Assessment of Peguero Lo-Presti Criteria for Electrocardiographic Diagnosis of LVH in Indian Subjects
Article Information
Suresh V Patted, Sanjay C Porwal, Sameer S Ambar, M R Prasad, Akshay S Chincholi*, Vishwanath Hesarur, Vaibhav Patil
Department of Medicine, Jawaharlal Nehru Medical College, Belagavi-590010, Karnataka, India
*Corresponding Author: Akshay S Chincholi, Department of Medicine, Jawaharlal Nehru Medical College, Belagavi-590010, Karnataka, India
Received: 03 April 2018; Accepted: 20 April 2018; Published: 07 May 2018
View / Download Pdf Share at FacebookAbstract
Background and objectives: The sensitivity of ECG to diagnose LVH (Left ventricular hypertrophy) is low. Peguero Lo-Presti have proposed new ECG criteria for LVH to improve the sensitivity of ECG while maintaining the high specificity when compared to older well-established criterion like Cornell voltage and Sokolow Lyon. The objective of this study was to evaluate Peguero Lo-Presti criteria in the diagnosis of LVH in patients with hypertension.
Methodology: 400 consecutive patients with hypertension who have visited the cardiology OPD (Out Patient Department) and have undergone ECG and 2D echocardiography were included in the study. Patients with valvular regurgitation (Grade II or higher), myocardial infarction, valvular stenosis, LV dysfunction, pericardial disease, COPD (Chronic obstructive pulmonary disease), bundle branch blocks, atrial fibrillation or flutter were excluded from the study.
Results: LVH was diagnosed in 192 (48%) of the patients by 2D echocardiography. Of the 192 patients, 104 patients had LVH based on Peguero Lo-Presti criteria with a sensitivity of 54.17%. Cornell Voltage criteria was positive in 76 out of 192 patients with a sensitivity of 39.58% and Sokolow-Lyon criteria was positive in 56 out of 192 with a sensitivity of 29.17%. The Peguero Lo-Presti ECG criteria had a higher sensitivity (54.17%) and specificity (91.35%) in the diagnosis of LVH by ECG.
Conclusion: Peguero Lo-Presti criteria to diagnose LVH has higher sensitivity and specificity compared to Sokolow-Lyon and Cornell voltage criteria.
Keywords
Electrocardiographic Diagnosis
Article Details
1. Introduction
Left ventricular hypertrophy is a marker of subclinical cardiac disease and helps in prognostication. It is a common finding in patients with hypertension and can be diagnosed either by electrocardiography or by echocardiography [1].
Population based studies have shown a strong association between hypertension and LVH. In fact, in severe forms of hypertension there is a >50% incidence of LVH while in milder forms it is <25% [2]. The Framingham studies have also established an age linked prevalence of LVH [3].
Left ventricular hypertrophy (LVH) secondary to arterial hypertension is a complex cardiac phenotype resulting from the response of myocyte and non-myocyte components to mechanical and neuro-humoral stimuli [4].
Various studies have shown that LVH independently predicts morbidity and mortality. LVH predisposes to heart failure, ventricular tachyarrhythmia, atrial fibrillation, ischemic stroke, embolic stroke and sudden cardiac death [5].
The sensitivity of all the well-established ECG criteria to diagnose LVH is low and is in the range of 7-35% with mild LVH and only 10-50% with moderate to severe LVH whereas the overall specificity is >90% [6].
To improve the sensitivity of ECG to diagnose LVH we evaluated the novel Peguero Lo-Presti criteria which has shown higher sensitivity when compared to older well established criterion like Cornell voltage and Sokolow Lyon criteria
2. Materials and Methods
This one cross-sectional study was conducted in the Department of Cardiology of a tertiary care centre in North Karnataka from May 2017 to December 2017. A total of 400 patients aged above 30 years presenting with hypertension to the cardiology OPD who underwent ECG and 2D echocardiography were included in the study. Patients with myocardial infarction, valvular heart disease (Grade II or higher), valvular stenosis, LV dysfunction, pericardial disease, COPD, bundle branch blocks, atrial fibrillation or flutter were excluded from the study. The patients fulfilling selection criteria were informed in detail about the nature of the study and a written informed consent was obtained before enrolment.
Detailed history was obtained and thorough clinical examination was done and the findings were recorded on a predesigned and pretested proforma. All patients have undergone 12 lead electrocardiography and transthoracic echocardiography.
2.1 2D echocardiography
Left ventricular mass was estimated by transthoracic echocardiography [7]. The LV was visualised with the patient lying in a modified left lateral decubitus position, with the ultrasound probe at the left parasternal window angled to visualise the heart in the long axis view. All the M-mode and 2D measurements were performed by the leading-edge-to-leading edge method, as described by the American Society of Echocardiography (ASE).
Left ventricular end-diastolic and end-systolic measurements were obtained according to recommendations by the American Society of Echocardiography [8,9]. Left ventricular mass was calculated by using the Devereux formula: left ventricular mass (g) = 0.80 x {1.04 x [(septal thickness + internal diameter + posterior wall thickness)3 ? (internal diameter)3]} + 0.6 g. The LV mass index was calculated according to body surface area. LVH was defined as a left ventricular mass index >115 g/m2 in male subjects and >95 g/m2 in female subjects [10].
2.2 ECG criterion
12 lead ECG was obtained from every patient. Using the PR segment as baseline, the tallest R and the deepest S wave in all the precordial and limb leads were recorded. The largest complex was selected if voltage differences within the same lead was present. The Peguero Lo-Presti criteria was calculated by adding SD to the S amplitude in V4 (SD + SV4). Cutoff values of SD + SV4 ≥ 2.3 mV for female subjects and ≥2.8 mV for male subjects were considered positive for LVH based on the recent study by Peguero JG et al. In cases in which the SD was found in lead V4, the S wave amplitude was doubled to obtain the value SD + SV4.
The Cornell voltage criteria was used as the main comparison given its reputation as the most accurate of the reported measurements [11]. The sex-specific Cornell voltage criteria was computed as the amplitude of R in aVL plus the amplitude of S or QS complex in V3 (RaVL + SV3) with a cutoff of >2.8 mV in men and >2.0 mV in women [12].
The Sokolow-Lyon voltage was obtained by adding the amplitude of S in V1 and the amplitude of R in V5 or V6 ≥ 3.5 mV (SV1 + RV5 or RV6) [13,14].
2.3 Statistical analysis
The categorical data was expressed as rates, ratios and percentages and comparison was done using chi-square test. Continuous data was expressed as mean ± standard deviation. The agreement between ECG criteria and 2D echocardiography was analysed with McNemar’s test and a ‘p’ value of less than or equal to 0.05 was considered as statistically significant. The accuracy of Peguero Lo-Presti criteria for the assessment of LVH was determined by estimating sensitivity, specificity, positive predictive value and negative predictive value.
3. Results
In this study 73.5% of the patients were males with male to female ratio of 2.77:1 (Graph 1). Age ranged between 35 to 89 years [Table 1] and most of the patients were aged between 61 to 70 years (38.50%) and the mean age was 63.79±10.36 years (Table 2 and 3). The clinical profile of the study population that is mean height, weight, ECG and 2D echocardiography parameters are as shown in Table 3. Based on 2D echocardiography, LVH was diagnosed in 48% of the patients (Graph 2). Based on ECG criteria that is, Peguero Lo-Presti, Cornell Voltage and Sokolow-Lyon criteria 30.50%, 24.50% and 21% of the patients were diagnosed to have LVH respectively (Table 3).
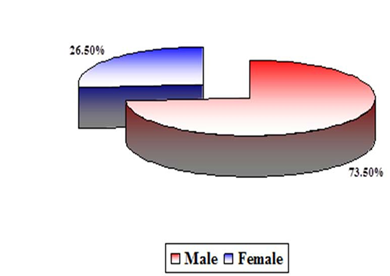
Graph 1: Distribution of patients according to sex
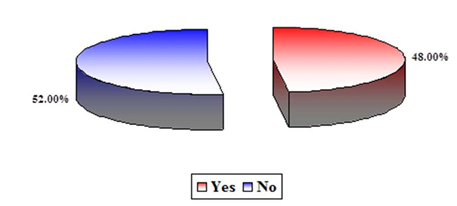
Graph 2: Distribution of patients according to the diagnosis of LVH based on LV mass index
|
Age (Years) |
Distribution (n=400) |
|
|
Number |
Percentage |
|
|
30 or less |
0 |
0.00 |
|
31 to 40 |
6 |
1.50 |
|
41 to 50 |
36 |
9.00 |
|
51 to 60 |
110 |
27.50 |
|
61 to 70 |
154 |
38.50 |
|
71 to 80 |
66 |
16.50 |
|
81 to 90 |
28 |
7.00 |
|
91 to 100 |
0 |
0.00 |
|
Total |
400 |
100.00 |
Table 1: Distribution of patients according to the age
|
Variables |
Distribution (n=400) |
Median |
Range |
||
|
Number |
Percentage |
Minimum |
Maximum |
||
|
Age (Years) |
63.79 |
10.36 |
63.50 |
35.00 |
89.00 |
|
Height (cms) |
160.36 |
4.35 |
160.00 |
150.00 |
170.00 |
|
Weight (Kg) |
63.21 |
6.31 |
62.00 |
51.00 |
84.00 |
|
Body Surface Area |
1.67 |
0.10 |
1.64 |
1.44 |
1.99 |
|
Duration of Hypertension (Years) |
7.78 |
6.62 |
7.00 |
0.08 |
76.00 |
|
Systolic blood pressure (mmHg) |
143.49 |
17.20 |
140.00 |
110.00 |
200.00 |
|
Diastolic blood pressure (mmHg) |
86.43 |
8.11 |
90.00 |
70.00 |
110.00 |
|
Pulse rate (/Minute) |
81.78 |
8.85 |
82.00 |
60.00 |
110.00 |
|
LVIDd |
4.13 |
0.35 |
4.10 |
3.20 |
4.90 |
|
PWTd |
1.25 |
0.12 |
1.25 |
1.00 |
1.50 |
|
IVSd |
1.31 |
0.15 |
1.30 |
0.50 |
1.60 |
|
LV mass by 2D |
193.63 |
39.65 |
189.50 |
97.00 |
283.00 |
|
115.98 |
25.06 |
113.00 |
59.00 |
172.00 |
|
|
SD |
1.48 |
0.34 |
1.40 |
1.00 |
2.60 |
|
SV4 |
0.97 |
0.25 |
0.90 |
0.10 |
1.60 |
|
SD + SV4 |
2.45 |
0.44 |
2.50 |
1.50 |
3.50 |
|
RaVL |
1.34 |
0.37 |
1.30 |
0.60 |
2.50 |
|
SV3 |
1.02 |
0.25 |
1.00 |
0.60 |
1.80 |
|
RaVL + SV3 |
2.36 |
0.47 |
2.30 |
1.50 |
3.40 |
|
SV1 |
1.20 |
0.28 |
1.20 |
0.60 |
2.00 |
|
RV5 or RV6 |
1.76 |
0.41 |
1.70 |
0.70 |
3.10 |
|
SV1 + RV5 or RV6 |
2.96 |
0.55 |
2.90 |
1.40 |
4.20 |
Table 2: Clinical profile of the study population
|
ECG criteria |
Findings |
Distribution (n=400) |
|
|
Number |
Percentage |
||
|
Peguero Lo-Presti criteria |
Yes (Raised SD + SV4) |
122 |
30.50 |
|
|
No (Normal SD + SV4) |
278 |
69.50 |
|
|
Total |
400 |
100.00 |
|
Cornell Voltage criteria for LVH |
Yes (Raised RaVL + SV3) |
98 |
24.50 |
|
|
No (Normal RaVL + SV3) |
302 |
75.50 |
|
|
Total |
400 |
100.00 |
|
Sokolow-Lyon criteria for LVH |
Yes (Raised SV1 + RV5 or RV6) |
84 |
21.00 |
|
|
No (Normal SV1 + RV5 or RV6) |
316 |
79.00 |
|
|
Total |
400 |
100.00 |
Table 3: Distribution of patients according to the diagnosis based on Peguero Lo-Presti criteria
Out of 192 patients with LVH based on 2D echocardiography, 104 were diagnosed to have LVH based on Peguero Lo-Presti criteria with strong agreement (p<0.001) between Peguero Lo-Presti criteria and 2D echocardiography for the diagnosis of LVH with sensitivity of 54.17%. Likewise, based on Cornell Voltage criteria 76 out of 192 were diagnosed to have LVH with sensitivity of 39.58% while based on Sokolow-Lyon criteria, 56 out of 192 were diagnosed to have LVH with sensitivity of 29.17%. The Peguero Lo-Presti ECG criteria yielded higher sensitivity (54.17%) and specificity (91.35%) in the diagnosis of LVH in patients with hypertension (Table 4).
|
ECG criteria |
ECG findings |
Coronary angiography findings |
Total |
Sensitivity (%) |
Specificity (%) |
PPV (%) |
NPV (%) |
p value |
|
|
Yes |
No |
||||||||
|
Peguero Lo-Presti criteria |
Yes |
104 |
18 |
122 |
54.17 |
91.35 |
85.25 |
68.35 |
<0.001 |
|
No |
88 |
190 |
278 |
|
|
|
|
|
|
|
Total |
192 |
208 |
400 |
|
|
|
|
|
|
|
Cornell Voltage criteria |
Yes |
76 |
22 |
98 |
39.58 |
89.42 |
77.55 |
61.59 |
<0.001 |
|
No |
116 |
186 |
302 |
|
|
|
|
|
|
|
Total |
192 |
208 |
400 |
|
|
|
|
|
|
|
Sokolow-Lyon criteria |
Yes |
56 |
28 |
84 |
29.17 |
86.54 |
66.67 |
56.96 |
<0.001 |
|
No |
136 |
180 |
316 |
|
|
|
|
|
|
|
Total |
192 |
208 |
400 |
|
|
|
|
|
|
Table 4: Accuracy of ECG criteria in predicting LVH considering LV mass index as gold standard
4. Discussion
The present study showed that, Peguero Lo-Presti criteria has higher sensitivity (54.17%), while maintaining higher specificity (91.35%) with higher diagnostic accuracy (73.50%) in the diagnosis of LVH among the patients with hypertension compared to the other two criterions that is Sokolow-Lyon criteria and Cornell Voltage criteria (Table 5).
Criterion |
Sensitivity |
Specificity |
PPV |
NPV |
Diagnostic accuracy |
|
Peguero Lo-Presti criteria |
54.17 |
91.35 |
85.25 |
68.35 |
73.5 |
|
Cornell Voltage criteria |
39.58 |
89.42 |
77.55 |
61.59 |
65.50 |
|
Sokolow-Lyon criteria |
29.17 |
86.54 |
66.67 |
56.96 |
59.00 |
Table 5: Comparison of accuracy of ECG criterion in predicting LVH considering LV mass index as gold standard
The Sokolow-Lyon criteria [14] has been evaluated in various studies to give sensitivity of 32% [14], 33% [14], 43% [15], while in this study the sensitivity was 29.17% which was in agreement with the previous studies. The Cornell voltage criteria has been evaluated to give sensitivity of 41% [16], and 28% [14] which was found to be 39.58% in the present study.
A retrospective study by Peguero JG et al. [17] in 2017 which devised the Peguero Lo-Presti criteria also reported sensitivity of 62% with specificity of 90% with strong agreement (p<0.011). The cut-off values determined by ROC obtained were ≥2.3 mV for females and ≥2.8 mv for males. In this study we used the same cut off values as that of Peguero JG et al. [17] and found higher sensitivity and specificity compared to other two criterions viz. Sokolow-Lyon and Cornell voltage criteria [14].
LVH is determined by an increase in LV mass, which can be estimated by the electrical voltage changes detected on 12 lead ECG. This makes 12 lead ECG an acceptable surrogate to detect LVH [17].
The sum of SD + SV4 had a better diagnostic value to detect LVH over the traditional LVH criteria [17].
The cardiac electrical voltage does not depend on the amount of myocardium alone, But, it also depends on the distance of LV cavity ? lead electrode, the location of the surface electrode, individual differences of antrophometry, myocardial fibrosis, and pulmonary pathology [17,18]. Day to day variation of ECG voltage has been described [13,20]. All of these factors may reduce the diagnostic accuracy of surface electrocardiography to diagnose LVH. Given the above drawbacks, any single lead showing the maximum voltage increase is more sensitive in identifying an LV mass, instead of using any fixed lead criteria.
Overall our study showes that, Peguero Lo-Presti criteria[17] has higher sensitivity and specificity in the electrocardiographic diagnosis of LVH compared to Sokolow-Lyon [14] and Cornell voltage criteria considering LV mass index by 2D Echocardiography as reference standard. However, these observations require further validation due to the potential limitations of this study that it is a single centre study and relatively smaller sample size. Another limitation is that the LV mass and LV mass index were estimated by using two-dimensional echocardiography and the main determinant of LVH in this study was the left ventricular mass. Though, echocardiography is known to have good reproducibility for the diagnosis of LVH and remains the most frequently used method in clinical practice [21]. It is reported that, 2D echocardiography ignores the left ventricular hypertrophy that occurs in initial stages and this may contribute to the discrepancies [22,23].
- Elias MF, Sullivan LM, Elias PK, D'Agostino RB, Wolf PA, Seshadri S, et al. Left ventricular mass, blood pressure, and lowered cognitive performance in the Framingham offspring. Hypertension 49 (2007): 439-45.
- Post WS, Larson MG, Levy D. Impact of left ventricular structure on the incidence of hypertension: the Framingham Heart Study. Circulation 90 (1994): 179-185.
- Hammond IW, Devereux RB, Alderman MH, Lutas EM, Spitzer MC, et al. The prevalence and correlates of echocardiographic left ventricular hypertrophy among employed patients with uncomplicated hypertension. J Am Coll Cardiol 7 (1986): 639-650
- C Diez J, Frohlich E. A translational approach to hypertensive heart disease. Hypertension 55 (2010): 1-8.
- Mann DL, Bonow RO, Zipes DP, Braunwald E, Libby P. Braunwalds Heart Disease ? A textbook of cardiovascular medicine 10th ed., New Delhi; Saunders, 2015.
- Barrios V, Escobar C, Calderon A, Ribas L, Marti D, Asin E. Prevalence of left ventricular hypertrophy detected by Cornell voltage-duration product in a hypertensive population. Blood Press 17 (2008): 110-115.
- Bacharova L, Ugander M. Left ventricular hypertrophy: the relationship between the electrocardiogram and cardiovascular magnetic resonance imaging. Ann Non-invasive Electrocardiol 19 (2014): 524-533.
- Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29 (2016): 277-314.
- Sahn D, De Maria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 58 (1978): 1072-1083.
- Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of, Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 17 (2016): 412.
- Schillaci G, Verdecchia P, Borgioni C, Ciucci A, Guerrieri M, et al. Improved electrocardiographic diagnosis of left ventricular hypertrophy. Am J Cardiol 74 (1994): 714-719.
- Casale PN, Devereux RB, Kligfield P, Eisenberg RR, Miller DH, et al. Electrocardiographic detection of left ventricular hypertrophy: development and prospective validation of improved criteria. J Am Coll Cardiol 6 (1985): 572-580.
- Hancock EW, Deal BJ, Mirvis DM, Okin P, Kligfield P, Gettes LS. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part V: electrocardiogram changes associated with cardiac chamber hypertrophy: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 53 (2009): 992-1002.
- Sokolow M, Lyon TP. The ventricular complex in right ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J 37 (1949): 161-186.
- Okin PM, Roman MJ, Devereux RB, Kohsaka S. Electrocardiographic identification of increased left ventricular mass by simple voltage-duration products. J Am Coll Cardiol 25 (1995): 417-423.
- Devereux RB, Dahlof B, Levy D, Pfeffer MA. Comparison of enalapril versus nifedipine to decrease left ventricular hypertrophy in systemic hypertension (the PRESERVE trial). Am J Cardiol 78 (1996): 61-65.
- Peguero JG, Lo Presti S, Perez J, Issa O, Brenes JC, et al. Electrocardiographic Criteria for the Diagnosis of Left Ventricular Hypertrophy 69 (2017): 1694-1703
- Bacharova L, Ugander M. Left ventricular hypertrophy: the relationship between the electrocardiogram and cardiovascular magnetic resonance imaging. Ann Noninvasive Electrocardiol 19 (2014): 524-533.
- Casale PN, Devereux RB, Alonso DR, Campo E, Kligfield P. Improved sex-specific criteria of left ventricular hypertrophy for clinical and computer interpretation of electrocardiograms: validation with autopsy findings.Circulation 75 (1987): 565-572.
- Angeli F, Verdecchia P, Angeli E, Poeta F, Sardone M, et al. Day-today variability of electrocardiographic diagnosis of left ventricular hypertrophy in hypertensive patients. Influence of electrode placement. J Cardiovasc Med 7 (2006): 812-816.
- Palmieri V, Dahlöf B, DeQuattro V, Sharpe N, Bella JN, et al. Reliability of echocardiographic assessment of left ventricular structure and function: the PRESERVE study. Prospective Randomized Study Evaluating Regression of Ventricular Enlargement. J Am Coll Cardiol 34 (1999): 1625-1632.
- Bacharova L. Electrocardiography-left ventricular mass discrepancies in left ventricular hypertrophy: electrocardiography imperfection or beyond perfection? J Electrocardiol 42 (2009): 593-596.
- Narayanan K, Reinier K, Teodorescu C, Uy-Evanado A, Chugh H, et al. Electrocardiographic versus echocardiographic left ventricular hypertrophy and sudden cardiac arrest in the community. Heart Rhythm 11 (2014): 1040-1046.


 Impact Factor: * 3.5
Impact Factor: * 3.5 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 14.80%
Acceptance Rate: 14.80%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 