Molecular Genetic Analysis of Maternal Inherited Diabetes with Deafness Associated Point Mutation A3243g in Puducherry
Article Information
R.R.Kumar1, AmirthaVarshini.M.J2, Biswajit Mohanty1
1Department of Biochemistry1, AarupadaiVeedu Medical College and Hospital, Vinayaka Missions Research Foundation, Pondicherry - 607403
2Department of Audiology and Speech Language Pathology2 AarupadaiVeedu Medical College and Hospital, Vinayaka Missions Research Foundation, Pondicherry - 607402
*Corresponding autor: R.R.Kumar, Department of Biochemistry1, AarupadaiVeedu Medical College and Hospital, Vinayaka Missions Research Foundation, Pondicherry - 607403;
Received: 25th Feb-2019; Revised: 25th Mar-2019; Accepted: 26th Mar-2019;
Copyright: ©2019 R.R.Kumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Citation: R.R.Kumar, AmirthaVarshini.M.J, Biswajit Mohanty. Molecular Genetic Analysis of Maternal Inherited Diabetes with Deafness Associated Point Mutation A3243g in Puducherry. International Journal of Plant, Animal and Environmental Sciences 9 (2019): 13-18.
View / Download Pdf Share at FacebookAbstract
The A3243G mutation of mitochondrial DNA (mtDNA) is main contributing factor for many common diseases, including diabetes mellitus and mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes (MELAS). In this study we aimed to understand the association between A3243G mutations with maternal inherited diabetes with deafness using Allele specific tetra ARMS PCR technique. In this study, we collected the blood samples from normal human and medically diagnosed diabetic subjects with maternal history.Allele-specific Tetra ARMS PCR for the A3243G mutation was performed in the presence of two sets newly designed primers.A successful PCR product with a single 475bp from wild condition was obtained and two bands at 475bp and 275bp were observed from mutant condition. To validate the results, we also conducted DNA sequencing for both the samples. The sequenced data is compared using bioinformatics tools and it is 100% matched with PCR results. We suggest that ARMS PCR method will be considered to be suitable candidate to diagnose the mutation responsible for maternally inherited diabetes with deafness.
Keywords
ARMS – PCR, Maternal Inherited diabetes, Mitochondrial DNA, DNA sequencing, m.3243A>G
Article Details
INTRODUCTION
Diabetes is considered to be one of the metabolic disorders in terms of incidence, healthcare costs and overall complications in developing and developed countries [1] .Diabetes is a major cause of blindness, kidney failure, heart attacks, stroke and lower limb amputation due to the inappropriate secretion of insulin leading to chronic hyperglycaemia. As a consequence of hyperglycaemia of diabetes, every tissue and organ of the body undergoes genetic and non-genetic alterations which account for the major complications in diabetics.
At present, several disorders such as Neurodegenerative and metabolic disorders are associated with mitochondrial gene mutation have been identified. According to the recently accepted criteria, diabetes with mitochondrial DNA mutations that result in impaired β cell function in islets of Langerhans has been classified as a distinct type of diabetes with familial clustering [2]. Therefore Diabetes with maternally inheritance pattern namely A3243G heteroplasmic mutation encoding tRNALeu (UUR) gene is thought to be responsible for the disease phenotype. It was found to be a major cause of maternally inherited diabetes accompanied with sensory neural hearing defect – a new subtype of diabetes mellitus which was given the name of “Maternally Inherited Diabetes and Deafness (MIDD)”. A3243G point mutation in the tRNALeu(UUR) gene is considered to be strongly linked with the pathogenesis of MIDD [3].
A variety of studies on diabetes mellitus shows, the A/G exchange is present in 0.5–1.5% of patients. If only those patients with a family history of diabetes are considered, the prevalence of the mutation is two to five times higher. In a cross sectional study in Netherlands among diabetes patients the prevalence of MIDD was reported to be 1.3% [4].
he prevalence of the mitochondrial mutation in a Japanese study was 4.6% in diabetic patients with maternal inheritance and/or hearing loss [5]. Similar finding were reported in a Chinese study [6]. In a cohort study conducted by Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow the incidence was found to be 1% (sample size 96). Therefore in the present study we aimed to evaluate whether the mitochondrial mutation (A-to-G) at position 3243 is significantwith patients suffering fromMIDD using Amplification Refractory mutation system (ARMS) primer.
MATERIALS AND METHODS
Prior to the start of the study, approval was obtained from the Institutional Ethical committee of AarupadaiVeedu medical college and hospital, Puducherry 607 403, India and written informedconsent was obtained from all the 30 patients (16 female and 14 male).
Audiometry and general examination
Puretone thresholds were measured using GSI 68 diagnostic audiometer in a sound treated room.Modified Hughson
– Westlake method was used to obtain the thresholds at 250 Hz, 500 Hz, 1KHz, 2 KHz , 4 KHz, 6 KHz and 8 KHz for Air conduction and 500 Hz, 1 KHz, 2 KHz and 4KHz for Bone conduction. Pure tone average was obtained at 500 Hz, 1 KHz and 2 KHz.Hearing impairment was categorized as minimal (16 – 25 dB), mild (26 – 40 dB), moderate (41– 55 dB), moderately severe ( 56 – 70 dB), severe (71 – 90 dB) and profound (91 dB and above).
Samples collection
All patients underwent a standardized clinical and laboratory evaluation. Next, samples were collected from the 30 suspected diabetic members. We collected 1.5–2.0 mL of blood samples from each participant to isolate adequate amount of DNA and stored at -80oC for further investigations
DNA extraction, amplification and sequencing
Genomic DNA was isolated and purified from blood samples following 0.2ml of blood is transferred to 1.5ml tube, 0.4ml of Lysis buffer is added and mixed well. 20ul of Proteinase K is added and incubated at -80oC for 10min. 200ul of Isopropanol is added and mixed well. Entire samples are transferred to HELINI Pure Fast Spin column and centrifuged at 12000rpm for 1min. Flow through is discarded and 0.5ml Wash buffer is added, centrifuged at 12000rpm for 1min. Flow through is discarded and 0.5ml Wash buffer-II is added. Centrifuged at 12000rpm for 1min. Flow through is discarded and empty spin is done for 2min. DNA is eluted by adding 50µl of elution buffer after centrifugation. The quality and quantity of eluted DNA is checked in 1% Agarose gel electrophoresis. [1gm agarose in 100ml of TAE buffer].
SNP Flanking region nucleotides are downloaded from NCBI. For downloaded nucleotide sequence, Tetra ARMS PCR primers are designed as follows; Forward inner primer (A allele, 275bp): 5’-
AGAACAGGGTTTGTTAAGATGGCCGA-3’,Reverseinnerprimer(Gallele,275bp):5’-
AAGTTTTAAGTTTTATGCGATTACCGGTCC-3’,Forwardouterprimer(5'-3',475bp):5’-
TGAGTTCAGACCGGAGTAATCCAGGT-3’, Reverse outer primer (5' - 3 475bp'): 5’-CGGTGATGTAGAGGGTGATGGTAGATG-3’. To screen for A3243G point mutation in the tRNALeu(UUR) gene,
PCR were conducted using the above primers for the patients suffering from Maternally Inherited Diabetes with or without Deafness.
All the PCR products are mixed with gel loading dye and loaded in vertical gel electrophoresis. Gel run at 100V to three fourth of its distance and Bands are visualized in UV Transilluminator for screening of MIDD.For further confirmation of the above results, we also sent the samples to Heleini Biomolecules, India for DNA sequencing. The sequenced data is compared using bioinformatics tools for identification of A3243G mutation gene.
RESULTS AND DISCUSSION
Clinical samples:
Thirty patients of maternal inherited Type 2 diabetes mellitus with or without hearing loss (Group 1) were thoroughly investigated and underwent a standard 75g oral glucose tolerance test (OGTT) to confirm diagnosis of T2DM. Mean age at which the patients developed diabetes mellitus was found to be 41 years. Mean plasma glucose and glycosylated hemoglobin level in patients of maternally inherited type 2 diabetes mellitus was significantly higher.Further these patients were subjected to audiography investigation to detect sensory neuronal deafness. In this study, bilateral neuro sensory hearing loss was present in 19 out of 30 maternally inherited diabetic patients (63.33%). Only four patients required a prosthetic hearing aid with the mean age of deafness was found to be 48 years. Diabetes was the first clinical manifestation of the disease in all of the patients, not the hearing loss [7]. Eleven patients did not present with any complaint of deafness (Table 1).
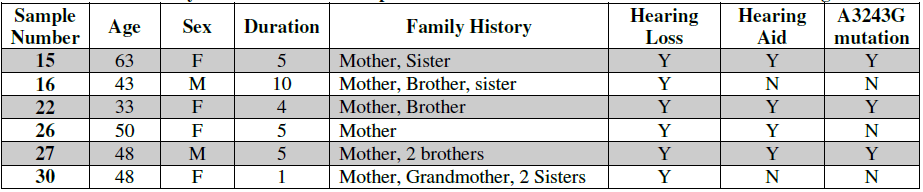
Table.1 Auditory characterization of 6 patients with maternal inherited diabetes with hearing loss
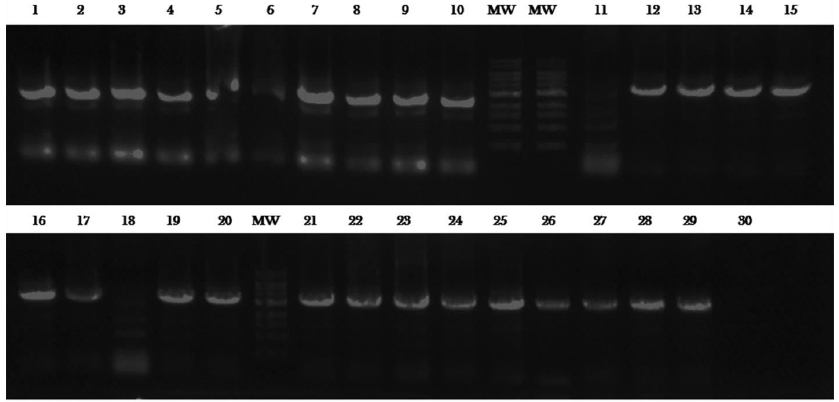
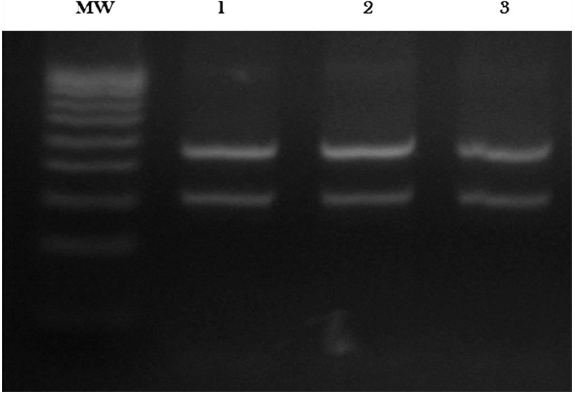
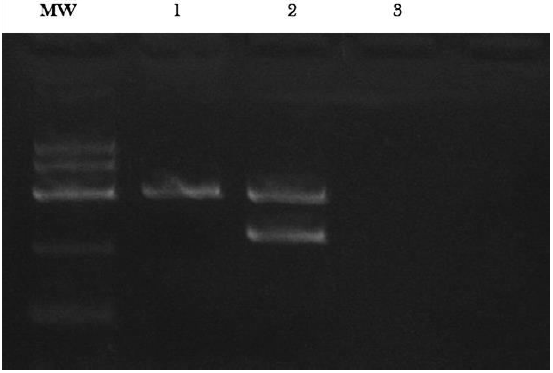
In wild type, at 3243 rd position will be having “A” in 5’ position. Complimentary for this is “T” will be opposite strand. We have designed a primer which ends with “A”. While PCR, if our primer “A” finds its complementary “T” at 3243 position, it will binds and extends, give rise to 475bp PCR product (Fig.1). If fails to find its complementary “T” at 3243 rd position, it will not bind that leads to absence of PCR product.In Mutant gene condition, at 3243 rd position will be having “G” in 5’ position.Complimentary for this“C” will be in opposite strand. We have designed a primer which ends with “C”. While PCR, if our primer “C” finds its complementary “G” at3243 position, it will binds and extends, give rise to 275 bp PCR product (Fig.2 & 3). If fails tofind its complementary “G” at 3243 rd position, it will not bind that leads to absence of the PCR product.As we understood that this particular mutation is heteroplasmy, in mutation condition, that is why we observe two bands. [ie.. normal mitochondria along with mutant] where as in pure wild, only one PCR product will be observed.
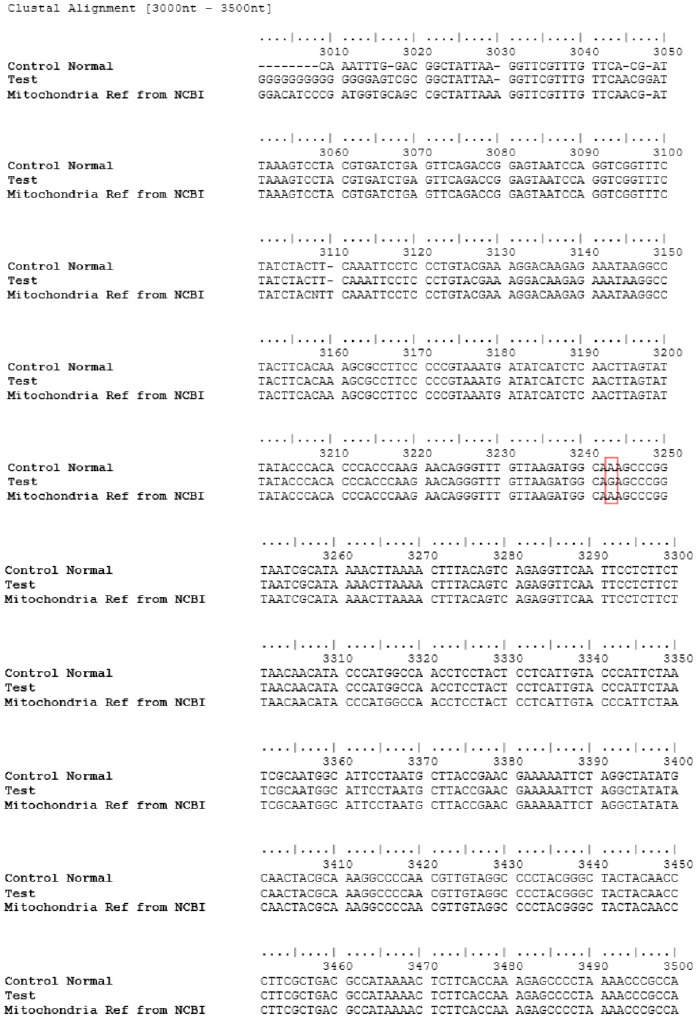
In our study we identified 10% of mtDNAA3243G mutation in tRNALeu(UUR) gene in maternal inherited diabetic patients whereas in control group no mutation was observed. Hence, our results also confirms and strengthen the findings of earlier studies. However, it really helps us to reach a conclusion that possible interaction of genetic factors has been involved in the development of T2DM and this study helped us to identify the diabetogenic gene mutation in suspected patients. However, almost all of the diseases produced by mutations in the mtDNA are usually accompanied by impaired hearing, mostly sensorineural in nature [8]. To validate results, we send both samples for DNA sequencing. The sequenced data is compared using bioinformatics tools and it is 100% matched
with PCR results. A multiple sequence alignment of wild type and mutant variant of mtDNAA3243G mutation in tRNALeu(UUR) gene in maternal inherited diabetic patients after obtaining from DNA sequencing report (Fig. 4). We suggest that this PCR method will be best one to use with diagnosis in order to identify the mutation responsible maternally inherited diabetes with deafness.
In conclusion, although previous clinical observations and studies have suggested some role of mitochondrial dysfunctions in the progression of type 2 diabetes mellitus, this study also confirms the A3243G mutation in mitochondrial tRNALeu(UUR) gene plays an important contributing etiological factor of T2DM in Puducherry population. The observed clinical hallmarks of diabetes might be the outcome of a one of the mechanism or factor involved in the pathogenesis of T2DM. Further screening of larger study group is required to fully determine the exact prevalence of this mutation in Puducherry population.
REFERENCES
- King, K.D., Jones, J.D. and Warthen, J., 2005. Microvascular and macrovascular complications of diabetes mellitus. American journal of pharmaceutical education, 69(5), p.87.
- Owen, K.R., Stride, A., Ellard, S. and Hattersley, A.T., 2003. Etiological investigation of diabetes in young adults presenting with apparent type 2 diabetes. Diabetes Care, 26(7), pp.2088-2093.
- Gerbitz, K.D., van den Ouweland, J.M., Maassen, J.A. and Jaksch, M., 1995. Mitochondrial diabetes mellitus: a review. Biochimicaet BiophysicaActa (BBA)-Molecular Basis of Disease, 1271(1), pp.253-260.
- Maassen, J.A. and Kadowaki, T., 1996. Maternally inherited diabetes and deafness: a new diabetes subtype. Diabetologia, 39(4), pp.375-382.
- Fukui, M., Nakano, K., Obayashi, H., Kitagawa, Y., Nakamura, N., Mori, H., Kajiyama, S., Wada, S., Fujii, M., Yoshimori, K. and Kanaitsuka, T., 1997. High prevalence of mitochondrial diabetes mellitus in Japanese patients with major risk factors. Metabolism, 46(7), pp.793-795.
- Li, M.Z., Yu, D.M., Pei, Y.U., Liu, D.M., Kun, W.A.N.G. and Tang, X.Z., 2008. Mitochondrial gene mutations and type 2 diabetes in Chinese families. Chinese medical journal, 121(8), pp.682-686.
- Naing, A., Kenchaiah, M., Krishnan, B., Mir, F., Charnley, A., Egan, C. and Bano, G., 2014. Maternally inherited diabetes and deafness (MIDD): Diagnosis and management. Journal of Diabetes and its Complications, 28(4), pp.542-546. (26)
- Van den Ouweland, J.M.W., Lemkes, H.H.P.J., Gerbitz, K.D. and Maassen, J.A., 1995. Maternally inherited diabetes and deafness (MIDD): a distinct subtype of diabetes associated with a mitochondrial tRNALeu (UUR) gene point mutation. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine, 18(S14), pp.S124-S130. (20)

 Impact Factor: * 3.6
Impact Factor: * 3.6 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 