Infratentorial Posterior Reversible Encephalopathy Syndrome (PRES) Presenting with Hydrocephalus
Article Information
Whitehead C1, Reehal R2, Shumon S3
1Core Surgical Trainee, Newcastle Upon Tyne Hospitals, United Kingdom
2Core Surgical Trainee, Northern deanery
3Neurosurgical Trainee, Northern deanery
*Corresponding Author: Dr. Whitehead C, Core Surgical Trainee, Northern deanery, Newcastle Upon Tyne Hospitals, United Kingdom
Received: 09 Sep 2019; Accepted: 30 September 2019; Published: 28 November 2019
Citation: Whitehead C, Reehal R, Shumon S. Infratentorial Posterior Reversible Encephalopathy Syndrome (PRES) Presenting with Hydrocephalus. Archives of Clinical and Medical Case Reports 3 (2019): 670-674.
View / Download Pdf Share at FacebookAbstract
Posterior reversible leukoencephalopathy syndrome (PRES) is a cranial disorder linked to hypertension usually presenting with symptoms of headache, nausea and vomiting, seizures and visual disturbance. We present a rare case of PRES jointly managed by neurology and neurosurgery with an EVD and antihypertensive therapy in a 46 year old female who presented with hydrocephalus at Newcastle Upon Tyne Hospitals. Cases of PRES presenting in this way were rare with only 8 cases being described in the past. These cases tend to be in a much younger patient subset who were more often male. Management has varied in the past described cases and more literature is required to reach a concensus.
Keywords
Reversible Encephalopathy Syndrome; Posterior reversible leukoencephalopathy syndrome; Neurology; Neurosurgery
Reversible Encephalopathy Syndrome articles, Posterior reversible leukoencephalopathy syndrome articles, Neurology articles, Neurosurgery articles
Reversible Encephalopathy Syndrome articles Reversible Encephalopathy Syndrome Research articles Reversible Encephalopathy Syndrome review articles Reversible Encephalopathy Syndrome PubMed articles Reversible Encephalopathy Syndrome PubMed Central articles Reversible Encephalopathy Syndrome 2023 articles Reversible Encephalopathy Syndrome 2024 articles Reversible Encephalopathy Syndrome Scopus articles Reversible Encephalopathy Syndrome impact factor journals Reversible Encephalopathy Syndrome Scopus journals Reversible Encephalopathy Syndrome PubMed journals Reversible Encephalopathy Syndrome medical journals Reversible Encephalopathy Syndrome free journals Reversible Encephalopathy Syndrome best journals Reversible Encephalopathy Syndrome top journals Reversible Encephalopathy Syndrome free medical journals Reversible Encephalopathy Syndrome famous journals Reversible Encephalopathy Syndrome Google Scholar indexed journals Encephalopathy Syndrome articles Encephalopathy Syndrome Research articles Encephalopathy Syndrome review articles Encephalopathy Syndrome PubMed articles Encephalopathy Syndrome PubMed Central articles Encephalopathy Syndrome 2023 articles Encephalopathy Syndrome 2024 articles Encephalopathy Syndrome Scopus articles Encephalopathy Syndrome impact factor journals Encephalopathy Syndrome Scopus journals Encephalopathy Syndrome PubMed journals Encephalopathy Syndrome medical journals Encephalopathy Syndrome free journals Encephalopathy Syndrome best journals Encephalopathy Syndrome top journals Encephalopathy Syndrome free medical journals Encephalopathy Syndrome famous journals Encephalopathy Syndrome Google Scholar indexed journals Syndrome articles Syndrome Research articles Syndrome review articles Syndrome PubMed articles Syndrome PubMed Central articles Syndrome 2023 articles Syndrome 2024 articles Syndrome Scopus articles Syndrome impact factor journals Syndrome Scopus journals Syndrome PubMed journals Syndrome medical journals Syndrome free journals Syndrome best journals Syndrome top journals Syndrome free medical journals Syndrome famous journals Syndrome Google Scholar indexed journals Posterior reversible leukoencephalopathy syndrome articles Posterior reversible leukoencephalopathy syndrome Research articles Posterior reversible leukoencephalopathy syndrome review articles Posterior reversible leukoencephalopathy syndrome PubMed articles Posterior reversible leukoencephalopathy syndrome PubMed Central articles Posterior reversible leukoencephalopathy syndrome 2023 articles Posterior reversible leukoencephalopathy syndrome 2024 articles Posterior reversible leukoencephalopathy syndrome Scopus articles Posterior reversible leukoencephalopathy syndrome impact factor journals Posterior reversible leukoencephalopathy syndrome Scopus journals Posterior reversible leukoencephalopathy syndrome PubMed journals Posterior reversible leukoencephalopathy syndrome medical journals Posterior reversible leukoencephalopathy syndrome free journals Posterior reversible leukoencephalopathy syndrome best journals Posterior reversible leukoencephalopathy syndrome top journals Posterior reversible leukoencephalopathy syndrome free medical journals Posterior reversible leukoencephalopathy syndrome famous journals Posterior reversible leukoencephalopathy syndrome Google Scholar indexed journals leukoencephalopathy articles leukoencephalopathy Research articles leukoencephalopathy review articles leukoencephalopathy PubMed articles leukoencephalopathy PubMed Central articles leukoencephalopathy 2023 articles leukoencephalopathy 2024 articles leukoencephalopathy Scopus articles leukoencephalopathy impact factor journals leukoencephalopathy Scopus journals leukoencephalopathy PubMed journals leukoencephalopathy medical journals leukoencephalopathy free journals leukoencephalopathy best journals leukoencephalopathy top journals leukoencephalopathy free medical journals leukoencephalopathy famous journals leukoencephalopathy Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals Neurology articles Neurology Research articles Neurology review articles Neurology PubMed articles Neurology PubMed Central articles Neurology 2023 articles Neurology 2024 articles Neurology Scopus articles Neurology impact factor journals Neurology Scopus journals Neurology PubMed journals Neurology medical journals Neurology free journals Neurology best journals Neurology top journals Neurology free medical journals Neurology famous journals Neurology Google Scholar indexed journals Neurosurgery articles Neurosurgery Research articles Neurosurgery review articles Neurosurgery PubMed articles Neurosurgery PubMed Central articles Neurosurgery 2023 articles Neurosurgery 2024 articles Neurosurgery Scopus articles Neurosurgery impact factor journals Neurosurgery Scopus journals Neurosurgery PubMed journals Neurosurgery medical journals Neurosurgery free journals Neurosurgery best journals Neurosurgery top journals Neurosurgery free medical journals Neurosurgery famous journals Neurosurgery Google Scholar indexed journals Mechanical atherothrombectomy articles Mechanical atherothrombectomy Research articles Mechanical atherothrombectomy review articles Mechanical atherothrombectomy PubMed articles Mechanical atherothrombectomy PubMed Central articles Mechanical atherothrombectomy 2023 articles Mechanical atherothrombectomy 2024 articles Mechanical atherothrombectomy Scopus articles Mechanical atherothrombectomy impact factor journals Mechanical atherothrombectomy Scopus journals Mechanical atherothrombectomy PubMed journals Mechanical atherothrombectomy medical journals Mechanical atherothrombectomy free journals Mechanical atherothrombectomy best journals Mechanical atherothrombectomy top journals Mechanical atherothrombectomy free medical journals Mechanical atherothrombectomy famous journals Mechanical atherothrombectomy Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals
Article Details
1. Introduction
Posterior reversible leukoencephalopathy syndrome (PRES) is a brain disorder that affects the cerebral white matter and usually presents with symptoms of headache, nausea and vomiting, seizures and visual disturbance [1]. It tends to be found in patients with renal failure, extreme fluctuations of blood pressure, eclampsia, autoimmune conditions or who are taking cytotoxic drugs/immunosuppressants. The pathology has not yet fully been described however it seems to be linked to endothelial dysfunction [2]. Very few cases have been described in which PRES has presented with hydrocephalus, particularly in adults [3]. We present a case of PRES which presented with hydrocephalus in a 46 year old female managed in Newcastle Upon Tyne Hospitals.
2. Case Report
The patient is a 46 year old female who presented with a 3 day history of vomiting and headache. Her CT scan demonstrated hydrocephalus and she was transferred to the regional specialist neurosciences unit for neurology and neurosurgery. She was hypertensive at 273/150 prior to transfer and 188/120 on arrival. An external ventricular drain (EVD) was fitted by the neurosurgical team on transfer and the patients blood pressure was lowered with a combination of amlodipine, bisoprolol and doxazosin. A MRI brain showed patchy and early confluent T2 hyperintensity associated with swelling affecting the pons, cerebellum, midbrain, deep grey nuclei and less extensively the supratentorial white matter consistent with a diagnosis of PRES. After tight control of blood pressure the patient recovered well, the EVD was removed and she was discharged (Figures 1 and 2).
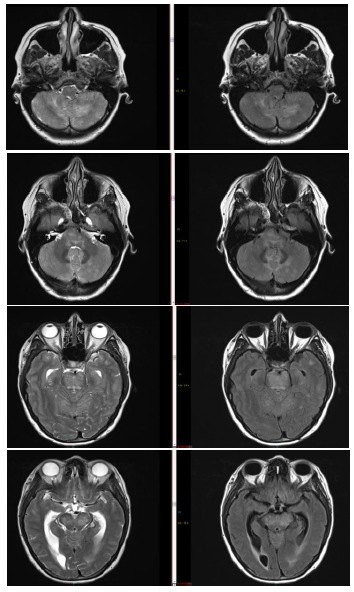
Figure 1: Pre-treatment showing patchy changes (Images 1-8).
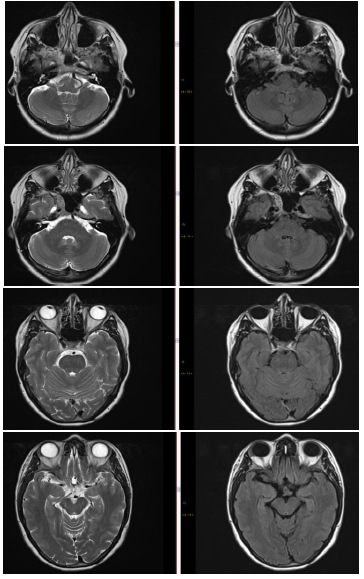
Figure 2: Post-treatment showing resolution of patchy changes (Images 1-8).
3. Discussion
Very few cases of PRES presenting with hydrocephalus have been described, particularly in adults. Searching PubMed with the keywords “posterior reversible encephalopathy syndrome” “PRES” “hydrocephalus” and “adult” yielded 8 papers discussing cases where hydrocephalus was identified in adults. Of these cases, the main precipitating factor was hypertension, with cases reporting immunosuppressive therapy [4], renal hypouricaemia [5] or, in one case, subarachnoid haemorrhage with an over-draining ventriculo-peritoneal shunt leading to PRES [6].
Variations of PRES are also beginning to be described since the first case of PRES was reported in 1996. Since infratentorial variations of PRES, such as the case reported here, have been illustrated with rapid rises in blood pressure, leading to oedema focused around the brainstem and cerebellum. The majority of these cases, however, have been in younger males rather than females, the reason for which is still not understood [7]. Development of oedema in the infratentorial region and especially the brain stem could explain why hydrocephalus develops, where oedematous tissues cause compression of the ventricular system thus blocking outflow. The management described in the 8 cases with concurrent hydrocephalus varied. The patients were treated either medically with surgical intervention such as external ventricular drain insertion [8, 9] or by cranial decompression [3, 10], or medically alone with best supportive care including anti-hypertensive therapy and withdrawal of immune suppressants if used [4, 5, 8, 11].
All treatments had positive outcomes with a seemingly full resolution of oedema within the parenchyma and reversal of hydrocephalus, but comparison between medical and surgical management is difficult to make as there is no long term follow up or randomisation of treatment given. Based on the cases reported, surgical approach alone was not sufficient and the initiating process, be it hypertension, immunosuppression or renal causes, needed to be treated to remove the precipitant. However the question remains that if the precipitant is identified and treated quickly, would the need for surgery be removed, or is decompression still necessary in the short term to prevent long term irreversible changes. Given the rarity of PRES, the chances to perform randomised trial are limited, however more research is required to improve our understanding of the best way to manage the condition when it presents in this way.
References
- Garg RK. Posterior leukoencephalopathy syndrome. Postgraduate Medical Journal 77 (2001): 24.
- Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions. The Lancet Neurology 14 (2015): 914-925.
- Grossbach AJ, Abel TJ, Hodis B, et al. Hypertensive posterior reversible encephalopathy syndrome causing posterior fossa edema and hydrocephalus. Journal of Clinical Neuroscience 21 (2014): 207-211.
- Naval PB, Martínez TF, Mora P, et al. Posterior reversible encephalopathy syndrome (PRES) with obstructive hydrocephalus. Diagnostic and interventional imaging 98 (2017): 745-746.
- Mou LJ, Jiang LP, Hu Y. A novel homozygous GLUT9 mutation cause recurrent exercise-induced acute renal failure and posterior reversible encephalopathy syndrome. Journal of nephrology 28 (2015): 387-392.
- Sato H, Koizumi T, Sato D, et al. Unilateral posterior reversible encephalopathy syndrome after ventriculo-peritoneal shunt for normal pressure hydrocephalus following subarachnoid hemorrhage: A Case report. No shinkei geka. Neurological surgery 44 (2016): 507-515.
- Ou S, Xia L, Wang L, et al. Posterior reversible encephalopathy syndrome with isolated involving infratentorial structures. Frontiers in neurology (2018): 9.
- Li D, Lian L, Zhu S. Isolated cerebellar involvement in posterior reversible encephalopathy syndrome. Journal of the neurological sciences 357 (2015): 101-105.
- Lee SY, Dinesh SK, Thomas J. Hypertension-induced reversible posterior leukoencephalopathy syndrome causing obstructive hydrocephalus. Journal of Clinical Neuroscience 15 (2008): 457-459.
- Abusabha Y, Petridis AK, Kraus B, et al. Life-threatening posterior reversible encephalopathy syndrome in the cerebellum treated by posterior fossa decompression. Acta neurochirurgica 159 (2017): 1325-1328.
- Togni M, Müller NJ, Sartoretti S, et al. Reversible posterior leukoencephalopathy: significance in everyday clinical practice. Schweizerische medizinische Wochenschrift 127 (1997): 1242-1246.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
