Impact of Group Prenatal Care Support on Breastfeeding Initiation Rates and Other Maternal and Perinatal Outcomes
Article Information
Pau Nicolau1, Susana Rodriguez2, Paula Maso1, Silvia Agramunt1,3, Emerita Garcia2, Assumpcio Sala2, Mar Vernet-Tomas1,3, Antonio Paya1,3
1Gynecologist. Gynecology and Obstetrics Department, Hospital del Mar and Primary Care Centers, Barcelona, Spain
2Nurse-Midwife. Gynecology and Obstetrics Department, Hospital del Mar and Primary Care Centers, Barcelona, Spain
3Universitat Autònoma de Barcelona, Campus de la UAB, Plaza Cívica, Barcelona, Spain
*Corresponding Author: Pau Nicolau, Gynecologist. Gynecology and Obstetrics Department, Hospital del Mar and Primary Care Centers, Barcelona, Spain
Received: 03 April 2018; Accepted: 10 April 2018; Published: 13 April 2018
Citation:
Pau Nicolau, Susana RodrÃguez, Paula Masó, Silvia Agramunt, Emerita Garcia, Assumpció Sala, Mar Vernet-Tomás, Antonio Payá. Impact of Group Prenatal Care Support on Breastfeeding Initiation Rates and Other Maternal and Perinatal Outcomes. Obstetrics and Gynecology Research 1 (2018): 038-044.
View / Download Pdf Share at FacebookAbstract
Group prenatal care support has been studied in order to increase maternal and neonatal benefits, such as breastfeeding initiation rates, in front of standard care. In our area, especially in some high risk sub-groups, it could be an important intervention to improve individual care.
The aim of the pilot initiative is to compare the effect of group prenatal care support versus only standard individual care on breastfeeding initiation rates and other perinatal outcomes. A retrospective cohort study was made analyzing all deliveries at Hospital del Mar in Barcelona during 1 year. All pregnant women were compared depending on whether they had received the group prenatal care support by midwifes or only standard care. 1383 women gave birth at Hospital del Mar in Barcelona in 2015. 207 received group prenatal care support (15% of total). In group prenatal care there significantly were more nulliparous and native women. Breastfeeding initiation rate was higher in group prenatal care women (94.2% vs. 86.7%, p=0.01). Other outcomes like cesarean section rates, prematurity and low birth weight rates also improved in group prenatal care support in front of standard care.
Our study suggests that group prenatal care support improves breastfeeding initiation rates and some other maternal and perinatal outcomes.
Keywords
Antepartum care; Breastfeeding; Group care; Vulnerable population
Antepartum care articles Antepartum care Research articles Antepartum care review articles Antepartum care PubMed articles Antepartum care PubMed Central articles Antepartum care 2023 articles Antepartum care 2024 articles Antepartum care Scopus articles Antepartum care impact factor journals Antepartum care Scopus journals Antepartum care PubMed journals Antepartum care medical journals Antepartum care free journals Antepartum care best journals Antepartum care top journals Antepartum care free medical journals Antepartum care famous journals Antepartum care Google Scholar indexed journals Breastfeeding articles Breastfeeding Research articles Breastfeeding review articles Breastfeeding PubMed articles Breastfeeding PubMed Central articles Breastfeeding 2023 articles Breastfeeding 2024 articles Breastfeeding Scopus articles Breastfeeding impact factor journals Breastfeeding Scopus journals Breastfeeding PubMed journals Breastfeeding medical journals Breastfeeding free journals Breastfeeding best journals Breastfeeding top journals Breastfeeding free medical journals Breastfeeding famous journals Breastfeeding Google Scholar indexed journals Group care articles Group care Research articles Group care review articles Group care PubMed articles Group care PubMed Central articles Group care 2023 articles Group care 2024 articles Group care Scopus articles Group care impact factor journals Group care Scopus journals Group care PubMed journals Group care medical journals Group care free journals Group care best journals Group care top journals Group care free medical journals Group care famous journals Group care Google Scholar indexed journals Vulnerable population articles Vulnerable population Research articles Vulnerable population review articles Vulnerable population PubMed articles Vulnerable population PubMed Central articles Vulnerable population 2023 articles Vulnerable population 2024 articles Vulnerable population Scopus articles Vulnerable population impact factor journals Vulnerable population Scopus journals Vulnerable population PubMed journals Vulnerable population medical journals Vulnerable population free journals Vulnerable population best journals Vulnerable population top journals Vulnerable population free medical journals Vulnerable population famous journals Vulnerable population Google Scholar indexed journals pregnant women articles pregnant women Research articles pregnant women review articles pregnant women PubMed articles pregnant women PubMed Central articles pregnant women 2023 articles pregnant women 2024 articles pregnant women Scopus articles pregnant women impact factor journals pregnant women Scopus journals pregnant women PubMed journals pregnant women medical journals pregnant women free journals pregnant women best journals pregnant women top journals pregnant women free medical journals pregnant women famous journals pregnant women Google Scholar indexed journals fetus articles fetus Research articles fetus review articles fetus PubMed articles fetus PubMed Central articles fetus 2023 articles fetus 2024 articles fetus Scopus articles fetus impact factor journals fetus Scopus journals fetus PubMed journals fetus medical journals fetus free journals fetus best journals fetus top journals fetus free medical journals fetus famous journals fetus Google Scholar indexed journals postnatal care articles postnatal care Research articles postnatal care review articles postnatal care PubMed articles postnatal care PubMed Central articles postnatal care 2023 articles postnatal care 2024 articles postnatal care Scopus articles postnatal care impact factor journals postnatal care Scopus journals postnatal care PubMed journals postnatal care medical journals postnatal care free journals postnatal care best journals postnatal care top journals postnatal care free medical journals postnatal care famous journals postnatal care Google Scholar indexed journals third trimester articles third trimester Research articles third trimester review articles third trimester PubMed articles third trimester PubMed Central articles third trimester 2023 articles third trimester 2024 articles third trimester Scopus articles third trimester impact factor journals third trimester Scopus journals third trimester PubMed journals third trimester medical journals third trimester free journals third trimester best journals third trimester top journals third trimester free medical journals third trimester famous journals third trimester Google Scholar indexed journals pregnancy articles pregnancy Research articles pregnancy review articles pregnancy PubMed articles pregnancy PubMed Central articles pregnancy 2023 articles pregnancy 2024 articles pregnancy Scopus articles pregnancy impact factor journals pregnancy Scopus journals pregnancy PubMed journals pregnancy medical journals pregnancy free journals pregnancy best journals pregnancy top journals pregnancy free medical journals pregnancy famous journals pregnancy Google Scholar indexed journals maternal articles maternal Research articles maternal review articles maternal PubMed articles maternal PubMed Central articles maternal 2023 articles maternal 2024 articles maternal Scopus articles maternal impact factor journals maternal Scopus journals maternal PubMed journals maternal medical journals maternal free journals maternal best journals maternal top journals maternal free medical journals maternal famous journals maternal Google Scholar indexed journals
Article Details
1. Introduction
Obstetrics, from the Latin “obstare” (-waiting for-), consists of controlling and attending pregnant women, fetus circumstances and childbirth. Prenatal care was first documented in Ancient Egypt (Ebers Papyrus, 1500 b.C.), but it did not have a key role until 20th century. Traditional prenatal care, understood as classical individual medical or midwife attention, has historically aimed to the antenatal time and the moment of childhood [1]. Prenatal care pretends to improve perinatal outcomes in terms of prematurity, low birth weight, screening of maternal conditions such as preeclampsia or gestational diabetes, as well as global fetal and maternal morbidity and mortality. More recently, different strategies in prenatal phase have also worked in postnatal care, as for breastfeeding initiation rates [2]. Even though the frequency, the tools and type of follow-up in low risk pregnancies remain controversial [3]. In this way, prenatal care could be particularly useful for high risk demographic sub-groups like immigrants or women with a low socio-economic status [4, 5] for who breastfeeding could be harder to implement [6].
Several strategies have been studied in order to increase the benefits of traditionalindividual prenatal care. In some vulnerable women, the effectiveness of programs as extending the number of controls, practicing telephonic support or realizing home visits have been reviewed [7]. The role of group prenatal care (GPC) has also been analyzed. Most of studies conclude that subjective perception and satisfaction of health attention, and some of the perinatal outcomes could improve with this model [8]; other authors refer it would not be worse than standard individual care (SIC) [9, 10]. According to the literature, previous meta-analysis and systematic reviews showed that the level of evidence is limited due to the lack of randomized control trials and heterogeneity of patterns of the group sessions [11, 12]. Although the evidence is scarce, some groups like the Dr Ickovics with the program Centering Pregnancy, have been working with adolescent girls, ethnical minorities and low socio-economic status groups of women with good results, especially in terms like breastfeeding initiation [13-15]. In this way, other groups working with this intervention have proposed some recommendations for the model implementation [16].
In our country, GPC was historically focused in the moment of childbirth, not in the pregnancy or post-partum phases. GPC support is nowadays understood as a complementary intervention additional to the traditional SIC at the third trimester [17]. Our institution, like other centers [18], detected a need of increasing the breastfeeding rates, especially in those vulnerable sub-groups of women who remain a high in proportion in our area [19].
The aim of this study is to compare the effect of GPC support versus only SIC on breastfeeding initiation rates and other perinatal outcomes.
2. Materials and Methods
2.1 DesignWe planned a retrospective cohort study.
2.2 Sample
We recorded data from all deliveries at Hospital del Mar in Barcelona from 1st of January to 31st of December 2015. The sample analyzed included 1383 women.
2.3 Setting
All pregnant women who gave birth in our center during the study period were grouped depending on whether they had received the GPC support. The sessions of GPC support were made in 10 public primary care centers in our referral zone by midwifes and consisted of weekly small group sessions (8-10 women), for women enrolled in the third trimester of pregnancy, additional to individual gynecologist monthly care. In our area, pregnant women choose to receive this intervention that midwifes offer in the first appointments. In these 1 hour sessions, midwifes conduct different issues about pregnancy, childbirth and post-partum, and all women can participate expressing doubts and opinions.
2.4 Measurement
Data on maternal demographics, pregnancy and delivery were retrieved from clinical records. To compare homogeneity between both groups we included the following variables: average maternal age, gestational age and ethnicity. To compare outcomes for both groups we compared: breastfeeding initiation rates, labor stage at hospital admission, and mode of delivery and presence of episiotomy/lacerations. Prematurity rates (defined as a gestational age below 37 weeks) and low birth weight rates (defined as weight below 2500 grams) were taken into account in both groups.
2.5 Analysis
We performed the statistical analysis with PAWS program 18th version (IBMR SPSSR software). Continuous variables were compared by t-Student and U Mann-Whitney. The comparisons of dichotomic variables were performed with Chi-square and exact Fisher tests. For all studies we considered the level of bilateral statistical significance at alpha type error below 0.05.
We followed the recommendations of Helsinki Declaration.
3. Results
During the study period, 1383 women gave birth at our center in Barcelona. Average maternal age was 30.6 years old (rank 14 ? 46), with a range of gestational age from 24.0 to 42.4 weeks of pregnancy, and with a birth weight range from 500 to 4990gr. Regarding ethnicities, 45.8% were European Caucasian women, 20.5% from South-East Asia, 17.9% from South-America, 7.7% from Maghreb, 6.5% from Oriental countries and 1.6% from other regions.
Two hundred and 7 women of the entire cohort went through GPC support during 2015 in the third trimester of pregnancy (15% of total). When comparing statistical descriptive outcomes, we found older women (31.9 years old vs. 30.4 years old, p<0.05) and a higher proportion of nulliparous women in GPC than in non-intervention group (81% vs. 40%, p<0.05). Seventy-three percent of women who received GPC were European Caucasian, and only 3% of them were South-East Asian (Pakistani, Indian and Bengali, who represent the second most frequent ethnicity in our zone); in the other side, 23.7% of women in non-intervention group were South-East Asian (p<0.05) (Figure 1).
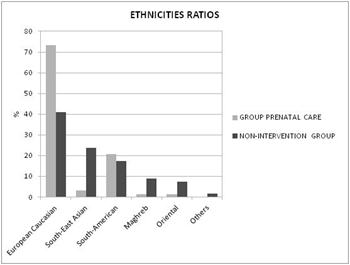
Figure 1: Ethnicities ratios of group prenatal care and non-intervention group.
Regarding perinatal outcomes, there were several significant results in the group who received GPC support (Table 1). Breastfeeding initiation rate was higher in this cohort of women (94.2% vs. 86.7%, p=0.01). Labor stage at hospital admission, mode of delivery, and episiotomy and lacerations rates were also analyzed. There was a significant higher rate of cesarean section in non-intervention-group (22.8% vs. 20.8%, p< 0.001), which represents 28 surgeries/year more in our hospital. In GPC support, there was a 63% of need of episiotomy or tears reparation in front of 52% in non-intervention group in vaginal deliveries (p=0.001). In terms of prematurity rates (2.0% vs. 7.6%, p=0.008) and low birth weight (3.4% vs. 9.1%, p=0.01), GPC was also an improvement tool. Regarding the maternal age in the moment of the childhood, we observed less extreme ages in the GPC.
|
Group Prenatal Care |
Non-Intervention Group |
Significance |
|
|
Breastfeeding initiation |
94.2% (195) |
86.7% (1019) |
P=0.01 |
|
Mode of delivery |
|||
|
- spontaneous vaginal |
51.7% (107) |
61.7% (725) |
P<0.001 |
|
- instrumental vaginal |
27.5% (57) |
15.5% (182) |
|
|
- cesarean section |
20.8% (43) |
22.8% (268) |
|
|
Vaginal deliveries |
P=0.001 |
||
|
- integrum perineum |
30% (62) |
40.3% (474) |
|
|
- episiotomy |
36.2% (75) |
24.1% (283) |
|
|
- tears grade I-II |
23.7% (49) |
26.5% (311) |
|
|
- tears grade III-IV |
2.9% (6) |
1.1% (14) |
|
|
- no data |
7.2% (15) |
7.9% (93) |
|
|
Prematurity <37weeks |
2.0% (4) |
7.6% (86) |
P=0.008 |
|
Extreme weights |
|||
|
- low birth weight < 2500gr |
3.4%(7) |
9.1% (107) |
P=0.01 |
|
- macrosoma >4000gr |
3.9% (8) |
5.7% (67) |
|
|
Extreme ages in the childbirth |
|||
|
- <18 years old |
1.0% (2) |
2.3% (27) |
P<0.001 |
|
- >40 years old |
2.4% (5) |
4.4% (51) |
Table 1: Results shows group prenatal care and non-intervention group.
4. Discussion
Our study supports the idea that GPC support increases breastfeeding rates after the childbirth. Almost 104 women more would initiate breastfeeding if group intervention support was carried on by all pregnant women every year in our area. The intervention has also a beneficial impact for pregnant women in some other maternal and perinatal outcomes, especially in terms of reduction of cesarean section rates, prematurity and low birth weight.
Some strength should be noted in our study. It is an annual analysis of all the deliveries, which could be a good approach to our reality. Our center, located in a high immigration area, assists several different ethnicities every day. These different cultures could translate into a very different ways to take care of the pregnancy and subjective experiences during the delivery or in the breastfeeding initiation [20], so interventions like GPC support could help them to receive the same information and to avoid problems associated to language barriers. Although our personal is well-trained and experienced in pregnant women from different cultures, more strategies should be thought to improve their maternity. The absolute results are moderate, but in our center (which consists in a medium size maternity in the country) these rates represent good improvements both for maternal and neonatal health, and in terms of hospital costs and public health system effectively.
In the same direction, there are some limitations as well. It is a retrospective study, including women who voluntarily receive GPC support, and this fact could lead to a selection bias so these women could not be representative of all the population. In GPC older, nulliparous and native pregnant women are significantly higher than in the SIC. Native women in our country are usually more informed than the immigrant ones about health practices like breastfeeding, or about the health system [21]. In this way, future prospective randomized projects in our area should be planned to clarify the benefits of the group prenatal intervention. Regarding specific details in the GPC, although the cesarean section rate is lower the instrumental vaginal delivery rate is higher, with more need of episiotomy and laceration reparations. This situation could be explained because these well-informed women could have an increased interest to get the vaginal delivery, so it could represent a specific issue to improve in the future. It was not documented if the delivery provider was a physician or a midwife, and as we know from previous research it could be interesting information.
5. Conclusion
In conclusion, GPC support improves breastfeeding initiation rates and some other maternal and perinatal outcomes in our area. More prospective randomized studies should be done to establish the benefits of this intervention during the whole pregnancy, and new strategies should be thought to arrive to all the pregnant women population.
References
- Ryan GM, Sweeney PJ, Solola AS. Prenatal care and pregnancy outcomes. American Journal of Obstetrics and Gynecology 137 (1980): 876-881.
- McFadden A, Gavine A, Renfrew MJ, et al. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Systematic Review 2 (2017).
- Khan-Neelofur D, GuÈlmezoglu M, Villar JA. Who should provide routine antenatal care for low risk women and how often? A systematic review of randomised controlled trials. WHO Antenatal Care Trial Research Group. Paediatric Perinatology Epidemiology 2 (1998): 7-26.
- Henderson J, Gao H, Redshaw M. Experiencing maternity care: the care received and perceptions of women from different ethnic groups. BMC Pregnancy and Childbirth 13 (2013): 196.
- Lindquist A, Kurinczuk JJ, Redshaw M. Experiences utilisation and outcomes of maternity care in England among women from different socio-economic groups: findings from the 2010 National Maternity Survey. British Journal of Obstetrics and Gynecology 122 (2015): 1610-1617.
- Colodro-Conde L, Sánchez-Romera JF, Tornero-Gómez MJ, et al. Relationship between level of education and breastfeeding duration depends on social context: breastfeeding trends over a 40-year period in Spain. Journal of Human Lactation 27 (2011): 272-278.
- Hollowell J, Oakley L, Kurinczuk JJ. The effectiveness of antenatal care programs to reduce infant mortality and preterm birth insocially disadvantaged and vulnerable women in high-income countries: a systematic review. BMC Pregnancy and Childbirth 11 (2011): 13.
- McDonald SD, Swordm W, Eryuzlu LE. A qualitative descriptive study of the group prenatal care experience: perceptions of women with low-risk pregnancies and their midwives. BMC Pregnancy and Childbirth 14 (2014): 334.
- Thielen K. Exploring the group prenatal care model: a critical review of the literature. The Journal of Perinatal Education Fall 21 (2012): 209-218.
- Ruiz-Mirazo E, Lopez-Yarto M, McDonald SD. Group prenatal care versus individual prenatal care: a systematic review and meta-analyses. Journal of Obstetrics and Gynaecology Canada 34 (2012): 223-229.
- Homer CS, Ryan C, Leap N. Group versus conventional antenatal care for women. Cochrane Database Systematic Review 11 (2012).
- Catling CJ, Medley N, Foureur M. Group versus conventional antenatal care for women. Cochrane Database Systematic Review 2 (2015).
- Ickovics JR, Kershaw TS, Westdahl C. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstetrics and Gynecology 110 (2007): 330-339.
- Ickovics JR, Reed E, Magriples U. Effects of group prenatal care on psychosocial risk in pregnancy: results from a randomized controlled trial. Psychology Health 26 (2011): 235-250.
- Ickovics JR, Earnshaw V, Lewis JB. Cluster Randomized Controlled Trial of Group Prenatal Care: Perinatal Outcomes Among Adolescents in New York City Health Centers. American Journal of Public Health 106 (2016): 359-365.
- Tilden EL, Hersh SR, Emeis CL. Group prenatal care: review of outcomes and recommendations for model implementation. Obstetrics and Gynecology Survey 69 (2014): 46-55.
- Departament de Salut Generalitat de Catalunya. Educació maternal preparació al naixement (2009).
- Schreck PK, Solem K, Wright T, et al. Both Prenatal and Postnatal Interventions Are Needed to Improve Breastfeeding Outcomes in a Low-Income Population. Breastfeed Med 12 (2017):142-148.
- Nicolau P, del Amo E, Carreras R. Primary gynecological care in multicultural areas. Medicina Clinica (Barcelona) Apr 7. Epub ahead of print (2017).
- Small R, Roth C, Raval M, et al. Immigrant and non-immigrant women’s experiences of maternity care: a systematic and comparative review of studies in five countries. BMC Pregnancy and Childbirth 14 (2014): 152.
- Gotsens M, Malmusi D, Villarroel N, et al. Health inequality between immigrants and natives in Spain: the loss of the healthy immigrant effect in times of economic crisis. European Journal of Public Health 25 (2015): 939-939.


 Impact Factor: * 3.2
Impact Factor: * 3.2 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 