Melasma (Chloasma): Pathogenesis and Treatment
Article Information
Fariyal Hoque1*, John McGrath2, Syed Ebeny Shaude3
1Ex-student MSc, Department of Clinical Dermatology, King’s College London, The United Kingdom
2Head, Department of Molecular Dermatology, King’s College London, The United Kingdom
3Chief coordinator, Department of Research, International Network of Doctors Journal, Dhaka, Bangladesh
*Corresponding author: Fariyal Hoque, Ex-student MSc, Department of Clinical Dermatology, King’s College London, The United Kingdom.
Received: 14 November 2022; Accepted: 21 November 2022; Published: 25 November 2022
Citation: Fariyal Hoque, John McGrath, Syed Ebeny Shaude. Melasma (Chloasma): Pathogenesis and Treatment. Journal of Biotechnology and Biomedicine 5 (2022): 236-243.
View / Download Pdf Share at FacebookAbstract
Background: Now-a-days melasma is a common pigmentary condition, particularly among Asians, and its treatment is challenging for dermatologists because of unsatisfactory responses and high recurrence rates in many patients.
Objectives: This dissertation provides an overview of the aetiology and pathogenesis of melasma, followed by a focus on its current management.
Methodology: This dissertation is based on a comprehensive literature search, identifying relevant articles using Ovid, PubMed, and Google Scholar. For the therapy section the data mainly involve a critical review of published randomized controlled trials. Various studies from sample groups of different ethnicities, age groups, and gender, were evaluated.
Clinical trial findings: Being an uncommon skin hyperpigmentation condition melasma now has become a serious problem especially among dark skinned population. Although the exact cause or pathogenesis of this condition is still 7 poorly understood, new data identifying proteins, RNAs and micro-RNAs implicated in melanocyte cell biology and extracellular matrix homeostasis and signalling pathways linked to melasma, may contribute towards novel treatments for melasma which may bring more positive results and better prevention of relapse. Currently, most available treatments for melasma are not showing effective or sustained outcomes. The ongoing treatments of melasma include regular UV protection, topical medicines, oral treatments, chemical peels, some clinical procedures, LASER sessions and light-based therapies. For dermatologists, optimal use of current treatment modalities should be directed by clinical trials data and evidence-based medicine.
Conclusions: Although Melasma is caused by several factors like genetics, sunlight exposure, female sex hormones, thyroid problems, anticonvulsant medication and cosmetic items, the main
Keywords
Azelaic acid; Glycolic acid; Hydroquinone; Kojic acid; Lactic acid
Azelaic acid articles Azelaic acid Research articles Azelaic acid review articles Azelaic acid PubMed articles Azelaic acid PubMed Central articles Azelaic acid 2023 articles Azelaic acid 2024 articles Azelaic acid Scopus articles Azelaic acid impact factor journals Azelaic acid Scopus journals Azelaic acid PubMed journals Azelaic acid medical journals Azelaic acid free journals Azelaic acid best journals Azelaic acid top journals Azelaic acid free medical journals Azelaic acid famous journals Azelaic acid Google Scholar indexed journals Glycolic acid articles Glycolic acid Research articles Glycolic acid review articles Glycolic acid PubMed articles Glycolic acid PubMed Central articles Glycolic acid 2023 articles Glycolic acid 2024 articles Glycolic acid Scopus articles Glycolic acid impact factor journals Glycolic acid Scopus journals Glycolic acid PubMed journals Glycolic acid medical journals Glycolic acid free journals Glycolic acid best journals Glycolic acid top journals Glycolic acid free medical journals Glycolic acid famous journals Glycolic acid Google Scholar indexed journals Hydroquinone articles Hydroquinone Research articles Hydroquinone review articles Hydroquinone PubMed articles Hydroquinone PubMed Central articles Hydroquinone 2023 articles Hydroquinone 2024 articles Hydroquinone Scopus articles Hydroquinone impact factor journals Hydroquinone Scopus journals Hydroquinone PubMed journals Hydroquinone medical journals Hydroquinone free journals Hydroquinone best journals Hydroquinone top journals Hydroquinone free medical journals Hydroquinone famous journals Hydroquinone Google Scholar indexed journals Kojic acid articles Kojic acid Research articles Kojic acid review articles Kojic acid PubMed articles Kojic acid PubMed Central articles Kojic acid 2023 articles Kojic acid 2024 articles Kojic acid Scopus articles Kojic acid impact factor journals Kojic acid Scopus journals Kojic acid PubMed journals Kojic acid medical journals Kojic acid free journals Kojic acid best journals Kojic acid top journals Kojic acid free medical journals Kojic acid famous journals Kojic acid Google Scholar indexed journals Lactic acid articles Lactic acid Research articles Lactic acid review articles Lactic acid PubMed articles Lactic acid PubMed Central articles Lactic acid 2023 articles Lactic acid 2024 articles Lactic acid Scopus articles Lactic acid impact factor journals Lactic acid Scopus journals Lactic acid PubMed journals Lactic acid medical journals Lactic acid free journals Lactic acid best journals Lactic acid top journals Lactic acid free medical journals Lactic acid famous journals Lactic acid Google Scholar indexed journals Melasma articles Melasma Research articles Melasma review articles Melasma PubMed articles Melasma PubMed Central articles Melasma 2023 articles Melasma 2024 articles Melasma Scopus articles Melasma impact factor journals Melasma Scopus journals Melasma PubMed journals Melasma medical journals Melasma free journals Melasma best journals Melasma top journals Melasma free medical journals Melasma famous journals Melasma Google Scholar indexed journals genetics articles genetics Research articles genetics review articles genetics PubMed articles genetics PubMed Central articles genetics 2023 articles genetics 2024 articles genetics Scopus articles genetics impact factor journals genetics Scopus journals genetics PubMed journals genetics medical journals genetics free journals genetics best journals genetics top journals genetics free medical journals genetics famous journals genetics Google Scholar indexed journals homeostasis articles homeostasis Research articles homeostasis review articles homeostasis PubMed articles homeostasis PubMed Central articles homeostasis 2023 articles homeostasis 2024 articles homeostasis Scopus articles homeostasis impact factor journals homeostasis Scopus journals homeostasis PubMed journals homeostasis medical journals homeostasis free journals homeostasis best journals homeostasis top journals homeostasis free medical journals homeostasis famous journals homeostasis Google Scholar indexed journals hyperpigmentation articles hyperpigmentation Research articles hyperpigmentation review articles hyperpigmentation PubMed articles hyperpigmentation PubMed Central articles hyperpigmentation 2023 articles hyperpigmentation 2024 articles hyperpigmentation Scopus articles hyperpigmentation impact factor journals hyperpigmentation Scopus journals hyperpigmentation PubMed journals hyperpigmentation medical journals hyperpigmentation free journals hyperpigmentation best journals hyperpigmentation top journals hyperpigmentation free medical journals hyperpigmentation famous journals hyperpigmentation Google Scholar indexed journals dermatologists articles dermatologists Research articles dermatologists review articles dermatologists PubMed articles dermatologists PubMed Central articles dermatologists 2023 articles dermatologists 2024 articles dermatologists Scopus articles dermatologists impact factor journals dermatologists Scopus journals dermatologists PubMed journals dermatologists medical journals dermatologists free journals dermatologists best journals dermatologists top journals dermatologists free medical journals dermatologists famous journals dermatologists Google Scholar indexed journals
Article Details
1. Introduction
The word Melasma comes from the Greek word ‘melas’ which signifies black. It is also known as ‘pregnancy mask’ or ‘chloasma’, which comes from the word ‘chloazein’ which means green, although greencoloured patches can be rarely seen in this condition. Thus, ‘melasma’ is the preferred expression [1]. Melasma is a chronic acquired hyperpigmentation condition of the skin characterized by irregular brown macules symmetrically distributed across sun-exposed parts of the body, especially the face [2]. Melasma is an increasing aesthetic concern among Nepalese people with Fitzpatrick skin types III-IV [3]. Melasma is a widespread, acquired pattern of symmetrical, light-to-dark brown face hyperpigmentation involving sun-exposed areas of skin. The cheekbones, forehead, nose, upper lip, chin, as well as neck, are all preferences.
Melasma affects many pregnant women, perhaps up to 70%. It is clear that spending time in the sun darkens melasma and avoid spending time in the sun to reduce the appearance of melasma is helpful [4]. Dermatologists should play an important role by informing their patients about the nature of the disease and also explaining that it can be recalcitrant to therapy [5]. Sunscreens were frequently used as medications, and drug therapy had a significant economic impact [3].
2. Clinical Classification
- Centro-facial pattern – This is the most prevalent clinical pattern, accounting for around 76 % of all melasma variants. The forehead, upper lip, chin, cheeks, and nose are all affected by hyperpigmented macules [6].
- Malar pattern: The malar pattern on the face is limited to the malar cheeks, whereas mandibular melasma can be found on the jawline and chin. The latter is thought to be more common in older people and may be linked to severe photodamage [7].
- Mandibular pattern: Malar melasma affects the malar cheeks on the face, whereas mandibular pattern affects the jawline and chin [8].

Figure 1: Centro-facial pattern Origin [6].

Figure 2: Malar Pattern Origin [7].

Figure 3: Mandibular pattern Origin [8].
Apart from these categories, numerous studies classify melasma into two clinical subtypes: centro-facial and peripheral. The lesions in the centrofacial pattern cover the glabella, nasal, zygomatic region, upper lip and chin whereas the peripheral type includes frontotemporal, preauricular and mandibular sites. Additionally, extra-facial melasma refers to melasma that affects sites other than the face, most commonly the forearms and neck. Extra-facial melasma is not a common type. It manifests as dark hyperpigmented blotches with uneven edges in menopausal women or those aged over 50 years [9].
3. Histological Patterns
Melasma is usually classified into 3 histological patterns depending on where the melanin pigment is found: epidermal, dermal, and mixed [10]. The epidermal form, in which melanin is dispersed throughout the epidermis, is the most common.The upper and mid dermis are involved in the dermal type. Many pigment-laden macrophages in the dermis are related to the pigmentation. Both epidermal melanin pigment and dermal melanophages are increased in the mixed type.
4. Aetiology
4.1. Genetic Factors
Genetic factors may play a role in the pathophysiology of melasma, as evidenced by familial and racial predisposition. Patients with darker skin types (IV-VI) are more likely than those with lighter skin types (II-III) to have a family member with melasma (Lee et al., 2015; Ogbechie-Godec et al., 2017). Positive family history rates vary widely between nations, ranging from 10.2% in a Singapore referral center research [11] to 61% in a case-control study in Brazil [2].
4.2. Female Sex hormones
Melasma is caused by fluctuations in particular hormones, which is why it is so common during pregnancy. Melasma can also happen if you start or stop using hormonal contraception, such as birth control pills, or if you start or stop using hormone replacement treatment [12].
4.3. UV Radiation
Sunlight has a direct effect on melanogenic activity. Although there is no concrete evidence of a relation between melasma and UV radiation at this time, similarities in microscopic results of both chronic UV exposure skin and melasma lesional skin support the relevance of UV in melasma pathogenesis. Melasma's clinical sign-symptoms often worsen in the hot weather and improve in the cold weather). [13] Despite using an efficient sunscreen against UV radiation, many patients experience a relapse of melasma throughout the summer. Studies have shown that lower wavelengths of visible light can cause hyperpigmentation in melanocytes via opsin3, a particular sensor [14,15].
4.4. Melasma Pathogenesis (Recently Discovered Factors)
Many histological examinations of melasma condition have revealed a rise in both solar elastosis and dermal mast cells, as well as vascularization and basal membrane alteration [16]. Histamine binds to histamine receptors (H2 receptors) in melanocytes and activates PKA, which increases melanogenesis [17]. UV radiation can activate mast cell tryptase, causing dermal ECM degradation by either increasing fibroblast elastin synthesis or activating promatrix metalloproteases (proMMP). This proMMP, particularly proMMP-9, has the ability to breakdown type IV collagen, resulting in alteration of the basement membrane. Granzyme B, a serine protease that can degrade the ECM, is also expressed by mast cells. TGF-2, fibroblast growth factor-2 (FGF-2), and vascular endothelial growth factor (VEGF) are all secreted by mast cells, which is fascinating. These angiogenic factors can cause vascular proliferation, which is one of melasma's most common characteristics. Solar elastosis does not appear in mast cell-deficient mice despite repeated sunlight exposure. Chronic UV exposure raises the levels of MMP-9 and MMP-2 in the skin, which can alter the basement membrane by destroying type VI and type IV collagen. Skin samples from melasma patients demonstrated basement membrane disruption by 83% via anti-collagen type IV immunohistochemistry and 95.5% via periodic acid-5chiffdianase (D-PAS) immunohistochemistry, according to a histochemical and immunohistochemical analysis. This disturbance in the basement membrane may facilitate the migration of melanin and melanocytes into the dermis, resulting in the formation of melanophages in melasma patients [18].
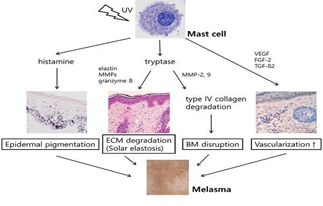
Figure 4: Figure shows the role of mast cell in photoaging and melanogenesis [18].
5. Clinical Assessment
The MASI score is the most widely used metric for determining the severity of melasma and how well it responds to treatment. It calculates a score based on a subjective assessment of three factors: involvement area, darkness, and homogeneity. The forehead, left malar region, right malar region, and chin each account for 30%, 30%, 30%, and 10% of the whole face, respectively [19]. Melasma severity can be assessed using objective measurements. Subjective evaluation scales are the Physician's Global Assessment (PGA), the Melasma Area and Severity Index (MASI), and the Melasma Severity Scale [20]. The psychological impact of this disease must be understood in order to manage it. Melasma Quality of Life Scale (MelasQol) is a validated modified version of the health-related quality of life scale used to assess the impact of melasma on quality of life -(HRQoL) [21,22].
6. MELASQOL Scale Description
On a scale of 1 (not bothered at all) to 7 (bothered all the time), the subject rates how he/she feels about
- The appearance of your skin condition.
- Frustration about your skin condition
- Embarrassment about your skin condition
- Feeling depressed about your skin condition.
- The effects of your skin condition on your interactions with other people
- The effect of your skin condition on your desire to be with people
- Skin condition making it hard to show affection
- Skin discoloration making you feel unattractive to others
- Skin discoloration making you feel less vital or productive
- Skin discoloration affecting your sense of freedom
Score from 7 to 70, with higher score indicating a worse melasma-related health-related quality of life. MELASQOL scale [23]
7. Management of Melasma
7.1. General management
Avoidance of exacerbating factors
UV exposure, hormone therapy, and phototoxic drugs are all examples of phototoxic agents. As a result, it is recommended to avoid or eliminate these factors [24].
7.2. Photoprotection
UV and visible light are both implicated in the aetiology of melasma, according to numerous researches. Avoiding the sun, especially from 10 a.m. to 3 p.m., is an important part of sun protection. Using a broad-spectrum sunscreen with a SPF of 30 or higher, as well as titanium dioxide zinc oxide, a physical blocker, and wearing wide-brimmed hats and protective clothes. While staying outside, sunscreen should be applied once every two hours in an acceptable amount [24,25].
7.3. Role of camouflage
Melasma lesions on the face can have psychosocial consequences for sufferers. Cosmetic: camouflage can be used as a supplement to other treatments. There are numerous options for camouflaging different skin tones. Cosmetic camouflage was found to significantly improve the DLQI in 24 patients with pigmentary disorders in one research. However, covering depigmented or hypopigmented lesions, such as those found in vitiligo, is less challenging than concealing hyperpigmented [24-26].
7.4. Specific treatments
Topical treatments the first-line treatment for melasma is currently topical medicines.
7.5. Hydroquinone (HQ, 1, 4-dihydroxybenttne)
For treating hyperpigmentation, HQ was one of the first agents to be used [27,28]. HQ inhibits tyrosinase, preventing DOPA from being converted to melanin. Moreover, HQ disrupts the assembly of the melanocyte membrane, resulting in melanocyte necrosis [29] Of note, 4% HQ was also said to be superior to 5% ascorbic acid, in a study [30] HQ concentrations range from 2% (over-the-counter in some counties) to 5% (prescription). HQ at a concentration of 2-4% is widely used as a monotherapy or in combination with other treatments. Moreover, 5% HQ can be used in difficult-to-treat cases due to its irritant effects, but it is not suggested for non-refractory cases [31,32].
7.6. Topical retinoid
Tretinoin is a retinoid (RA) that can help with melasma treatment by reducing melanosome transfer, boosting keratinocyte turnover, and increasing the penetration of other topical ingredients [28] One of the most common side effects is retinoid dermatitis
8. Triple Combination Cream (TCC)
The most effective first-line therapies, according to recent papers, include sunscreen use, sun avoidance, and triple combination therapy. One of the first combination medicines used to treat hyperpigmentation was the Kligman-Willis formula. It has 5% HQ, 0.1% RA, and 0.1% dexamethasone in it. The formula has the potential to improve each drug's efficacy, reduce adverse effects, and shorten treatment time. Tretinoin can prevent HQ from oxidising, and the steroid component can minimise irritation from the other two components while also inhibiting the secretory function of melanocytes [25,33] .
8.1. Azelaic acid
Azelaic acid (AA) exerts a cytotoxic impact on hyperactive melanocytes that is selective. It has no effect on healthy skin since it primarily affects defective melanocytes. As a result, negative consequences are reduced [34] In a 6-month trial, 20% AA was found to be more effective than 2% HQ in comparison to HQ [35].
8.2. Kojic Acid (KA)
A randomised single-blind trial found that a combination of 1% KA and 2% HQ is more effective than 1% KA alone [36].
8.3. Arbutin/deoxyarbutin
The clinical benefit of lightening the leisions was noticed in 76 % of the treatment group in a double-blind, placebo-controlled, randomised study of 2.5% beta-arbutin applied twice daily in female patients with melasma for 8 weeks [37].
8.4. Ascorbic add (Vitamin C)
Ascorbic acid is highly unstable and oxidises quickly. When taken alone, it has a lower effectiveness. It is more effective when used in combination with licorice extracts [24,27].
8.5. Tranexamic acid
Tranexamic acid (TXA) inhibits plasmin synthesis that prevents the conversion of plasminogen to plasmin. UV irradiation can boost plasmin levels, which can activate melanin formation [38].
8.6. Chemical peeling
Second-line treatment is the addition of chemical peels to a topical treatment. Chemical peeling can improve epidermal remodelling and keratinocyte turnover, allowing lesions to be cleared more quickly and effectively [39,28].
8.7. Glycolic acid (GA)
More effective than GA peels alone were 20-50 % GA peels mixed with 2% HQ or 0.25 % tretinoin [40] Patients with resistant melasma who had a combination of peels with 20% AA and 0.1% adapalene gel at 3- week intervals for 6 months had a much better outcome when compared to those who only received 20% AA and 0.1% adapalene gel [41].
8.8. Lactic acid (LA)
Patients with epidermal melasma who have skin type IV may benefit from LA. All 12 individuals in one study who had 92 %LA peels every 3 weeks for 6 treatments had a statistically significant improvement in their MASI score [42].
8.9. Salicylic acid (SA)
SA is a keratolytic, anti-inflammatory beta hydroxy acid peel [1]. For superficial peeling in epidermal melasma, SA can be used at a concentration of 15-30% and administered once a week or twice a week [43].
8.10. Trichloroacetic acid (TCA) peels
TCA is an acetic acid derivative that is often used in the treatment of epidermal melasma at a dosage of 10-20% with good short-term results. Due to the significant risk of PIH and scarring, TCA should be used with caution in persons with darker skin types [1,24].
8.11. Jessner’s solution
Jessner's peel contains 14% resorcinol, 14% LA, and 14% SA. Through its keratolytic activity, it acts as a superficial chemical peeling agent [1]. When both peels were administered in conjunction with topical HQ and tretinoin [44]. Jessner's peel had equivalent efficacy to 70% GA.
8.12. Other chemical peels
Tretinoin peel ,amino fruit acid, and pyruvic peel are some of the other chemical peels used to treat melasma . Furthermore, using tretinoin 2 weeks before beginning the peels can reduce PIH and improve and maintain the peeling agents' effectiveness .
8.13. Future therapeutic modalities
Lasers may be used to treat melasma in the future, not only by directly targeting the pigment, but also by using Laser-Assisted Drug Delivery (LADD) which will be able to maximize the utilization of topical medications [27].In melasma patients, a recent split-face study analyzed the efficacy and safety of fractional Er:YAG laser as a drug delivery system for HQ: the side treated with Er:YAG laser and HQ had significantly lower MASI scores and pigmentation levels than the side treated with HQ alone [45]. Furthermore, because normal topical delivery would have little efficacy in treating this type of melasma, LADD may be a preferable technique of delivering drugs in the dermal type [27]. Radiofrequency (RF) devices have become increasingly popular in recent years. Because the mechanism of RF technology is not dependent on pigment, it can be used on patients of all skin types [46]. Further research into the efficacy of fractional RF in the treatment of melasma is needed. It is necessary to observe how the device can contribute in the treatment of melasma.
9. Melsma in Bangladeshi People
A study held in Dhaka CMH showed Duration of melasma ranged between 1 and 8 years with a mean 3.2±2.3 years. There was no significant precipitating factor observed in relation to occurrence of melasma. Most cases (84%) were of epidermal type and one-fourth (16%) of the cases were of mixed type of melasma. The most common pattern was malar (78%) followed by centrofacial pattern (24%) and mandibular (10%). MASI scores at baseline 6,12 and 18 weeks. Response to treatment in MASI scoring after 12 weeks was 78% reduction (from 26.5 to 5.9) in GA group and 79% reduction (from 28.9 to 6) in TCA group [47]. Another study showed, among the study participants (n=130), both groups Group A (n=65) and Group B (n=65) had the majority of female participants 44 (67.69%) and 43 (66.15%) respectively. In Group A patients, epidermal melasma was seen in 47(72.31%) followed by mixed type 11 (16.92%) and dermal 07 (10.77%). In Group B patients, the majority had epidermal melasma 40 (61.54%) followed by mixed type 18 (27.69%) and dermal 07 (10.77%). Distribution of melasma in Group A was frontal 07 (10.77%), centrofacial 51 (78.46%), chin 07 (10.77%) and in Group B, frontal 07 (10.77%), centrofacial 54 (83.07%), chin 04 (6.15%) respectively. In Group A patients, 36.90% of participants showed good and 45.40% showed excellent improvement and the satisfaction score was 11.08±2.91 at baseline vs 8.95±2.08 at week 8 and 7.84±2.44 at week 12. The improvement in Group A patients at 8th and 12th week was statistically significant p-value <0.05% but in Group B patients, findings at 8th week only were statistically significant [48].
Conclusions
Melasma is a common skin hyperpigmentation condition that affects largely Asian, African and Hispanic descent who mainly have dark skin especially skin type IV-VI. Although Melasma is caused by several factors like genetics, sunlight exposure, female sex hormones, thyroid problems, anticonvulsant medication and cosmetic items, the main pathogenesis is yet to be understood clearly. In the pathophysiology of melasma, paracrine factors from keratinocytes or fibroblasts, mast cells, microRNAs play a significant role. treatment of melasma is complicated due to it’s complex aetiology, chronicity and relapsing property. A combination of medication and modalities are frequently used as treatment rather than single therapy. The first-line treatment is currently topical agents among which triple combination is the most effective one. For moderate to severe melasma, TCC has greater improvement than 4% HQ monotherapy. Fluocinolone-based TCC can be used for more than 8 weeks up to 1 year in either daily, intermittent or tapering dose regimens. TCC can be given as a maintenance regimen twiceweekly up to 6 months in order to prevent relapse and achieve a long-term response. Besides, 3% topical TXA was found to be equally effective as 3% HQ mixed with 0.01% dexamethasone in the treatment of melasma.
Recommendation
Melasma's aetiology and pathophysiology aren't completely understood. As a result, more research is needed to pinpoint the actual cause. A greater understanding of the pathogenesis will aid in the development of innovative melasma treatments. Identification of melasma-specific triggering factors for particular patients may lead to a desirable personalised therapy in the future, overcoming the therapeutic challenges associated with melasma. There are a variety of treatments and unique therapeutic techniques to choose from. However, due to a lack of consistency in research characteristics and outcome evaluation, well-designed RCTs are lacking.
Acknowledgements
The wide range of disciplines involved in durability and versatility of Melasma (Chloasma): Pathogenesis and Treatment means that an Editors needs much assistance from referees in the evaluation of papers submitted for publication. I am very grateful to many colleagues for their thorough, helpful and usually prompt response to requests for their opinion and advice.
Declaration
Funding
None funding sources
Conflict of interest
None declared.
Ethical approval
The study was approved by the ethical committee of King’s College London, The United Kingdom.
References
- Ball Arefiev KL, Hantash BM. Advances in the treatment of melasma: a review of the recent literature. Dermatologic surgery 38 (2012): 971-984.
- Handel AC, Miot LD, Miot HA. Melasma: a clinical and epidemiological review. Anais brasileiros de dermatologia 89 (2014): 771-782.
- Dwari BC, Palaian S, Poudel A, et al. Clinical profile and management pattern of melasma patients in Western Nepal: A Hospital Based Study. Internet Journal of Dermatology 7 (2009).
- Kroumpouzos G, Cohen LM. Dermatoses of pregnancy. Journal of the American Academy of Dermatology 45 (2001): 1-22.
- Torok H, Taylor S, Baumann L, et al. A large 12-month extension study of an 8-week trial to evaluate the safety and efficacy of triple combination (TC) cream in melasma patients previously treated with TC cream or one of its dyads. Journal of drugs in dermatology: JDD 4 (2005): 592-597.
- Rathore S, Gupta S, Gupta V. Pattern and prevalence of physiological cutaneous changes in pregnancy: A study of 2000 antenatal women. Indian Journal of Dermatology, Venereology and Leprology 77 (2011): 402.
- Sehgal VN, Verma P, Srivastava G, et al. Melasma: treatment strategy. Journal of Cosmetic and Laser Therapy 13 (2011): 265-279.
- Kumar S, Mahajan BB, Kamra N. Melasma in North Indians: A clinical, epidemiological, and etiological study. Pigment International 1 (2014): 95.
- Madke B, Kar S, Yadav N, et al. Extrafacial melasma over forearms. Indian Dermatology Online Journal 7 (2016): 344.
- Gupta AK, Gover MD, Nouri K, et al. The treatment of melasma: a review of clinical trials. Journal of the American Academy of Dermatology 55 (2006): 1048-1065.
- Goh CL, Dlova CN. A retrospective study on the clinical presentation and treatment outcome of melasma in a tertiary dermatological referral centre in Singapore. Singapore medical journal 40 (1999): 455-458.
- Resnik SS. Melasma and other skin manifestations or oral contraceptives. Transactions of the New England Obstetrical and Gynecological Society 21 (1967): 101-107.
- Tamega AD, Miot LD, Bonfietti C, et al. Clinical patterns and epidemiological characteristics of facial melasma in Brazilian women. Journal of the European Academy of Dermatology and Venereology 27 (2013): 151-156.
- Duteil L, Cardot-Leccia N, Queille-Roussel C, et al. Differences in visible light-induced pigmentation according to wavelengths: a clinical and histological study in comparison with UVB exposure. Pigment cell & melanoma research 27 (2014): 822-826.
- Regazzetti C, Sormani L, Debayle D, et al. Melanocytes sense blue light and regulate pigmentation through opsin-3. Journal of Investigative Dermatology 138 (2018): 171-178.
- Hernández-Barrera R, Torres-Alvarez B, Castanedo-Cazares JP, et al. Solar elastosis and presence of mast cells as key features in the pathogenesis of melasma. Clinical and Experimental Dermatology: Continuing professional development (CPD) 33 (2008): 305-308.
- Lee AY. Recent progress in melasma pathogenesis. Pigment cell & melanoma research 28 (2015): 648-660.
- Kwon SH, Hwang YJ, Lee SK, et al. Heterogeneous pathology of melasma and its clinical implications. International Journal of Molecular Sciences 17 (2016): 824.
- Pandya AG, Hynan LS, Bhore R, et al. Reliability assessment and validation of the Melasma Area and Severity Index (MASI) and a new modified MASI scoring method. Journal of the American Academy of Dermatology 64 (2011): 78-83.
- Ball Arefiev KL, Hantash BM. Advances in the treatment of melasma: a review of the recent literature. Dermatologic surgery 38 (2012): 971-984.
- Lieu TJ, Pandya AG. Melasma quality of life measures. Dermatologic clinics 30 (2012): 269-280.
- Cestari TF, Hexsel D, Viegas ML, et al. Validation of a melasma quality of life questionnaire for Brazilian Portuguese language: the MelasQoL-BP study and improvement of QoL of melasma patients after triple combination therapy. British Journal of Dermatology 156 (2006): 13-20.
- Kim NH, Cheong KA, Lee TR, et al. PDZK1 upregulation in estrogen-related hyperpigmentation in melasma. Journal of investigative dermatology 132 (2012): 2622-2631.
- Rodrigues M, Pandya AG. Melasma: clinical diagnosis and management options. Australasian Journal of Dermatology 56 (2015): 151-163.
- Sarkar R, Gokhale N, Godse K, et al. Medical management of melasma: A review with consensus recommendations by Indian pigmentary expert group. Indian journal of dermatology 62 (2017): 558.
- Holme SA, Beattie PE, Fleming CJ. Cosmetic camouflage advice improves quality of life. British Journal of Dermatology 147 (2002): 946-949.
- Sheth VM, Pandya AG. Melasma: a comprehensive update: part II. Journal of the American Academy of Dermatology 65 (2011): 699-714.
- Ogbechie-Godec OA, Elbuluk N. Melasma: an up-to-date comprehensive review. Dermatology and therapy 7 (2017): 305-318.
- Jimbow K, Obata H, Pathak MA, et al. Mechanism of depigmentation by hydroquinone. Journal of Investigative Dermatology 62 (1974): 436-449.
- Espinal-Perez LE, Moncada B, Castanedo-Cazares JP. A double-blind randomized trial of 5% ascorbic acid vs. 4% hydroquinone in melasma. International journal of dermatology 43 (2004): 604-607.
- Haddad AL, Matos LF, Brunstein F, et al. A clinical, prospective, randomized, double-blind trial comparing skin whitening complex with hydroquinone vs. placebo in the treatment of melasma. International journal of dermatology 42 (2003): 153-156.
- Rendon M, Berneburg M, Arellano I, et al. Treatment of melasma. Journal of the American Academy of Dermatology 54 (2006): S272-281.
- Shankar K, Godse K, Aurangabadkar S, et al. Evidence-based treatment for melasma: expert opinion and a review. Dermatology and therapy 4 (2014): 165-186.
- Doris Hexsel MD, BSca CS. Objective assessment of erythema and pigmentation of melasma lesions and surrounding areas in long-term management regimens with triple combination. J Drugs Dermatol 13 (2014): 444-448.
- Garcia-Lopez M. Double-blind comparison of azelaic acid and hydroquinone in the treatment of melasma. Acta Derm Venereol (Stockh) 143 (1989): 58-61.
- Deo KS, Dash KN, Sharma YK, et al. Kojic acid vis-a-vis its combinations with hydroquinone and betamethasone valerate in melasma: a randomized, single blind, comparative study of efficacy and safety. Indian journal of dermatology 58 (2013): 281.
- Morag M, Nawrot J, Siatkowski I, et al. A double-blind, placebo-controlled randomized trial of Serratulae quinquefoliae folium, a new source of β-arbutin, in selected skin hyperpigmentations. Journal of Cosmetic Dermatology 14 (2015): 185-190.
- Taraz M, Niknam S, Ehsani AH. Tranexamic acid in treatment of melasma: A comprehensive review of clinical studies. Dermatologic therapy 30 (2017): e12465.
- Trivedi MK, Yang FC, Cho BK. A review of laser and light therapy in melasma. International journal of women's dermatology 3 (2017): 11-20.
- Garg VK, Sarkar R, Agarwal R. Comparative evaluation of beneficiary effects of priming agents (2% hydroquinone and 0.025% retinoic acid) in the treatment of melasma with glycolic acid peels. Dermatologic surgery 34 (2008): 1032-1040.
- Erbil H, Sezer E, Tastan B, et al. Efficacy and safety of serial glycolic acid peels and a topical regimen in the treatment of recalcitrant melasma. The Journal of dermatology 34 (2007): 25-30.
- Sharquie KE, Al-Tikreety MM, Al-Mashhadani SA. Lactic acid as a new therapeutic peeling agent in melasma. Dermatologic surgery 31 (2005): 149-154.
- Amer Ejaz NR, Iftikhar N, Muzzafar F. Comparison of 30% salicylic acid with Jessner’s solution for superficial chemical peeling in epidermal melasma. Journal of the College of Physicians and Surgeons Pakistan 18 (2008): 205-208.
- Lawrence N, Cox SE, Brody HJ. Treatment of melasma with Jessner's solution versus glycolic acid: a comparison of clinical efficacy and evaluation of the predictive ability of Wood's light examination. Journal of the American Academy of Dermatology 36 (1997): 589-593.
- Badawi AM, Osman MA. Fractional erbium-doped yttrium aluminum garnet laser-assisted drug delivery of hydroquinone in the treatment of melasma. Clinical, cosmetic and investigational dermatology 11 (2018): 13.
- El-Domyati M, Hosam W, Abdel-Azim E, et al. Microdermabrasion: a clinical, histometric, and histopathologic study. Journal of cosmetic dermatology 15 (2016): 503-513.
- Begum ST, Khan MA, Hasan MS, et al. A Comparative Study on Efficacy of 30% Trichloroacetic Acid versus 35% Glycolic Acid Peel in the Treatment of Melasma. Journal of Armed Forces Medical College, Bangladesh 12 (2016): 68-71.
- Karim AR, Sadeque SP, Ferdous A, et al. Treatment of Melasma Cases by Oral Tranexamic Acid: A Randomized Control Trial. Journal of Armed Forces Medical College, Bangladesh 14 (2018): 148-151.


 Impact Factor: * 5.3
Impact Factor: * 5.3 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 