Paradoxical Presentation In A Case of Deep Frontal Lobe Abscess
Article Information
Vasan TS, Karan Mathur*, Rahul Vyas
JSS Medical College and Hospital, Mysore, Karnataka, India
*Corresponding Author: Karan Mathur, JSS Medical College and Hospital, Mysore, Karnataka, India
Received: 11 November 2019; Accepted: 02 December 2019; Published: 13 January 2020
Citation: Vasan TS, Karan Mathur, Rahul Vyas. Paradoxical Presentation In A Case of Deep Frontal Lobe Abscess. Archives of Clinical and Medical Case Reports 4 (2020): 071-074.
View / Download Pdf Share at FacebookAbstract
A pyogenic brain abscess may start initially with cerebritis and later develop a capsule and a necrotic centre thus, forming an abscess. A pyogenic abscess is not uncommon and can be due to a multitude of organisms. It may occur due to spread from a contiguous focus, haematogenous spread or head trauma etc. We report here, a case with no detectable source of infection in a case with a left to right shunt patent foramen ovale (PFO). Such a shunt is an unusual presentation as only a right to left shunt is known to bypass the pulmonary filter and lead to seeding, in the absence of a coexisting pulmonary arteriovenous malformation.
Keywords
Brain abscess; Neurosurgery; Patent foramen ovale; Left to right shunt; Cryptogenic brain abscess
Brain abscess articles, Neurosurgery articles, Patent foramen ovale articles, Left to right shunt articles, Cryptogenic brain abscess articles
Brain abscess articles Brain abscess Research articles Brain abscess review articles Brain abscess PubMed articles Brain abscess PubMed Central articles Brain abscess 2023 articles Brain abscess 2024 articles Brain abscess Scopus articles Brain abscess impact factor journals Brain abscess Scopus journals Brain abscess PubMed journals Brain abscess medical journals Brain abscess free journals Brain abscess best journals Brain abscess top journals Brain abscess free medical journals Brain abscess famous journals Brain abscess Google Scholar indexed journals Neurosurgery articles Neurosurgery Research articles Neurosurgery review articles Neurosurgery PubMed articles Neurosurgery PubMed Central articles Neurosurgery 2023 articles Neurosurgery 2024 articles Neurosurgery Scopus articles Neurosurgery impact factor journals Neurosurgery Scopus journals Neurosurgery PubMed journals Neurosurgery medical journals Neurosurgery free journals Neurosurgery best journals Neurosurgery top journals Neurosurgery free medical journals Neurosurgery famous journals Neurosurgery Google Scholar indexed journals Patent foramen ovale articles Patent foramen ovale Research articles Patent foramen ovale review articles Patent foramen ovale PubMed articles Patent foramen ovale PubMed Central articles Patent foramen ovale 2023 articles Patent foramen ovale 2024 articles Patent foramen ovale Scopus articles Patent foramen ovale impact factor journals Patent foramen ovale Scopus journals Patent foramen ovale PubMed journals Patent foramen ovale medical journals Patent foramen ovale free journals Patent foramen ovale best journals Patent foramen ovale top journals Patent foramen ovale free medical journals Patent foramen ovale famous journals Patent foramen ovale Google Scholar indexed journals Laparoscopy articles Laparoscopy Research articles Laparoscopy review articles Laparoscopy PubMed articles Laparoscopy PubMed Central articles Laparoscopy 2023 articles Laparoscopy 2024 articles Laparoscopy Scopus articles Laparoscopy impact factor journals Laparoscopy Scopus journals Laparoscopy PubMed journals Laparoscopy medical journals Laparoscopy free journals Laparoscopy best journals Laparoscopy top journals Laparoscopy free medical journals Laparoscopy famous journals Laparoscopy Google Scholar indexed journals Left to right shunt articles Left to right shunt Research articles Left to right shunt review articles Left to right shunt PubMed articles Left to right shunt PubMed Central articles Left to right shunt 2023 articles Left to right shunt 2024 articles Left to right shunt Scopus articles Left to right shunt impact factor journals Left to right shunt Scopus journals Left to right shunt PubMed journals Left to right shunt medical journals Left to right shunt free journals Left to right shunt best journals Left to right shunt top journals Left to right shunt free medical journals Left to right shunt famous journals Left to right shunt Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals Cryptogenic brain abscess articles Cryptogenic brain abscess Research articles Cryptogenic brain abscess review articles Cryptogenic brain abscess PubMed articles Cryptogenic brain abscess PubMed Central articles Cryptogenic brain abscess 2023 articles Cryptogenic brain abscess 2024 articles Cryptogenic brain abscess Scopus articles Cryptogenic brain abscess impact factor journals Cryptogenic brain abscess Scopus journals Cryptogenic brain abscess PubMed journals Cryptogenic brain abscess medical journals Cryptogenic brain abscess free journals Cryptogenic brain abscess best journals Cryptogenic brain abscess top journals Cryptogenic brain abscess free medical journals Cryptogenic brain abscess famous journals Cryptogenic brain abscess Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals blood pressure articles blood pressure Research articles blood pressure review articles blood pressure PubMed articles blood pressure PubMed Central articles blood pressure 2023 articles blood pressure 2024 articles blood pressure Scopus articles blood pressure impact factor journals blood pressure Scopus journals blood pressure PubMed journals blood pressure medical journals blood pressure free journals blood pressure best journals blood pressure top journals blood pressure free medical journals blood pressure famous journals blood pressure Google Scholar indexed journals tumor articles tumor Research articles tumor review articles tumor PubMed articles tumor PubMed Central articles tumor 2023 articles tumor 2024 articles tumor Scopus articles tumor impact factor journals tumor Scopus journals tumor PubMed journals tumor medical journals tumor free journals tumor best journals tumor top journals tumor free medical journals tumor famous journals tumor Google Scholar indexed journals
Article Details
1. Introduction
A brain abscess is a relatively uncommon, yet life-threatening condition. They are frequently known to arise from a contiguous source of infection or via haematogenous spread. In such cases, which are potentially fatal it is of utmost importance to know the source of infection, but unfortunately 10 to 35 % of brain abscesses are cryptogenic[1]. In cases with cardiac anomalies which have right to left shunting of blood, the foci of infection can bypass the pulmonary filter and embolise in the cerebral microvasculature and cause a brain abscess; but in cases with only a left to right shunting of blood such a result is unreported without the presence of coexisting arteriovenous malformations. In this report, we present a case of a brain abscess that occurred in an apparently healthy young female patient presenting with complaints of jaundice and diarrhoea with an undetected PFO, who did not have any clinically apparent source of infection throughout her course in the hospital.
2. Case Report
A 20-year-old female presented to the emergency room with fever, chills, vomiting along with complaints of jaundice and watery stools for about a week. She admitted to consuming alternative medicine for the same. On arrival her O2 saturation was 88% on room air, Pulse was 98 beats/min and regular, Respiratory rate was 22 cycles/min, her temperature was 99.5? and blood pressure was 100/60 mm of Hg. On admission, she was fully conscious and aware of her surroundings with a Glasgow Coma Scale (GCS) of 15.
On examination, icterus, clubbing and cyanotic features were noted. She was admitted to the general medicine ward for further management. On the second-day post admission, she was found to be drowsy, disoriented, speaking only a couple of words on repeated questioning and was moving all limbs with no focal deficits. Computed Tomography (CT) and Contrast Enhanced Magnetic Resonance Imaging (MRI) (Figure 1) of the brain revealed a deep right frontal lobe brain abscess communicating with the frontal horn of lateral ventricle resulting in ventriculitis and choroiditis with adjacent subacute haemorrhage. There was no evidence of any foci of infection in contiguous locations. Magnetic Resonance Spectroscopy (MRS) revealed evidence of high lipid/lactate peak decreased choline and N-Acetyl Aspartate (NAA).
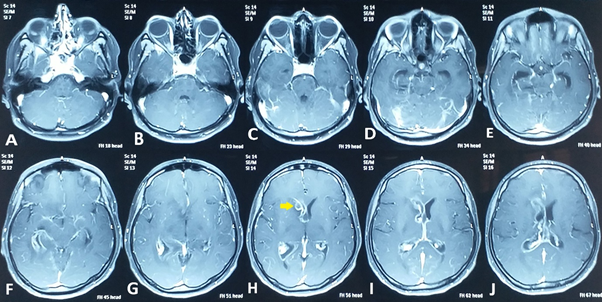
Figure 1: Axial cuts of the Contrast Enhanced MRI showing the abscess (marked with a yellow arrow) in panes H, I and J.
Serial blood and urine cultures did not show any growth. She was then referred to neurosurgery and managed in the Intensive Care Unit (ICU). On admission to the ICU, the patient’s relatives revealed a history of cyanotic spells since childhood.
Fundoscopy revealed no papilledema, suggesting normal intracranial pressure. The Otorhinolaryngologist was unable to find any potential sources of infection in the paranasal sinuses, oral cavity or ears. Cardiac evaluation with echo, revealed a tiny PFO with a left to right shunt, mild tricuspid regurgitation, dilated right atrium and ventricle. CT of the heart revealed cardiomegaly, a 3mm inferoseptal ventricular septal defect, dilated right heart, dilated inferior vena cava, superior vena cava and a thin left ventricle wall.
In the absence of any overt cardiac causative factors causing brain abscess, a pulmonary angiography was done to rule out pulmonary arteriovenous malformations. This revealed a normal pulmonary vasculature. Due to a small sized single abscess, the patient was managed conservatively with antibiotics; she was given meropenem-sulbactam along with metronidazole and linezolid. Antiepileptics were given in the form of oral levetiracetam along with mannitol to manage intracranial pressure and dexamethasone to control cerebral oedema.
The patient responded to treatment, regained consciousness and recovered from her fever. She was ambulatory and was moving all four limbs at the time of discharge, but was discharged early against medical advice due to financial constraints.
3. Discussion
Brain abscesses frequently occur due to the haematogenous spread of septic microemboli from other sources of infection in the body and can also occur by the spread of infection from a contiguous focus of infection [2]. The most common causes of brain abscesses include; spread from a contiguous focus 25 to 50% of the time (ear/mastoid (40-63.3%), sinuses (15%), oral cavity (15%), meninges etc.), hematogenous spread 20 to 35% of cases, and by direct traumatic and intraoperative inoculation [1, 6].
Multiple brain abscesses are usually the result of metastatic spread from remote primary foci and single abscesses commonly occur by extension from adjacent infected foci, according to independent studies by Le Moal et al and Bakshi et al. [3, 4]. This case presented with a single deep right frontal lobe abscess, which points towards the presence of a contiguous focus/foci. However, no such infective focus could be revealed on imaging.
Even though the neuroimaging is not suggestive of haematogenous spread, the patient could have developed the abscess from this route as she was found to have cardiac anomalies including a patent foramen ovale. Kastenbauer et al. suggest several such potential mechanisms of spread that include expansion of an adjacent focus, haematogenous spread from the venous circulation like in right to left shunting of blood or in pulmonary arteriovenous malformations (fistulae) and direct traumatic spread [5]. However, a large number of brain abscesses are designated cryptogenic and are attributed to low-level bacteraemia due to asymptomatic dental infections due to the lack of any other explainable focus of infection.
This case revealed no detectable right to left shunting on TEE and a normal pulmonary vasculature on pulmonary angiography, suggesting no overt cardiac cause of the spread of infection. Nonetheless, there remains the possibility of transient reversal of shunting at the PFO causing a right to left shunt and enabling venous blood to bypass the pulmonary filter. Treatment options in such cases can be conservative or surgical; conservative treatment alone is usually given if ICP is not raised, especially if the abscess is small (<3 cm) [6].
Recommended conservative treatment includes a third generation cephalosporin, metronidazole and vancomycin [6]. This patient also received similar treatment, she was administered meropenem-sulbactam, metronidazole and linezolid to provide similar antibacterial coverage. The mainstay of surgical treatment is stereotactic needle aspiration of the brain abscess in cases of a deep-seated abscess. In cases of a more superficial abscess, excision may be considered.
5. Conclusion
A brain abscess is known to occur via seeding from many different foci, but in this case, no known foci could be found and implicated even with the presence of a known risk factor like patent foramen ovale. A PFO with left to right shunt with normal pulmonary vasculature may also possibly be associated with brain abscess. According to our review of literature, many studies and reports suggest the definitive treatment of choice as repair of PFO rather than lifelong anticoagulant therapy, but in this case, the same cannot be recommended as there is no direct evidence of any right to left shunting along with relatively normal cardiac function, even though the patient presents with a history of hypoxia and cyanosis.
Conflicts of Interest
There are no conflicts of interest to declare.
References
- Allan RT, W Michael S: Brain Abscess. Youmans Neurological Surgery. H Richard W (6th edition) 1 (2011): 588-599.
- Seong Rok Han, Chan Young Choi, Jae-Jin Kwak. Prevotella brain abscess in a healthy young patient with patent foramen ovale. Clinical Neurology Neurosurgery 142 (2016): 128-131.
- Le Moal G, Landron C, Grollier G, et al. Characteristics of brain abscess with isolation of anaerobic bacteria. Scandinavian Journal of Infectious Diseases 35 (2003): 318-321.
- Rohit Bakshi, Peter D. Wright, Peter R. Kinkel, Vernice E. Bates, Laszlo L. Mechtler, Sadaat Kamran et al. Cranial magnetic resonance imaging findings in bacterial endocarditis: The neuroimaging spectrum of septic brain embolization demonstrated in twelve patients. Journal of Neuroimaging 9 (1999): 78-84.
- Kastenbauer S, Pfister HW, Wispelwey B, et al. Brain abscess. Infections of the Central NervousSystem (3rd edition) Scheld WM, Whitley RJ, Marra CM (2004): 479-507.
- Dharkar SR, Sardana VR, Purohit D. Brain Abscess. Textbook of Neurosurgery: Ramamurthi and Tandon (3rd edition) 1 (2011): 695-705.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
