Knee Mega-Prosthesis in the Management of Complex Knee Fracture of the Elderly a Case Series and Review of the Literature
Article Information
Soufiane Aharram1,*, Jawad Amghar1, Mounir Yahyaoui1, Omar Agoumi2, Abdelkarim Daoudi3
1Faculty of Medicine and Pharmacy of Oujda , Department of traumatology orthopeadic surgery, CHU Mohammed VI, Oujda, Morocco
2Associate professor of orthopaedic and trauma surgery, Faculty of Medicine and Pharmacy of Oujda, Department of traumatology orthopeadic surgery, CHU Mohammed VI, Oujda, Morocco
3Professor of higher education in orthopaedic surgery and traumatology, Faculty of Medicine and Pharmacy of Oujda, Department of traumatology orthopeadic surgery, CHU Mohammed VI, Oujda, Morocco
*Corresponding Author: Dr. Soufiane Aharram, Faculty of Medicine and Pharmacy of Oujda , Department of traumatology orthopeadic surgery, CHU Mohammed VI, Oujda, Morocco
Received: 11 July 2020; Accepted: 17 July 2020; Published: 02 January 2021
Citation: Soufiane Aharram, Jawad Amghar, Mounir Yahyaoui, Omar Agoumi, Abdelkarim Daoudi. Knee Mega-Prosthesis in the Management of Complex Knee Fracture of the Elderly a Case Series and Review of the Literature. Journal of Orthopaedics and Sports Medicine 3 (2021): 197-203.
View / Download Pdf Share at FacebookAbstract
Purpose: the goal of this paper is to share our experience with the use of mega knee-prosthesis as a treatment option for complex DFF in the elderly patient and do a review the literature.
Methods: we operated 4 patients with complex DFF using a mega knee-prosthesis. All patients were operated by one senior surgeon. No patients were lost at follow-up. One patient died 7 months after the surgery from flu. All patient were female and the average age at the time of the surgery was 79, 5. Clinical outcomes were measured through the WOMAC, Oxford knee score and pain NRS. Post-operative autonomy was measured using the Parker score. A follow-up radiographic analysis was performed independently by the surgeon and a radiologist.
Results: At an average follow-up of 2,3 years (range, 0,6 to 4,2 years), the average Western Ontario and McMaster Universities Osteoarthritis index (WOMAC) was 17,25 (range, 7 to 37), the average Oxford knee score was 35,25 (range, 25 to 41) and the average pain Numerical Rating Scale (NRS) was 0,5 (range, 0 to 1).
Conclusion: The use of cemented knee mega-prosthesis for complex intra-articular distal femoral fractures is a viable treatment option in elderly patient with osteoporotic bone as it allows immediate full weight bearing and a rapid return to pre-operative functional status.
Keywords
Distal femur fracture (DEF); Arthroplasty; Knee megaprosthesis; Complex fracture
Knee Mega-Prosthesis articles Knee Mega-Prosthesis Research articles Knee Mega-Prosthesis review articles Knee Mega-Prosthesis PubMed articles Knee Mega-Prosthesis PubMed Central articles Knee Mega-Prosthesis 2023 articles Knee Mega-Prosthesis 2024 articles Knee Mega-Prosthesis Scopus articles Knee Mega-Prosthesis impact factor journals Knee Mega-Prosthesis Scopus journals Knee Mega-Prosthesis PubMed journals Knee Mega-Prosthesis medical journals Knee Mega-Prosthesis free journals Knee Mega-Prosthesis best journals Knee Mega-Prosthesis top journals Knee Mega-Prosthesis free medical journals Knee Mega-Prosthesis famous journals Knee Mega-Prosthesis Google Scholar indexed journals Traumatology articles Traumatology Research articles Traumatology review articles Traumatology PubMed articles Traumatology PubMed Central articles Traumatology 2023 articles Traumatology 2024 articles Traumatology Scopus articles Traumatology impact factor journals Traumatology Scopus journals Traumatology PubMed journals Traumatology medical journals Traumatology free journals Traumatology best journals Traumatology top journals Traumatology free medical journals Traumatology famous journals Traumatology Google Scholar indexed journals Distal femur fracture articles Distal femur fracture Research articles Distal femur fracture review articles Distal femur fracture PubMed articles Distal femur fracture PubMed Central articles Distal femur fracture 2023 articles Distal femur fracture 2024 articles Distal femur fracture Scopus articles Distal femur fracture impact factor journals Distal femur fracture Scopus journals Distal femur fracture PubMed journals Distal femur fracture medical journals Distal femur fracture free journals Distal femur fracture best journals Distal femur fracture top journals Distal femur fracture free medical journals Distal femur fracture famous journals Distal femur fracture Google Scholar indexed journals Orthopeadic surgery articles Orthopeadic surgery Research articles Orthopeadic surgery review articles Orthopeadic surgery PubMed articles Orthopeadic surgery PubMed Central articles Orthopeadic surgery 2023 articles Orthopeadic surgery 2024 articles Orthopeadic surgery Scopus articles Orthopeadic surgery impact factor journals Orthopeadic surgery Scopus journals Orthopeadic surgery PubMed journals Orthopeadic surgery medical journals Orthopeadic surgery free journals Orthopeadic surgery best journals Orthopeadic surgery top journals Orthopeadic surgery free medical journals Orthopeadic surgery famous journals Orthopeadic surgery Google Scholar indexed journals Trauma surgery articles Trauma surgery Research articles Trauma surgery review articles Trauma surgery PubMed articles Trauma surgery PubMed Central articles Trauma surgery 2023 articles Trauma surgery 2024 articles Trauma surgery Scopus articles Trauma surgery impact factor journals Trauma surgery Scopus journals Trauma surgery PubMed journals Trauma surgery medical journals Trauma surgery free journals Trauma surgery best journals Trauma surgery top journals Trauma surgery free medical journals Trauma surgery famous journals Trauma surgery Google Scholar indexed journals Osteoporosis articles Osteoporosis Research articles Osteoporosis review articles Osteoporosis PubMed articles Osteoporosis PubMed Central articles Osteoporosis 2023 articles Osteoporosis 2024 articles Osteoporosis Scopus articles Osteoporosis impact factor journals Osteoporosis Scopus journals Osteoporosis PubMed journals Osteoporosis medical journals Osteoporosis free journals Osteoporosis best journals Osteoporosis top journals Osteoporosis free medical journals Osteoporosis famous journals Osteoporosis Google Scholar indexed journals Knee fracture articles Knee fracture Research articles Knee fracture review articles Knee fracture PubMed articles Knee fracture PubMed Central articles Knee fracture 2023 articles Knee fracture 2024 articles Knee fracture Scopus articles Knee fracture impact factor journals Knee fracture Scopus journals Knee fracture PubMed journals Knee fracture medical journals Knee fracture free journals Knee fracture best journals Knee fracture top journals Knee fracture free medical journals Knee fracture famous journals Knee fracture Google Scholar indexed journals Mega-prosthetic implants articles Mega-prosthetic implants Research articles Mega-prosthetic implants review articles Mega-prosthetic implants PubMed articles Mega-prosthetic implants PubMed Central articles Mega-prosthetic implants 2023 articles Mega-prosthetic implants 2024 articles Mega-prosthetic implants Scopus articles Mega-prosthetic implants impact factor journals Mega-prosthetic implants Scopus journals Mega-prosthetic implants PubMed journals Mega-prosthetic implants medical journals Mega-prosthetic implants free journals Mega-prosthetic implants best journals Mega-prosthetic implants top journals Mega-prosthetic implants free medical journals Mega-prosthetic implants famous journals Mega-prosthetic implants Google Scholar indexed journals Osteosynthesefragen articles Osteosynthesefragen Research articles Osteosynthesefragen review articles Osteosynthesefragen PubMed articles Osteosynthesefragen PubMed Central articles Osteosynthesefragen 2023 articles Osteosynthesefragen 2024 articles Osteosynthesefragen Scopus articles Osteosynthesefragen impact factor journals Osteosynthesefragen Scopus journals Osteosynthesefragen PubMed journals Osteosynthesefragen medical journals Osteosynthesefragen free journals Osteosynthesefragen best journals Osteosynthesefragen top journals Osteosynthesefragen free medical journals Osteosynthesefragen famous journals Osteosynthesefragen Google Scholar indexed journals Spinal anesthesia articles Spinal anesthesia Research articles Spinal anesthesia review articles Spinal anesthesia PubMed articles Spinal anesthesia PubMed Central articles Spinal anesthesia 2023 articles Spinal anesthesia 2024 articles Spinal anesthesia Scopus articles Spinal anesthesia impact factor journals Spinal anesthesia Scopus journals Spinal anesthesia PubMed journals Spinal anesthesia medical journals Spinal anesthesia free journals Spinal anesthesia best journals Spinal anesthesia top journals Spinal anesthesia free medical journals Spinal anesthesia famous journals Spinal anesthesia Google Scholar indexed journals Venous thromboembolism articles Venous thromboembolism Research articles Venous thromboembolism review articles Venous thromboembolism PubMed articles Venous thromboembolism PubMed Central articles Venous thromboembolism 2023 articles Venous thromboembolism 2024 articles Venous thromboembolism Scopus articles Venous thromboembolism impact factor journals Venous thromboembolism Scopus journals Venous thromboembolism PubMed journals Venous thromboembolism medical journals Venous thromboembolism free journals Venous thromboembolism best journals Venous thromboembolism top journals Venous thromboembolism free medical journals Venous thromboembolism famous journals Venous thromboembolism Google Scholar indexed journals Minimally invasive percutaneous plate osteosynthesis articles Minimally invasive percutaneous plate osteosynthesis Research articles Minimally invasive percutaneous plate osteosynthesis review articles Minimally invasive percutaneous plate osteosynthesis PubMed articles Minimally invasive percutaneous plate osteosynthesis PubMed Central articles Minimally invasive percutaneous plate osteosynthesis 2023 articles Minimally invasive percutaneous plate osteosynthesis 2024 articles Minimally invasive percutaneous plate osteosynthesis Scopus articles Minimally invasive percutaneous plate osteosynthesis impact factor journals Minimally invasive percutaneous plate osteosynthesis Scopus journals Minimally invasive percutaneous plate osteosynthesis PubMed journals Minimally invasive percutaneous plate osteosynthesis medical journals Minimally invasive percutaneous plate osteosynthesis free journals Minimally invasive percutaneous plate osteosynthesis best journals Minimally invasive percutaneous plate osteosynthesis top journals Minimally invasive percutaneous plate osteosynthesis free medical journals Minimally invasive percutaneous plate osteosynthesis famous journals Minimally invasive percutaneous plate osteosynthesis Google Scholar indexed journals Sarcopenia articles Sarcopenia Research articles Sarcopenia review articles Sarcopenia PubMed articles Sarcopenia PubMed Central articles Sarcopenia 2023 articles Sarcopenia 2024 articles Sarcopenia Scopus articles Sarcopenia impact factor journals Sarcopenia Scopus journals Sarcopenia PubMed journals Sarcopenia medical journals Sarcopenia free journals Sarcopenia best journals Sarcopenia top journals Sarcopenia free medical journals Sarcopenia famous journals Sarcopenia Google Scholar indexed journals Knee arthritis articles Knee arthritis Research articles Knee arthritis review articles Knee arthritis PubMed articles Knee arthritis PubMed Central articles Knee arthritis 2023 articles Knee arthritis 2024 articles Knee arthritis Scopus articles Knee arthritis impact factor journals Knee arthritis Scopus journals Knee arthritis PubMed journals Knee arthritis medical journals Knee arthritis free journals Knee arthritis best journals Knee arthritis top journals Knee arthritis free medical journals Knee arthritis famous journals Knee arthritis Google Scholar indexed journals Supracondylar fracture articles Supracondylar fracture Research articles Supracondylar fracture review articles Supracondylar fracture PubMed articles Supracondylar fracture PubMed Central articles Supracondylar fracture 2023 articles Supracondylar fracture 2024 articles Supracondylar fracture Scopus articles Supracondylar fracture impact factor journals Supracondylar fracture Scopus journals Supracondylar fracture PubMed journals Supracondylar fracture medical journals Supracondylar fracture free journals Supracondylar fracture best journals Supracondylar fracture top journals Supracondylar fracture free medical journals Supracondylar fracture famous journals Supracondylar fracture Google Scholar indexed journals
Article Details
1. Introduction
Distal femur fracture (DFF) account for 0,4% of all adult fractures and 3% of femoral fractures. The annual incidence is 4,5 per 100.000 adults with a male-to-female ratio of 1:2. They typically present in a bimodal distribution as either young male patients with high-energy trauma or elderly female patients with low-energy trauma related to osteoporosis [1]. Supracondylar fracture of the elderly can be very challenging to treat and total knee replacement is often not considered. Mega-prosthetic implants were first introduced in oncological orthopedic surgery as a treatment for tumors requiring massive bone resections [2]. Osteoporosis, comorbidities and lower pre-injury activity of the elderly alter the outcome of ORIF compared to a younger population [3-4]. The goal of this paper is to share our experience with the use of mega knee-prosthesis as a treatment option for complex DFF in the elderly patient and do a review the literature.
2. Material and Methods
From September 2015 to October 2019, we operated 4 patients with complex DFF using a mega knee-prosthesis. All patients were operated by one senior surgeon. No patients were lost at follow-up.
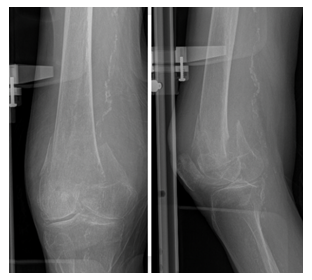
Figure 1: Plain radiographs of the right knee showing a complex DFF.
One patient died 7 months after the surgery from flu. All patient were female and the average age at the time of the surgery was 79, 5 (range, 69 to 95 years). The Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification was used to classify the fractures [5]. All patients had computed tomography scan preoperatively that showed DFF AO33C3 with severe comminution (Figure 1). None of the knees were previously operated. All patients were autonomous pre-operatively and lived at home. All patients had osteoporosis and 2 patients had underlying knee arthritis.
The surgery was on average done 6,5 days after the trauma (range, 6 to 7 days). 3 patients were immobilized by an extension knee brace prior to surgery and one benefited from an external fixator of the knee on the day of the trauma. Clinical outcomes were measured through the WOMAC, Oxford knee score and pain NRS. Post-operative autonomy was measured using the Parker score. A follow-up radiographic analysis was performed independently by the surgeon and a radiologist.
2.1 Surgical technique
The surgery was performed under general or spinal anesthesia combined with nerve blocks. A tourniquet was placed but not inflated. Patients received 1g of intravenous tranexamic acid 30 minutes prior to the incision. A standard midline incision and medial parapatellar approach were utilized for all surgical procedures. The implant used for all cases was the cemented OSSTM Orthopaedic Salvage System (Zimmer Biomet, Warsaw, Indiana, USA) (Figure2).
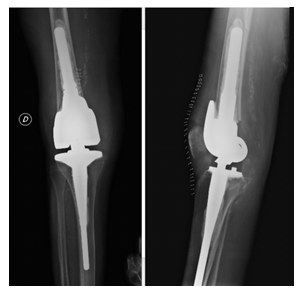
Figure 2: Postoperative plain radiographs of the right knee after treatment by knee mega-prosthesis.
Physiotherapy was started on the first day after the surgery, with mobilization of the knee in bed and walking as soon as possible. All patients were permitted to bear full weight postoperatively and had to use a walker during the hospital stay. All patients were instructed to take enoxaparine 40mg once a day for 30 days for postoperative chemoprophylaxis against venous thromboembolism. Clinical and radiographic evaluations were made at 2 weeks, 6 weeks, 6 month and 1 year after the surgery. For the purpose of this paper all patients were convoked for clinical and radiological assessment.
3. Results
At an average follow-up of 2,3 years (range, 0,6 to 4,2 years), the average Western Ontario and McMaster Universities Osteoarthritis index (WOMAC) was 17,25 (range, 7 to 37), the average Oxford knee score was 35,25 (range, 25 to 41) and the average pain Numerical Rating Scale (NRS) was 0,5 (range, 0 to 1). 3 patients were discharged to inpatients rehabilitation facilities and 1 returned home. Average length of hospital stay was 14, 75 days (range, 12 to 18 days).
(Table1) On average the first walk above 5 meters was 5, 25 days after the surgery (range, 3 to 7 days). The autonomy of the patient was assessed using the parker score, at an average follow-up of 2, 3 years, 1.75 points were lost (range, 1 to 3). The average range of motion (ROM) was 0/117, 5 degrees (range, 0/100 to 0/135degrees) (Table 2). On the radiographic analyses no aseptic loosening, fracture or migration of the implant was found.
|
Table 1 |
Age |
ASA score |
Time to OR (days) |
Type of anesthesia |
Complications |
LOS in days |
Walk >5m |
Discharged to: |
|
Patient 1 |
69 |
3 |
Day 7 |
EA + FNB |
Urinary tract infection + Postoperative Anemia |
17 |
Day 3 |
Home |
|
Patient 2 |
72 |
3 |
Day 7 |
GA + FNB |
Postoperative Anemia |
12 |
Day 5 |
RC |
|
Patient 3 |
95 |
3 |
Day 6 |
GA + FNB |
Confusion + Postoperative Anemia |
18 |
Day 7 |
RC |
|
Patient 4 |
82 |
3 |
Day 6 |
EA + FNB |
Postoperative Anemia |
12 |
Day 6 |
RC |
Abbreviations:
American Society of Anesthesiologists, ASA; Operating room, OR; Epidural Anesthesia, EA; General anesthesia, GA; femoral nerve block, FNB; LOS, length of stay; rehabilitation center, RC; meter, m.
Table 1: Summary of patient’s characteristics and surgical particularities.
|
Table 2 |
Preoperative Parker score |
Postoperative Parker score |
Oxford score |
WOMAC score |
NRS |
ROM in degrees |
Follow-up in month |
|
Patient 1 |
8 |
7 |
36 |
17 |
1 |
0/110 |
42 |
|
Patient 2 |
9 |
7 |
39 |
8 |
0 |
0/135 |
51 |
|
Patient 3 |
8 |
5 |
25 |
37 |
1 |
0/100 |
7 |
|
Patient 4 |
9 |
8 |
41 |
7 |
0 |
0/125 |
12 |
Table 2: Results of the different clinical outcome scores and range of motion (ROM) achieved postoperatively.
3.1 Complications
One patient suffered from a urinary tract infection treated with antibiotics. 3 patients had postoperative anemia that required blood transfusion. One patient was confused for 3 days following surgery. Neither mechanical nor implant related complication occurred to this day.
4. Discussion
It has been accepted and demonstrated for quite some time that better results and fewer complications were achieved with surgical treatment for displaced DFF compared with conservative treatment as Butt and al. showed in 1996 [3]. Different fixation techniques such as plating, intramedullary retrograde nailing and external fixation have been described and validated for the treatment of DFF [6]. Locking plated inserted using a minimally invasive percutaneous plate osteosynthesis (MIPPO) approach is now the most common treatment method and shows better results for complications occurrence and union rates [7].
But the management of the elderly population with supracondylar fractures continues to pose a challenge compared to younger patients. A retrospective study by Henderson and al. analyzing the complications of locked plating for DFF showed 20% of non-union and 27% of re-operation for a population with a mean age of 60 [8]. The use of tumor endoprosthesis for DFF has been described for the first time in 1982 [9] and the first studies were published in 1992 [10-11]. To our knowledge just a handful of studies regarding the management of DFF of the elderly with knee mega-prosthesis have been published since. Pour et al. [12] concluded in their retrospective study that rotated hinged prosthesis should be considered as a salvage device and should be used primarily for the elderly and sedentary patients with complex knee problems.
We agree that their use in traumatology shouldn’t be routinized but this technique can also benefit active elderly patients for whom immediate full-weight-bearing could diminish a loss of autonomy and complications due to prolonged decubitus such as bedsores, thromboembolic disease, pneumonia, loss of autonomy and sarcopenia [3]. We used this technique for elderly autonomous patients with complicated DFF, osteoporotic bone and preferably with radiological signs of arthritis.
Osteoarthritis following ORIF of intra-articular DFF can occur in up to 50% of the patient at 6 years follow-up [13-14]. For this reason, the OSSTM could be used for DFF on knee without osteoarthritis. Freedman et al. [15] published a study on 8 DFF with a mean follow-up of 49 month. They reported similar results to ours with a good radiologic outcome and a mean range of motion of 114, 3 degrees. In a study published by Bettin et al. [16] the mean WOMAC score at 1.7 years follow-up on average was 23.1 which are similar to our results of 17.25. High rates of complications associated with the use of knee mega-prosthesis for nonneoplasic surgery are found in the literature with 22% of patellar instability [17], up to 20% of aseptic loosening and deep infections ranging from 14,5 to 19,2% [12, 17].
In our case series the only surgery related complication that occurred was postoperative anemia. However longer follow-up is needed to asses long-term complications such as aseptic loosening and deep infections. As Bettin et al. [16] rightfully mentioned in their article, the cost of the mega-prosthetic implant is significant but might still be cheaper that a failed ORIF requiring additional hospitalization and revision arthroplasty components. Limitations of this study included those inherent to its retrospective design, the low number of patients, the relatively short follow-up and the lack of control group for comparison. A prospective, randomized trial comparing the use of primary cemented knee mega-prosthesis and MIPPO locked plating is needed to address the merits of each method.
5. Conclusion
The use of cemented knee mega-prosthesis for complex intra-articular distal femoral fractures is a viable treatment option in elderly patient with osteoporotic bone as it allows immediate full weight bearing and a rapid return to pre-operative functional status. Because of the high rates of complication found in the literature, patients should be carefully selected.
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
There is no source of funding.
Ethical Approval
This article does not contain any studies by any of the authors involving human or animal participants.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review.Injury 37 (2006): 691-697.
- Gautam D, Malhotra R. Megaprosthesis versus Allograft Prosthesis Composite for massive skeletal defects.J Clin Orthop Trauma 9 (2018): 63-80.
- Butt MS, Krikler SJ, Ali MS. Displaced fractures of the distal femur in elderly patients. Operative versus non-operative treatment.J Bone Joint Surg Br 78 (1996): 110-114.
- Karpman RR, Del Mar NB. Supracondylar femoral fractures in the frail elderly. Fractures in need of treatment. Clin Orthop Relat Res 316 (1995): 21-24.
- The compendium is branded as the AO/OTA or OTA/AO Fracture and Dislocation Classification Compendium. In publications, it will be cited as Meinberg E, Agel J, Roberts C, et al. Fracture and Dislocation Classification Compendium–2018,Journal of Orthopaedic Trauma 32 (2018).
- Meluzio MC, Oliva MS, Minutillo F, et al. The use of knee mega-prosthesis for the management of distal femoral fractures: A systematic review [published online ahead of print, Aug 13].Injury S0020-1383 (2019): 30473-30475.
- Kregor PJ, Stannard JA, Zlowodzki M, et al. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures.J Orthop Trauma 18 (2004): 509-520.
- Henderson CE, Lujan TJ, Kuhl LL, et al. 2010 mid-America Orthopaedic Association Physician in Training Award: healing complications are common after locked plating for distal femur fractures.Clin Orthop Relat Res 469 (2011): 1757-1765.
- Wolfgang GL. Primary total knee arthroplasty for intercondylar fracture of the femur in a rheumatoid arthritis patient. A case report.Clin Orthop Relat Res (1982): 80-82.
- Wolf LR, Rothman RH, Hozack WJ, et al. Primary total knee arthroplasty for displaced, acute intraarticular knee fractures. A report of four cases. Clin Orthop Relat Res. Mar (1992): 229-236.
- Bell KM, Johnstone AJ, Court-Brown CM, et al. Primary knee arthroplasty for distal femoral fractures in elderly patients. J Bone Joint Surg Br. May 74 (1992): 400-402.
- Pour AE, Parvizi J, Slenker N, et al. Rotating hinged total knee replacement: use with caution.J Bone Joint Surg Am 89 (2007): 1735-1741.
- Rodriguez EK, Boulton C, Weaver MJ, et al. Predictive factors of distal femoral fracture nonunion after lateral locked plating: a retrospective multicenter case-control study of 283 fractures.Injury 45 (2014): 554-559.
- Pettine KA. Supracondylar fractures of the femur: long-term follow-up of closed versus nonrigid internal fixation.Contemp Orthop 21 (1990): 253-261.
- Freedman EL, Hak DJ, Johnson EE, et al. Total knee replacement including a modular distal femoral component in elderly patients with acute fracture or nonunion.J Orthop Trauma 9 (1995): 231-237.
- Bettin CC, Weinlein JC, Toy PC, et al. Distal Femoral Replacement for Acute Distal Femoral Fractures in Elderly Patients.J Orthop Trauma 30 (2016): 503-509.
- Rand JA, Chao EY, Stauffer RN. Kinematic rotating-hinge total knee arthroplasty.J Bone Joint Surg Am 69 (1987): 489-497.


 Impact Factor: * 4.3
Impact Factor: * 4.3 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 