Paraneoplastic Pemphigus in A Patient with Chronic Lymphocytic Leukemia: A Case Report
Article Information
Arif Kus1, Abdulkerim Yild?z2*, Betul Erdem3, Murat Albayrak2, Cigdem Pala Ozturk2, Muzeyyen Gonul3
1University of Health Sciences, Diskapi Yildirim Beyazit Training and Research Hospital, Department of Internal Medicine, Ankara, Turkey
2University of Health Sciences, Diskapi Yildirim Beyazit Training and Research Hospital, Department of Hematology, Ankara, Turkey
3University of Health Sciences, Diskapi Yildirim Beyazit Training and Research Hospital, Department of Dermatology, Ankara, Turkey
*Corresponding Author: Dr. Abdulkerim Yild?z, Diskapi Yildirim Beyazit Training and Research Hospital, Department of Hematology, Ankara, Turkey
Received: 01 June 2018; Accepted: 19 June 2018; Published: 22 June 2018
Citation: Arif Kus, Abdulkerim Yildiz, Betul Erdem, Murat Albayrak, Cigdem Pala Ozturk, Muzeyyen Gonul. Paraneoplastic Pemphigus in A Patient with Chronic Lymphocytic Leukemia: A Case Report. Journal of Cancer Science and Clinical Therapeutics 2 (2018): 84-88.
View / Download Pdf Share at FacebookAbstract
Paraneoplastic pemphigus (PNP) is a rare and autoimmune mucocutaneous disease associated with underlying neoplasia. The diagnosis of PNP is often difficult since skin manifestations maybe initially similar to other dermatological disorders. The case is here reported of an 84-year old male diagnosed with PNP associated with CLL, who initially presented with severe diffuse erythematous lesions in the oral mucosa and nasal mucosa, and vesicular-bullous lesions on the trunk and extremities. The patient died due to respiratory failure and hypotension caused by acute PTE.
Keywords
Leukemia, Paraneoplastic pemphigus
Leukemia articles Leukemia Research articles Leukemia review articles Leukemia PubMed articles Leukemia PubMed Central articles Leukemia 2023 articles Leukemia 2024 articles Leukemia Scopus articles Leukemia impact factor journals Leukemia Scopus journals Leukemia PubMed journals Leukemia medical journals Leukemia free journals Leukemia best journals Leukemia top journals Leukemia free medical journals Leukemia famous journals Leukemia Google Scholar indexed journals Paraneoplastic pemphigus articles Paraneoplastic pemphigus Research articles Paraneoplastic pemphigus review articles Paraneoplastic pemphigus PubMed articles Paraneoplastic pemphigus PubMed Central articles Paraneoplastic pemphigus 2023 articles Paraneoplastic pemphigus 2024 articles Paraneoplastic pemphigus Scopus articles Paraneoplastic pemphigus impact factor journals Paraneoplastic pemphigus Scopus journals Paraneoplastic pemphigus PubMed journals Paraneoplastic pemphigus medical journals Paraneoplastic pemphigus free journals Paraneoplastic pemphigus best journals Paraneoplastic pemphigus top journals Paraneoplastic pemphigus free medical journals Paraneoplastic pemphigus famous journals Paraneoplastic pemphigus Google Scholar indexed journals malignancies articles malignancies Research articles malignancies review articles malignancies PubMed articles malignancies PubMed Central articles malignancies 2023 articles malignancies 2024 articles malignancies Scopus articles malignancies impact factor journals malignancies Scopus journals malignancies PubMed journals malignancies medical journals malignancies free journals malignancies best journals malignancies top journals malignancies free medical journals malignancies famous journals malignancies Google Scholar indexed journals lymphoma articles lymphoma Research articles lymphoma review articles lymphoma PubMed articles lymphoma PubMed Central articles lymphoma 2023 articles lymphoma 2024 articles lymphoma Scopus articles lymphoma impact factor journals lymphoma Scopus journals lymphoma PubMed journals lymphoma medical journals lymphoma free journals lymphoma best journals lymphoma top journals lymphoma free medical journals lymphoma famous journals lymphoma Google Scholar indexed journals chemotherapy articles chemotherapy Research articles chemotherapy review articles chemotherapy PubMed articles chemotherapy PubMed Central articles chemotherapy 2023 articles chemotherapy 2024 articles chemotherapy Scopus articles chemotherapy impact factor journals chemotherapy Scopus journals chemotherapy PubMed journals chemotherapy medical journals chemotherapy free journals chemotherapy best journals chemotherapy top journals chemotherapy free medical journals chemotherapy famous journals chemotherapy Google Scholar indexed journals polymorphous articles polymorphous Research articles polymorphous review articles polymorphous PubMed articles polymorphous PubMed Central articles polymorphous 2023 articles polymorphous 2024 articles polymorphous Scopus articles polymorphous impact factor journals polymorphous Scopus journals polymorphous PubMed journals polymorphous medical journals polymorphous free journals polymorphous best journals polymorphous top journals polymorphous free medical journals polymorphous famous journals polymorphous Google Scholar indexed journals mucocutaneous articles mucocutaneous Research articles mucocutaneous review articles mucocutaneous PubMed articles mucocutaneous PubMed Central articles mucocutaneous 2023 articles mucocutaneous 2024 articles mucocutaneous Scopus articles mucocutaneous impact factor journals mucocutaneous Scopus journals mucocutaneous PubMed journals mucocutaneous medical journals mucocutaneous free journals mucocutaneous best journals mucocutaneous top journals mucocutaneous free medical journals mucocutaneous famous journals mucocutaneous Google Scholar indexed journals neoplasia articles neoplasia Research articles neoplasia review articles neoplasia PubMed articles neoplasia PubMed Central articles neoplasia 2023 articles neoplasia 2024 articles neoplasia Scopus articles neoplasia impact factor journals neoplasia Scopus journals neoplasia PubMed journals neoplasia medical journals neoplasia free journals neoplasia best journals neoplasia top journals neoplasia free medical journals neoplasia famous journals neoplasia Google Scholar indexed journals Rituximab-Chlorambucil articles Rituximab-Chlorambucil Research articles Rituximab-Chlorambucil review articles Rituximab-Chlorambucil PubMed articles Rituximab-Chlorambucil PubMed Central articles Rituximab-Chlorambucil 2023 articles Rituximab-Chlorambucil 2024 articles Rituximab-Chlorambucil Scopus articles Rituximab-Chlorambucil impact factor journals Rituximab-Chlorambucil Scopus journals Rituximab-Chlorambucil PubMed journals Rituximab-Chlorambucil medical journals Rituximab-Chlorambucil free journals Rituximab-Chlorambucil best journals Rituximab-Chlorambucil top journals Rituximab-Chlorambucil free medical journals Rituximab-Chlorambucil famous journals Rituximab-Chlorambucil Google Scholar indexed journals stomatitis articles stomatitis Research articles stomatitis review articles stomatitis PubMed articles stomatitis PubMed Central articles stomatitis 2023 articles stomatitis 2024 articles stomatitis Scopus articles stomatitis impact factor journals stomatitis Scopus journals stomatitis PubMed journals stomatitis medical journals stomatitis free journals stomatitis best journals stomatitis top journals stomatitis free medical journals stomatitis famous journals stomatitis Google Scholar indexed journals
Article Details
1. Introduction
Paraneoplastic pemphigus (PNP) is a dermatosis which generally occurs secondary to lymphoproliferative malignancies such as non-Hodgkin's lymphoma (NHL), chronic lymphocytic leukemia (CLL) and Castleman's disease and thymoma [1]. Males are affected more often than females. The disease differs from classical pemphigus as it has polymorphous lesions (bullous, targetoid, lichenoid, eczematized) and severe mucosal involvement accompanied by resistant stomatitis [1, 2, 3]. The PNP case reported in this paper developed after the first cycle of Rituximab-Chlorambucil (RC) chemotherapy regimen for the treatment of CLL.
2. Case Presentation
An 84-year-old male patient with CLL was admitted to the Hematology Department with complaints of head and neck lesions. The patient had received the first cycle of RC chemotherapy two weeks previously and it was learned from the history that the lesions started 1 week after the chemotherapy. The physical examination of the patient revealed yellow crusted lesions with purulent discharge in the head and neck region, especially in the periorbital region, diffuse erythematous lesions in the oral mucosa and nasal mucosa, and vesicular-bullous lesions on the trunk and extremities. No other positive sign was detected in the examinations of other systems. The patient was first evaluated in the Outpatients Clinics of the Infectious Diseases and Dermatology Departments (Figure 1).
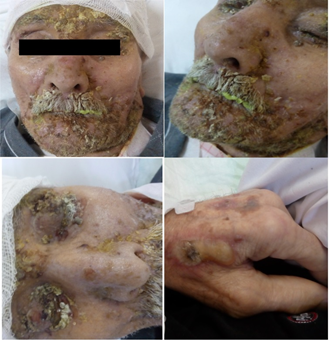
Figure 1: Vesiculo-bullous skin lesions with purulent discharge in the head and neck region, especially in the periorbital region.
The patients was hospitalised as disseminated herpes virus infection, streptococcal skin infection and gingivistomatitis were considered in the initial differential diagnosis. Fluconazole, acyclovir and sulbactam-ampicillin (SAM) treatments were all started empirically. Complete blood count revealed Hb:12.0 gr/dl, leukocyte:19000/mm3, lym:11000/ mm3, Plt:295000/ mm3, C-reactive protein:103 mg/dl, sedimentation rate:52 mm/s, urea:105 mg/dl, glucose:150 mg/dl, creatinine:1.66 mg/dl, Na:136 mEq/L, and K:5.4 mEq/L. No atypical cells except mature lymphocytosis and smudge cells were seen on the peripheral blood smear. IgM antibody of Herpes simplex virus (HSV) type I and II was negative, whereas IgG was positive. Biopsy of the skin lesions revealed intraepidermal suprabasal cleavage, epidermal acantholysis, and dyskeratotic keratinocytes. The skin biopsy samples for DIF testing showed linear deposition of IgG along the basal membrane. ELISA testing for antibody against desmoglein 3 was positive. The patient was diagnosed with PNP. Thus on the 9th day of admission, treatment was started of Rituximab at 1000 mg dose and methylprednisolone at 1 mg/kg/day. All empirical antibiotherapies were discontinued except SAM to prevent the forming of secondary bacterial skin infections. Despite these treatments, the lesions progressed so that patient was admitted to the Dermatology Department on day 13 of admission. During the follow-up period, the patient developed pulmonary thromboembolism. DMAH was started but the patient died due to severe respiratory failure 5 days after admission to the Dermatology Department.
3. Discussion
Paraneoplastic pemphigus (PNP) is a rare and autoimmune mucocutaneous disease associated with underlying neoplasia. Both humoral and cellular immunity play a role in the pathogenesis of PNP. It has several clinical and immunopathological features [1]. There have been no randomized control trials to guide the evidence-based treatment of PNP due to the rarity and high mortality and morbidity of the disease.
To date, all evidence of treatment efficacy has been obtained from case reports, small case series and expert advice [2]. PNP is associated with NHL (39%), CLL (18%), Castleman's disease (18%), carcinoma (9%), thymoma (6%), sarcoma (6%), and Waldenström macroglobulinemia (1%). Choi Y et al. analyzed 12 Korean patients with PNP and associated hematological-related neoplasms were determined in 11 patients, the most common being 4 with Castleman's disease [1]. In all these malignancy-associated cases, chemotherapy and radiotherapy applied for malignancy may play an additional role in the pathogenesis of the disease [4]. The association of PNP with CLL has been reported in many cases, particularly in recent years [5, 6, 7].
The diagnosis of PNP is often difficult since skin manifestations maybe initially similar to other dermatological disorders. The case reported here is of a patient with PNP associated with CLL, who initially presented with severe diffuse erythematous lesions in the oral mucosa and nasal mucosa, and vesicular-bullous lesions on the trunk and extremities. Streptococcal skin infection was considered most likely, so empirical antimicrobial agents were started. Some authors have identified three major and three minor diagnostic criteria for the diagnosis of PNP. The major criteria include a polymorphic rash, any accompanying malignancies, and positive detection of heterogeneous autoantibodies with immunofluorescent testing. The minor criteria include IgG and C3 deposition in direct immunofluorescence (DIF) assay in histopathology, the detection of acantholysis findings and detection of autoantibodies in the IFA. There must be 3 major criteria or 2 major and 2 minor criteria for the diagnosis of PNP [8, 9]. In the current case, there was a polymorphic rash accompanying CLL as major criteria and acantholysis, and linear IgG deposition in DIF testing as minor criteria.
The clinical manifestation of PNP differs from classical pemphigus as it shows acral, periocular involvement, severe and treatment-resistant stomatitis, targetoid, eczematous or lichenoid lesions [8]. In the current patient, periocular erosions were present in the acral areas, with erythematous plaques with bullae in the centers of the targetoid, especially in the acral areas, and stomatitis resistant to treatment. There were vacuolar changes in the basal layer and linear IgG deposition in addition to suprabasal cleavage.
PNP has a poor prognosis and patients generally die because of treatment-induced immunosuppression, respiratory failure and gastrointestinal bleeding. The 5-year overall survival rate has been reported to be 38% [10]. As first-line treatment, systemic steroids, rituximab and daclicuzumab are commonly used whereas cyclosporine, cyclophosphamide, azathiopurine, IVIG and plasmapheresis can be used as second-line treatment [2]. It is difficult to treat these cases with underlying associated malignancies and/or chemotherapy induced immunosuppression. Additional immunosuppressive drugs may exacerbate immunesuppression and cause severe infections. Recent reports have shown that the major reasons for mortality in PNP cases are sepsis, progression of malignancies and respiratory failure [1, 7, 10]. Venous thromboembolism is one of the most common causes of morbidity and mortality in cancer patients with incidence of approximately 11% in CLL cases [11]. Hyperleukocytosis may contribute to thrombosis in CLL patients. In the current case, the patient died due to respiratory failure and hypotension caused by acute PTE.
4. Conclusion
This report presents a PNP case which is rare but dangerous condition in a patient with CLL. As the management and treatment is difficult, early and definitive diagnosis is very important. Clinicians should aware of PNP as a differential diagnosis in patients with CLL when vesiculo-bulloeus skin lesions with purulent discharge develop.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Choi Y, Nam KH, Lee JB, et al. Retrospective analysis of 12 Korean patients with paraneoplastic pemphigus. The Journal of dermatology 39 (2012): 973-981.
- Frew JW, Murrell DF. Current management strategies in paraneoplastic pemphigus (paraneoplastic autoimmune multiorgan syndrome). Dermatologic clinics 29 (2011): 607-612.
- Czernik A, Camilleri M, Pittelkow MR, et al. Paraneoplastic autoimmune multiorgan syndrome: 20 years after. International journal of dermatology 50 (2011): 905-914.
- Anhalt GJ. Paraneoplastic pemphigus. (Edn 8th) New York: Mc Graw-Hill. (Lowell A. Goldsmith SIK, Barbara A. Gilchrest editor. Fitzpatrick’s Dermatology in General Medicine) (2012).
- Taddesse A, Tesfaye W. Chronic lymphocytic leukemia-associated paraneoplastic pemphigus (bullous pemphigoid-like). Ethiopian medical journal 51 (2013): 215-218.
- Adaszewska A, Ishii N, Dwilewicz-Trojaczek J, et al. Paraneoplastic pemphigus with anti-desmocollin 3 autoantibodies and chronic lymphocytic leukemia. Postepy dermatologii i alergologii 35 (2018): 113-115.
- Jiang Q, Zhang BH. Paraneoplastic pemphigus associated with chronic lymphocytic leukemia: A case report. Medicine 96 (2017): e6184.
- Frew JW, Murrell DF. Paraneoplastic pemphigus (paraneoplastic autoimmune multiorgan syndrome): clinical presentations and pathogenesis. Dermatologic clinics 29 (2011): 419-425.
- Sehgal VN, Srivastava G. Paraneoplastic pemphigus/paraneoplastic autoimmune multiorgan syndrome. International journal of dermatology 48 (2009): 162-169.
- Leger S, Picard D, Ingen-Housz-Oro S, et al. Prognostic factors of paraneoplastic pemphigus. Archives of dermatology 148 (2012): 1165-1172.
- Whittle AM, Allsup DJ, Bailey JR. Chronic lymphocytic leukaemia is a risk factor for venous thromboembolism. Leukemia research 35 (2011): 419-421.


 Impact Factor: * 4.1
Impact Factor: * 4.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 