Mystery of The Blue Toes
Article Information
Alena Varantsova*
NYP Brooklyn Methodist hospital, New York, USA
*Corresponding Author: Dr. Alena Varantsova, NYP Brooklyn Methodist hospital, New York, USA
Received: 15 March 2021; Accepted: 06 April 2021; Published: 03 May 2021
Citation: Alena Varantsova. Mystery of The Blue Toes. Archives of Clinical and Medical Case Reports 5 (2021): 361-367.
View / Download Pdf Share at FacebookKeywords
Hemolytic anemia; Pulmonary; Hematocrit
Hemolytic anemia articles; Pulmonary articles; Hematocrit articles
Hemolytic anemia articles Hemolytic anemia Research articles Hemolytic anemia review articles Hemolytic anemia PubMed articles Hemolytic anemia PubMed Central articles Hemolytic anemia 2023 articles Hemolytic anemia 2024 articles Hemolytic anemia Scopus articles Hemolytic anemia impact factor journals Hemolytic anemia Scopus journals Hemolytic anemia PubMed journals Hemolytic anemia medical journals Hemolytic anemia free journals Hemolytic anemia best journals Hemolytic anemia top journals Hemolytic anemia free medical journals Hemolytic anemia famous journals Hemolytic anemia Google Scholar indexed journals Pulmonary articles Pulmonary Research articles Pulmonary review articles Pulmonary PubMed articles Pulmonary PubMed Central articles Pulmonary 2023 articles Pulmonary 2024 articles Pulmonary Scopus articles Pulmonary impact factor journals Pulmonary Scopus journals Pulmonary PubMed journals Pulmonary medical journals Pulmonary free journals Pulmonary best journals Pulmonary top journals Pulmonary free medical journals Pulmonary famous journals Pulmonary Google Scholar indexed journals anemia articles anemia Research articles anemia review articles anemia PubMed articles anemia PubMed Central articles anemia 2023 articles anemia 2024 articles anemia Scopus articles anemia impact factor journals anemia Scopus journals anemia PubMed journals anemia medical journals anemia free journals anemia best journals anemia top journals anemia free medical journals anemia famous journals anemia Google Scholar indexed journals environment articles environment Research articles environment review articles environment PubMed articles environment PubMed Central articles environment 2023 articles environment 2024 articles environment Scopus articles environment impact factor journals environment Scopus journals environment PubMed journals environment medical journals environment free journals environment best journals environment top journals environment free medical journals environment famous journals environment Google Scholar indexed journals Hematocrit articles Hematocrit Research articles Hematocrit review articles Hematocrit PubMed articles Hematocrit PubMed Central articles Hematocrit 2023 articles Hematocrit 2024 articles Hematocrit Scopus articles Hematocrit impact factor journals Hematocrit Scopus journals Hematocrit PubMed journals Hematocrit medical journals Hematocrit free journals Hematocrit best journals Hematocrit top journals Hematocrit free medical journals Hematocrit famous journals Hematocrit Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Chronic cold agglutinin disease articles Chronic cold agglutinin disease Research articles Chronic cold agglutinin disease review articles Chronic cold agglutinin disease PubMed articles Chronic cold agglutinin disease PubMed Central articles Chronic cold agglutinin disease 2023 articles Chronic cold agglutinin disease 2024 articles Chronic cold agglutinin disease Scopus articles Chronic cold agglutinin disease impact factor journals Chronic cold agglutinin disease Scopus journals Chronic cold agglutinin disease PubMed journals Chronic cold agglutinin disease medical journals Chronic cold agglutinin disease free journals Chronic cold agglutinin disease best journals Chronic cold agglutinin disease top journals Chronic cold agglutinin disease free medical journals Chronic cold agglutinin disease famous journals Chronic cold agglutinin disease Google Scholar indexed journals Cancer articles Cancer Research articles Cancer review articles Cancer PubMed articles Cancer PubMed Central articles Cancer 2023 articles Cancer 2024 articles Cancer Scopus articles Cancer impact factor journals Cancer Scopus journals Cancer PubMed journals Cancer medical journals Cancer free journals Cancer best journals Cancer top journals Cancer free medical journals Cancer famous journals Cancer Google Scholar indexed journals Microscopic colitis articles Microscopic colitis Research articles Microscopic colitis review articles Microscopic colitis PubMed articles Microscopic colitis PubMed Central articles Microscopic colitis 2023 articles Microscopic colitis 2024 articles Microscopic colitis Scopus articles Microscopic colitis impact factor journals Microscopic colitis Scopus journals Microscopic colitis PubMed journals Microscopic colitis medical journals Microscopic colitis free journals Microscopic colitis best journals Microscopic colitis top journals Microscopic colitis free medical journals Microscopic colitis famous journals Microscopic colitis Google Scholar indexed journals
Article Details
1. Introduction
Chronic cold agglutinin disease (CAD) is a subgroup of autoimmune hemolytic anemia. The autoantibodies responsible for hemagglutination at low temperature, cold agglutinins, bind to erythrocytes and cause agglutination, which causes activation of complement and cold-induced circulatory symptoms. Essential clinical manifestation of primary CAD is hemolytic anemia and cold-induced circulatory symptoms [1]. CAD is rare to present as peripheral gangrene, and there are only a few published reports in the medical literature. We are reporting a case of peripheral gangrene, which was due to CAD.
2. Case Presentation
An 81-year-old non-verbal female was sent from a nursing home with new-onset bilateral toe cyanosis. Her past medical history included coronary artery disease, pulmonary embolism status post inferior vena cava filter placement, chronic ischemic cardiomyopathy, hypertension, hyperlipidemia, hypothyroidism, anemia, cerebral vascular accident with left arm hemiparesis, schizophrenia, chronic respiratory failure on supplemental oxygen and dementia.
Her admission vitals showed a temperature of 98o F, blood pressure 109/62, pulse 105 BPM, and oxygen saturation of 91% on a nonrebreather mask. The review of systems was unobtainable due to the patient's clinical status. Physical exam revealed cyanotic changes in both feet where toes were cold to touch with sharp demarcation at the metacarpophalangeal joint, although both dorsal pedis and tibial pulses were 2+ bilaterally. Refer to Figure 1 and 2. Initial laboratory findings included hemoglobin 10.1 g/dL, hematocrit 13.0 %, mean corpuscular volume (MCV) of 123 fL/cell.
There was high suspicion for lower limb ischemia from peripheral artery disease (PAD). However, ankle-brachial index/pulse volume recording, computed tomography angiography of the lower extremities, and venous doppler ultrasound were negative, ruling out peripheral vascular disease and deep vein thrombosis. A computed tomography scan of the chest suggested chronic pulmonary embolism. A transthoracic echocardiogram showed severe pulmonary hypertension. EKG showed short RP interval and prolonged QTc.
Early in her admission, the laboratory discovered that her blood samples would agglutinate, producing lab results that were hemolyzed. Also, there was a mismatch between hematocrit and hemoglobin ratio, showing significantly lower than expected hematocrit level. From these observations, there was a high suspicion of CAD. Additional workup showed reticulocyte count of 3.7%, peripheral blood smear showing red blood cell (RBC) agglutination (refer to Figure 3), direct Coombs test positive for C3D and negative for IgG, total IgM level: 326 mg/dL. Mycoplasma IgG was positive; however, IgM was negative. The Hepatitis panel was negative. Serum protein electrophoresis showed a small monoclonal band in the gamma region, demonstrating IgM/Kappa identity. Urine protein electrophoresis showed no proteins. Diagnosis of CAD was made based on the above laboratory findings.
The patient was given a warmer and managed conservatively with avoidance of cold temperatures. Given the patients' multiple co-morbidities and poor functional status, it was elected to treat the patient with conservative medical management. Medical treatment included heparin drip and a trial of bilevel positive airway pressure. Cyanosis remained largely stable while on anti-coagulation. Hospital course complicated by worsening hypoxic respiratory failure. The health care proxy elected for comfort measures, and the patient ultimately expired.
An autopsy was performed showing coronary artery disease; the left anterior descending artery shows approximately 80% occlusion, right ventricle dilation to 1.8 cm, and remote myocardial infarction. Extremities report showed five black gangrenous toes. Section of the spleen showed significant congestion. Section of bone marrow showed cellular marrow for age and left shift. The cause of death was a saddle embolus of the right pulmonary artery.

Figure 1 and 2: Patient presenting with peripheral cyanosis.

Figure 3: Peripheral blood smear showing agglutination.
3. Discussion
CAD is a type of autoimmune hemolytic anemia that occurs due to infections, malignancy, autoimmune diseases and paraproteins. This triggers the formation of pathological antibodies (most commonly IgM) that are directed against RBC surface [2]. The hemolysis is due to IgM binding to RBC surfaces leading to agglutination in the presence of a drop in blood temperature, which in terms leads to activation of complements cascade resulting in intravascular cell lysis. When warming of the blood occurs, IgM detaches from the cell surface resulting in agglutinated cells detaching from each other [3]. Pathophysiology of CAD depicted in Figure 4 [4]. Pathologic cold agglutinins occur in titers above 1:1000 and frequently react at 28-31°C and rarely at 37°C [5]. These high titers cause sludging of the RBCs resulting in cold and painful extremities (also known as acrocyanosis).
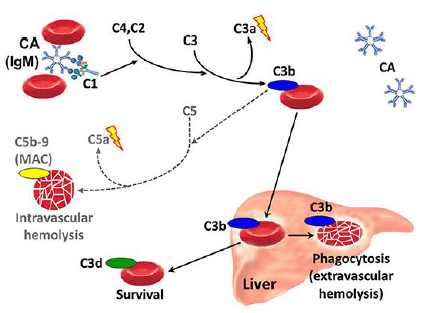
Figure 4: Pathophysiology of CAD.
CAD has traditionally been classified into a primary or idiopathic type which has been regarded unrelated to underlying condition and has been associated with clonal B-lymphocyte proliferation, and a secondary type associated with malignant disease, most often lymphoma [6] or underlying infections [3, 7]. Diagnosis can be guided based on physical symptoms. Patients can present with cyanosis or reporting pain or discomfort upon exposure to cold. Signs of respiratory distress may be present. Very few cases have been published regarding gangrene in these patients. Patel M et al. explains a case of syphilis with existing cold agglutinin disease that led to peripheral gangrene [7]. Bachmeyer C et al. describes a patient who had T cell lymphoma cold-induced immune hemolysis that led to gangrene [6].
To confirm the diagnosis, laboratory results are crucial. A hemoglobin-hematocrit mismatch can be an important diagnostic clue on initial evaluation. The micro-aggregation of erythrocytes is counted as single cells and large clamps of cells are excluded from the count, which leads to decreased RBC count, falsely low hematocrit level, and elevated MCV [8]. An elevated reticulocyte count in response to the patient's anemia is common. Cold agglutinin titers are present in normal individuals, usually less than 1:64, with patients with CAD having amounts exceeding 1:2000 [9].
Due to the constant consumption, this may lead to a drop in complement levels. Positive Coombs test shows bound complement on erythrocytes. Diagnostic criteria for primary CAD depicted in Table 1. After a diagnosis has been made, the patient should be worked up for infection, lymphoma, and autoimmune disorders. Further testing can include serum electrophoresis, measurement of serum immunoglobulins, and flow cytometry of the bone marrow aspirate.
|
Chronic hemolysis |
|
Cold agglutinin titers >= 64 @ 4°C |
|
COOMBS test polyspecific positive or specific for C3d |
|
Absence of secondary causes: malignancy or infections |
Table 1: Diagnostic criteria for Primary CAD.
Modality of treatment of CAD depends on severity and character of underlying symptoms, degree of anemia and presence of underlying disease. Non-pharmacological management includes avoidance of cold exposure or infusion of cold liquids. Transfusions can be safely given when indicated, provided the necessary precautions are observed. Patients are usually not responsive to splenectomy or corticosteroids, and such modalities should be avoided [10]. Plasmapheresis is efficient as a "first-aid" in an acute situation in patients presenting with severe symptoms or before surgery; however, remission achieved is only short-lived [10]. There are have been no large trials to access the efficacy of plasmapheresis, and currently known data is based on case reports only. IVIG has been rarely used in CAD, and its efficacy is not well characterized. The only case reports data is available [11].
There is evidence that CAD is a clonal lymphoproliferative disorder (LPD) of the bone marrow, producing cold agglutinins, detected in blood or marrow without clinical or radiological evidence of malignancy [2]. That is the reason why B-cell-directed therapy became the main pharmacological therapy in the management of chronic symptoms of CAD. Rituximab has been studied as a single agent [12, 13] as well as in combination with Bendamustine or Fludarabine. When used alone, an overall response rate was 54%, with the median response duration of 11-13 months. Overall, treatment was well tolerated [13]. The Fludarabine and Rituximab is a very efficient combination with a response rate of 76% and 21% of patients achieving complete response (CR).
A majority of the patients tolerated the treatment well. However, there were observed cases of asymptomatic cytopenias. Few patients experienced reactivation of Herpes Zoster [14]. Chemoimmunotherapy with Bendamustine and Rituximab results in a high total response rate (71-78%), and the CR rate was nearly doubled compared with the fludarabine-rituximab trial (41% vs 21%), with response rate lasting for more than 88 months. The safety profile appears more favorable using bendamustine-rituximab than with the fludarabine-rituximab combination and may be considered as a first-line treatment for most patients with CAD requiring therapy [12, 15]. Bortezomib is an acceptable non-rituximab-based therapy for patients not able to tolerate alternatives [16]. The summary of pharmacological management of CAD is depicted in Table 2.
|
Medications regimen |
Response rate |
Duration of response |
Side effects |
|
IvIg |
Unknown |
Unknown |
No reports |
|
Plasmapheresis |
Unknown |
Unknown |
No reports |
|
Rituximab |
54% |
11-13 month |
Well tolerated |
|
Rituximab + Bendamustine |
71-78% (40-53% CR) |
>88 month |
Neutropenia GI symptoms |
|
Rituximab + Fludarabine |
76% (20% CR) |
> 66 months |
Neutropenia Herpes Zoster |
|
Bortezomib |
32% (16% CR) |
16 months |
Neurotoxicity, rare |
Table 2: Overview of pharmacological management of CAD.
4. Conclusion
CAD remains a rare cause of peripheral gangrene; however, it should be considered when the most common causes of dry gangrene are excluded on initial workup and in the presence of characteristic laboratory findings. In the presented case, given the patient's age and past medical history, there was a high suspicion of PAD. However, the observation that her blood samples would agglutinate at room temperature, resulting in hemoglobin-hematocrit mismatch and need to be re-warmed, led to a diagnosis of CAD. In the case of this patient, peripheral blood sample agglutination likely related to secondary CAD due to the presence of monoclonal bands.
References
- Berentsen S, Beiske K, Tjønnfjord GE. Primary chronic cold agglutinin disease: an update on pathogenesis, clinical features and therapy. Hematology 12 (2007): 361-370.
- Silberstein LE, Berkman EM, Schreiber AD. Cold hemagglutinin disease associated with IgG cold-reactive antibody. Ann Intern Med 106 (1987): 238-242.
- Karunarathne S, Weerasinghe S, Govindapala D, et al. Cold autoimmune haemolytic anaemia secondary to Epstein Barr virus infection presenting with peripheral gangrene; case report. Thromb J 10 (2012): 4.
- Berentsen S. New Insights in the Pathogenesis and Therapy of Cold Agglutinin-Mediated Autoimmune Hemolytic Anemia. Front Immunol 11 (2020): 590.
- Swiecicki PL, Hegerova LT, Gertz MA. Cold agglutinin disease. Blood 122 (2013): 1114-1121.
- Bachmeyer C, Blum L, Chesneau AM, et al. Raynaud's phenomenon with necrosis of the extremities induced by cold agglutinin disease secondary to a T-cell lymphoma. Acta Derm Venereol 83 (2003): 374-375.
- Patel M, Durao H, Govender Y. Paroxysmal cold haemoglobinuria coexisting with cold agglutinins in a patient with syphilis resulting in peripheral gangrene: a case report. East Afr Med J 70 (1993): 526-527.
- Ercan S, Cal1skan M, Koptur E. 70-year old female patient with mismatch between hematocrit and hemoglobin values: the effects of cold agglutinin on complete blood count. Biochem Med (Zagreb) 24 (2014): 391-395.
- Sinha A, Richardson G, Patel RT. Cold agglutinin related acrocyanosis and paroxysmal haemolysis. Eur J Vasc Endovasc Surg 30 (2005): 563-565.
- Berentsen S. How I manage patients with cold agglutinin disease. Br J Haematol 181 (2018): 320-330.
- Kanemitsu S, Onoda K, Yamamoto K, et al. Simple preoperative management for cold agglutinins before cardiac surgery. J Thorac Cardiovasc Surg 140 (2010): e73-e74.
- Berentsen S, Barcellini W, D'Sa S, et al. Cold agglutinin disease revisited: a multinational, observational study of 232 patients. Blood 136 (2020): 480-488.
- Berentsen S, Ulvestad E, Gjertsen BT, et al. Rituximab for primary chronic cold agglutinin disease: a prospective study of 37 courses of therapy in 27 patients. Blood 103 (2004): 2925-2928.
- Berentsen S, Randen U, Vågan AM, et al. High response rate and durable remissions following fludarabine and rituximab combination therapy for chronic cold agglutinin di3ease. Blood 116 (2010): 3180-3184.
- Berentsen S, Randen U, Oksman M, et al. Bendamustine plus rituximab for chronic cold agglutinin disease: results of a Nordic prospective multicenter trial. Blood 130 (2017): 537-541.
- Rossi G, Gramegna D, Paoloni F, et al. Short course of bortezomib in anemic patients with relapsed cold agglutinin disease: a phase 2 prospective GIMEMA study. Blood 132 (2018): 547-550.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
