulation function and thrombocytopenia, there are fewer punctures in the clinic because of the high risk of liver biopsy. The most common features of pre-contrast CT in the patients with HVOD are ascites and the global enlargement of the liver. On contrast-enhanced CT, patchy liver enhancement and heterogeneous hypoattenuation are two most common radiologic findings in PAs-induced HVOD, heterogeneous hypoattenuation in portal phase was the most important feature of PAs-induced HVOD on contrast-enhanced CT [9].
present, the treatment of HVOD is mainly symptomatic supportive treatment, including restricting fluid intake, reducing water and sodium retention, improving the liver functions, maintaining water-electrolyte balance, nutritional support therapy, and infection control [10]. When fluid retention cannot be controlled, peritoneal dialysis was necessary [11]. Transjugular intrahepatic portosystemic shunt (TIPS), an approach to decrease the intrahepatic vascular pressure by creating a shunt, which was not recommended for patients with HVOD [1]. Drug therapy is currently recommended as follows: (1) Defibrin: the drug with the most comprehensive and consistent evidence of efficacy, it can protect endothelial cells and has an anti-inflammatory effect [12]. (2) Use of LMWH is highly controversial because of bleeding risk [13]. (3) Methylprednisolone: inhibits the production of cytokines and has many adverse reactions, a lot of clinical trials are still needed [14]. Some scholars recommend that early liver transplantation can improve the prognosis of patients [15]. For HVOD caused by Gynura segetum, early diagnosis and symptomatic support therapy can prevent disease progression and improve prognosis. In conclusion Chinese herbal medicine containing PA, represented by Gynura segetum, is widely used by Chinese people, but its toxicity is not well understood. Clinicians should strengthen the understanding of HVOD caused by PA and strengthen the education of this kind of Chinese herbal medicine to reduce the occurrence of HVOD caused by Gynura segetum.
4. Conclusion
Chinese herbal medicine containing PA, represented by Gynura segetum, is widely used by Chinese people, but its toxicity is not well understood. Clinicians should strengthen the understanding of HVOD caused by PA and strengthen the education of this kind of Chinese herbal medicine to reduce the occurrence of HVOD caused by Gynura segetum.
Conflict of Interest
The authors indicated no potential conflicts of interest
References
- Sun Z, Kang J, Zhang Y. Hepatic veno-occlusive disease related to Gynura segetum: A case report. Medicine (Baltimore) 97 (2018): e0552.
- Wang JY, Gao H. Tusanqi and hepatic sinusoidal obstruction syndrome. J Dig Dis 15 (2014): 105-107.
- Richardson PG, Triplett BM, Ho VT, et al. Defibrotide sodium for the treatment of hepatic veno-occlusive disease/sinusoidal obstruction syndrome. Expert Rev Clin Pharmacol 11 (2018): 113-124.
- Mohty M, Malard F, Abecassis M, et al. Sinusoidal obstruction syndrome/veno-occlusive disease: current situation and perspectives-a position statement from the European Society for Blood and Marrow Transplantation (EBMT). Bone Marrow Transplant 50 (2015): 781-789.
- Wang X, Qi X, Guo X. Tusanqi-Related Sinusoidal Obstruction Syndrome in China: A Systematic Review of the Literatures. Medicine (Baltimore) 94 (2015): e942.
- Wang X, Kanel GC, DeLeve LD. Support of Sinusoidal Endothelial Cell Glutathione Prevents Hepatic Veno-occlusive Disease in the Rat. Hepatology 31 (2000): 428-434.
- Yang M, Ruan J, Gao H, et al. First evidence of pyrrolizidine alkaloid N-oxide-induced hepatic sinusoidal obstruction syndrome in humans. Arch Toxicol 91 (2017): 3913-3925.
- Park JE, Choi YH, Cheon JE, et al. Gallbladder wall oedema and ascites are independent predictors of progression to hepatic veno-occlusive disease for children with hematopoietic stem cell transplantation. Eur Radiol 28 (2018): 2291-2298.
- Xuefeng Kan, Jin Ye, Xinxin Rong, et al. Diagnostic performance of Contrast-enhanced CT in Pyrrolizidine Alkaloids-induced Hepatic Sinusoidal Obstructive Syndrome. Sci Rep 6 (2016): 37998.
- Mesini A, Cangemi G, Palmisani E, et al. Hepatic veno-occlusive disease during isavuconazole administration. J Chemother 30 (2018): 63-64.
- Parmar V, Lewis M, Shenoy M, et al. Ascitic fluid drainage using a peritoneal dialysis catheter to prevent and treat multi-organ dysfunction in veno-occlusive disease in children undergoing hematopoietic stem cell transplantation. Pediatr Blood Cancer 64 (2017).
- Faraci M, Bertaina A, Luksch R, et al. Sinusoidal obstruction syndrome veno-occlusive disease. Biol Blood Marrow Transplant 25 (2019): 313-320
- Wang Y, Qiao D, Li Y, et al. Risk factors for hepatic veno-occlusive disease caused by Gynura segetum: a retrospective study. BMC Gastroenterol 18 (2018): 156.
- Dalle JH, Giralt SA. Hepatic Veno-Occlusive Disease after Hematopoietic Stem Cell Transplantation: Risk Factors and Stratification, Prophylaxis, and Treatment. Biol Blood Marrow Transplant 22 (2016): 400-409.
- Harimoto N, Yugawa K, Ikegami T, et al. Hepatobiliary and Pancreatic: Pregnancy induced hepatic veno-occlusive disease requiring liver transplantation. J Gastroenterol Hepatol 33 (2018): 9.


 Impact Factor: * 3.5
Impact Factor: * 3.5 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 14.80%
Acceptance Rate: 14.80%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 