Physical Activity: COVID-19 Enemy
Article Information
Dimitrios I. Bourdas1*, Emmanouil D. Zacharakis2
1Department of Sports Medicine and Biology of Exercise, School Physical Education and Sport Science, National and Kapodistrian University of Athens, Greece
2School Physical Education and Sport Science National and Kapodistrian University of Athens, Greece
*Corresponding Author: Dimitrios I. Bourdas, Department of Sports Medicine and Biology of Exercise, School Physical Education and Sport Science, National and Kapodistrian University of Athens, 11 Kalvou, Egaleo, 12243, Greece
Received: 09 December 2020; Accepted: 30 December 2020; Published: 13 January 2021
Citation: Dimitrios I. Bourdas, Emmanouil D. Zacharakis. Physical Activity: COVID-19 Enemy. Archives of Clinical and Medical Case Reports 5 (2021): 84-90.
View / Download Pdf Share at FacebookAbstract
For much of mankind, the COVID-19 pandemic created an extraordinary condition, with a severe impact on almost all domains of life. Physical activity (PA) was no exception, and disturbing findings showing the deleterious effect of lockdown measures on PA were recorded in relevant studies conducted in several different countries. It appears that society has overlooked or underestimated the advantages of PA in developing a defense against the virus and the incremental trend of non-communicable diseases (NCDs), and the prevalence of physical inactivity has presented many major challenges to public health authorities. In this article, in the presence of COVID-19, we briefly remember and highlight the beneficial impact of a physically active life and daily exercise training on public health, even more so for the most vulnerable groups. In this respect, we should not underestimate the role of PA and non-exhaustive exercise as a countermeasure and an indirect therapeutic agent against the virus, as well as against NCDs and mental health issues arising from the COVID-19 crisis.
Keywords
Sedentary life; Exercise; Contagious disease; Inactivity; Public Health; SARS-CoV-2
Sedentary life articles; Exercise articles; Contagious disease articles; Inactivity articles; Public Health articles; SARS-CoV-2 articles
Sedentary life articles Sedentary life Research articles Sedentary life review articles Sedentary life PubMed articles Sedentary life PubMed Central articles Sedentary life 2023 articles Sedentary life 2024 articles Sedentary life Scopus articles Sedentary life impact factor journals Sedentary life Scopus journals Sedentary life PubMed journals Sedentary life medical journals Sedentary life free journals Sedentary life best journals Sedentary life top journals Sedentary life free medical journals Sedentary life famous journals Sedentary life Google Scholar indexed journals Exercise articles Exercise Research articles Exercise review articles Exercise PubMed articles Exercise PubMed Central articles Exercise 2023 articles Exercise 2024 articles Exercise Scopus articles Exercise impact factor journals Exercise Scopus journals Exercise PubMed journals Exercise medical journals Exercise free journals Exercise best journals Exercise top journals Exercise free medical journals Exercise famous journals Exercise Google Scholar indexed journals Inactivity articles Inactivity Research articles Inactivity review articles Inactivity PubMed articles Inactivity PubMed Central articles Inactivity 2023 articles Inactivity 2024 articles Inactivity Scopus articles Inactivity impact factor journals Inactivity Scopus journals Inactivity PubMed journals Inactivity medical journals Inactivity free journals Inactivity best journals Inactivity top journals Inactivity free medical journals Inactivity famous journals Inactivity Google Scholar indexed journals Public Health articles Public Health Research articles Public Health review articles Public Health PubMed articles Public Health PubMed Central articles Public Health 2023 articles Public Health 2024 articles Public Health Scopus articles Public Health impact factor journals Public Health Scopus journals Public Health PubMed journals Public Health medical journals Public Health free journals Public Health best journals Public Health top journals Public Health free medical journals Public Health famous journals Public Health Google Scholar indexed journals SARS-CoV-2 articles SARS-CoV-2 Research articles SARS-CoV-2 review articles SARS-CoV-2 PubMed articles SARS-CoV-2 PubMed Central articles SARS-CoV-2 2023 articles SARS-CoV-2 2024 articles SARS-CoV-2 Scopus articles SARS-CoV-2 impact factor journals SARS-CoV-2 Scopus journals SARS-CoV-2 PubMed journals SARS-CoV-2 medical journals SARS-CoV-2 free journals SARS-CoV-2 best journals SARS-CoV-2 top journals SARS-CoV-2 free medical journals SARS-CoV-2 famous journals SARS-CoV-2 Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals Sclerosis articles Sclerosis Research articles Sclerosis review articles Sclerosis PubMed articles Sclerosis PubMed Central articles Sclerosis 2023 articles Sclerosis 2024 articles Sclerosis Scopus articles Sclerosis impact factor journals Sclerosis Scopus journals Sclerosis PubMed journals Sclerosis medical journals Sclerosis free journals Sclerosis best journals Sclerosis top journals Sclerosis free medical journals Sclerosis famous journals Sclerosis Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals tomography articles tomography Research articles tomography review articles tomography PubMed articles tomography PubMed Central articles tomography 2023 articles tomography 2024 articles tomography Scopus articles tomography impact factor journals tomography Scopus journals tomography PubMed journals tomography medical journals tomography free journals tomography best journals tomography top journals tomography free medical journals tomography famous journals tomography Google Scholar indexed journals
Article Details
1. Introduction
One of the world's leading causes of preventable death is the lack of physical activity (PA) per se [1-5]. Recent researches show the effects of exercise against non-communicable diseases (NCDs: cardiovascular diseases, cancers, chronic respiratory diseases and diabetes) as an adjuvant therapeutic agent [6,7], positively related to decreased mortality and increased quality of life, and negatively linked to the incidence or effect of diseases [8,9]. The continuation of daily exercise and PA in a secure home setting should therefore be a priority during the COVID-19 period for a healthy life. However, the COVID-19 pandemic created an unparalleled condition that had an unprecedented effect on most of humanity, in almost all domains of life [PA was no exception, [10-12]]. Due to the imminent rise in loneliness (self-isolation) and physical inactivity, organizations with a global scope instantly hurried to stress the importance of PA for society and to highlight pre-existing exercise guidelines for a more physically active life in order to prevent any impending adverse effects.
Unfortunately, the well-documented advantages of PA, i.e. defense against the virus and against the development of NCDs [3], seem to have been mostly underestimated or generally neglected by the community and the current drastic policies, which have favored a substantial degree of inactivity (Figure 1), [10-12]. More specifically, a series of very recent studies have demonstrated the deleterious impact of the COVID-19 restrictive orders to stay at home and avoid wider socialization on PA [13–17] and a clear association on overall negative change in PA (Figure 2), [10-12]. In any case, during and after lockdown the dominance of physical inactivity has posed many great challenges to health and sport officials, medical professionals and practitioners, professional and recreational athletes and the community. For these reasons, we would like to highlight the benefit of physically active life and daily exercise training (not intense or exhaustive) for public health, especially for the most vulnerable groups (people with serious underlying health conditions or elderly) [3,18,19].
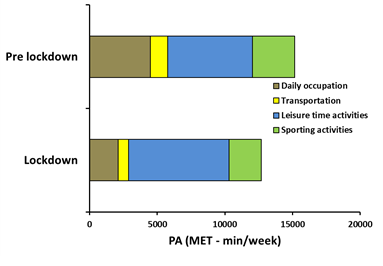
Figure 1: Physical activities by daily occupation, transportation to and from daily occupation, leisure time activities, and regular sporting activities, on a weekly basis in Greek adults (n=8495), [12]. The 95%CI of change in overall PA (from the Pre lockdown to Lockdown conditions) was –17.3 to –15.4. Abbreviations: CI, confidence interval; PA, physical activity.
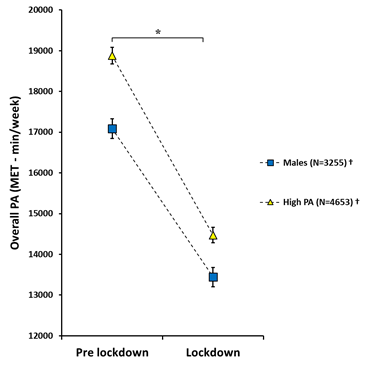
Figure 2: Overall PA (daily occupation, transportation to and from daily occupation, leisure time activities, and regular sporting activities) pre and during COVID-19 lockdown conditions in Greek adults [12]. Data are presented as mean ± SE. * p < 0.05, significant difference in all groups between conditions. † p< 0.05, significant interaction effect of lockdown on the PA subgroups (Males and High PA). Abbreviations: MET, metabolic equivalent task (=3.5 mLO2/kg/min); PA, physical activity.
2. The Positive Effects of Physical Activity
In order to minimize the risk of COVID-19 spread in the population, physical distancing and self-isolation steps have been used in most countries worldwide. leading to intensified behavioral routines that contribute to physical inactivity [10-12], potentially anxiety, depression and the growth of other NCDs [3,18,19]. Contrariwise, PA and routine daily exercise training are strategically necessary to maintain an acceptable health status and reverse the sedentary lifestyle [3].
A physically active lifestyle, outdoor sports activities and exercise may be a powerful combination to resolve the negative effects of the COVID-19 crisis on public health, particularly for the most vulnerable groups [19]. Physical activity amplifies the quality of life and has been negatively related to the incidence or effects of diseases and mortality. More precisely, in various diseases, PA strengthens the immune system and function, either in chronic systemic inflammation or after vaccination [20-22]. A regular exercise of mild to moderate intensity releases millions of immune cells (T cells, macrophages) and proteins (cytokines), which in turn allow the immune system to function better in inflammatory and stressful environments [20,23]. Physical activity is effective in both the prevention and treatment of NCDs, all of which increase the risk of morbidity and mortality among COVID-19 infected people [3,19]. Lack of PA and decreased daily energy expenditure, on the other hand, can contribute to a substantial increase in body fat, further loss and decrease in mitochondrial function, increased chronic oxidative stress and inflammation, deteriorating muscle, blood vessel and bone conditions and also degrade the already depleted cardiorespiratory reserves and immunity function of vulnerable groups [19,24,25]. In addition, inactivity per se is one of the world's main causes of preventable death [26].
As the pandemic COVID-19 outbreak continues, symptoms of psychological stress increase [18], causing imbalances between cortisol and other hormones, which adversely affect the biological response to inflammation and the immune system itself [27]. A PA lifestyle, on the contrary, has major mental health benefits: it decreases symptoms of depression and anxiety to COVID-19 pandemic stress and restores cortisol equilibrium [28]. Furthermore, frequent PA and daily exercise in individuals aged 65 years have beneficial effects on aging and related conditions, increase cognitive function and self-esteem, decrease the risk of falling, help prevent sarcopenia and dynapenia, and ultimately help prevent frailty [23].
As numerous new cases of COVID-19 appear daily in the world, many healthy individuals are being asked by official authorities to remain in self-quarantine at home. Being active during the COVID-19 pandemic crisis, while all national public health directives and general hygiene rules must be respected, is a challenge for everyone. Nevertheless, the World Health Organization has detailed recommendations on the manner and the amount of PA individuals should carry out to achieve favorable cardiovascular and metabolic health effects [24,29]. Briefly, infants (~1 year old) must be physically involved in activities several times a day [30]. Children ~3-4 years must be moderately to vigorously active for at least an hour a day and children aged ~5 years should be physically active for at least 180 minutes a day [30]. Children and adolescents (~5-17 years of age) should have at least 60 minutes of moderate-to-vigorous-intensity physical activity a day, including muscle and bone building exercises, at least 3 days a week [24]. Adults aged ≥ 18 years should have a total of at least 150 minutes of PA of moderate intensity during the week or at least 75 minutes of PA of vigorous intensity during the week, including 2 or more days a week of muscle-strengthening activities [24]. In order to improve balance and avoid falls, older adults (≥ 60 years) with poor mobility should have PA 3 or more days a week [24]. In the current COVID-19 pandemic situation, adults people in self-quarantine without any signs or diagnosis of acute respiratory disease, 150 min of moderate-intensity PA, or 75 min of vigorous-intensity PA, or a combination of both is recommended per week [29,31]. It is worth emphasizing that these guidelines can be followed at home, without special facilities and in a limited space. However, it is of paramount importance to keep in mind that any PA is always better than none.
3. Conclusion
Despite the fact that intensive efforts have been made worldwide to find a pharmaceutical agent and vaccine to battle COVID-19, the value of PA and non-exhaustive exercise as countermeasures and adjuvant therapeutic agents against the virus, NCDs and mental health disorders arising from the COVID-19 crisis should not be underestimated. Therefore, daily PA and exercise during the COVID-19 pandemic in a safe environment for a healthy life is absolutely necessary.
Authors’ Contributions
All authors contributed to writing this manuscript. All authors have read and approved the final version of this manuscript and agree with the order of presentation of the authors.
Declaration of Conflicting Interests
The authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
References
- Lopez AD, Mathers CD, Ezzati M, et al. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. The Lancet 367 (2006): 1747-1757.
- Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Comprehensive Physiology 2 (2011): 1143-1211.
- Durstine JL, Gordon B, Wang Z, et al. Chronic disease and the link to physical activity. Journal of Sport and Health Science 2 (2013): 3-11.
- Word Health Organization. Physical activity [Internet]. 2018 [cited 2020 Nov 11]. Available from: https://www.who.int/news-room/fact-sheets/detail/physical-activity
- Word Health Organization. Physical inactivity a leading cause of disease and disability, warns WHO [Internet]. 2020 [cited 2020 Nov 11]. Available from: https://www.who.int/news/item/04-04-2020-physical-inactivity-a-leading-cause-of-disease-and-disability-warns-who
- Kujala UM. Evidence on the effects of exercise therapy in the treatment of chronic disease. British Journal of Sports Medicine 43 (2009): 550-555.
- Pedersen BK, Saltin B. Exercise as medicine–evidence for prescribing exercise as therapy in 26 different chronic diseases. Scandinavian Journal of Medicine & Science in Sports 25 (2015): 1-72.
- O'Donovan G, Blazevich AJ, Boreham C, et al. The ABC of Physical Activity for Health: a consensus statement from the British Association of Sport and Exercise Sciences. Journal of Sports Sciences 28 (2010): 573-591.
- Reiner M, Niermann C, Jekauc D, et al. Long-term health benefits of physical activity–a systematic review of longitudinal studies. BMC Public Health 13 (2013): 1-9.
- Bourdas D, Zacharakis E. Impact of lockdown on physical activity in the early COVID-19 presence: Greece national cross-sectional study. Available at SSRN 3619812 (2020).
- Bourdas DI, Zacharakis ED. Evolution of changes in physical activity over lockdown time: Physical activity datasets of four independent adult sample groups corresponding to each of the last four of the six COVID-19 lockdown weeks in Greece. Data in Brief 32 (2020): 106301.
- Bourdas DI, Zacharakis ED. Impact of COVID-19 Lockdown on Physical Activity in a Sample of Greek Adults. Sports 8 (2020): 139.
- Gallo LA, Gallo TF, Young SL, et al. The impact of isolation measures due to COVID-19 on energy intake and physical activity levels in Australian university students. medRxiv (2020).
- Constandt B, Thibaut E, De Bosscher V, et al. Exercising in Times of Lockdown: An Analysis of the Impact of COVID-19 on Levels and Patterns of Exercise among Adults in Belgium. International Journal of Environmental Research and Public Health 17 (2020): 4144.
- Maugeri G, Castrogiovanni P, Battaglia G, et al. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 6 (2020): e04315.
- Qin F, Song Y, Nassis GP, et al. Physical activity, screen time, and emotional well-being during the 2019 novel coronavirus outbreak in China. International Journal of Environmental Research and Public Health 17 (2020): 5170.
- Barwais FA. Physical Activity at Home During the COVID-19 Pandemic in the Two Most-affected Cities in Saudi Arabia. The Open Public Health Journal 13 (2020).
- Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet (2020).
- Maffetone PB, Laursen PB. The perfect storm: Coronavirus (Covid-19) pandemic meets overfat pandemic. Frontiers in Public Health 8 (2020): 135.
- Nieman DC, Wentz LM. The compelling link between physical activity and the body's defense system. Journal of Sport and Health Science 8 (2019): 201-217.
- Simpson RJ, Campbell JP, Gleeson M, et al. Can exercise affect immune function to increase susceptibility to infection?. Exercise Immunology Review 26 (2020): 8-22.
- Woods JA, Keylock KT, Lowder T, et al. Cardiovascular exercise training extends influenza vaccine seroprotection in sedentary older adults: the immune function intervention trial. Journal of the American Geriatrics Society 57 (2009): 2183-2191.
- Jiménez-Pavón D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people. Progress in Cardiovascular Diseases (2020).
- Word Health Organization. Global Recommendations on Physical Activity for Health. WHO Press. World Heal. Organ. Geneva: WHO Library Cataloguing-in-Publication Data (2010).
- Kraemer J. Natural course and prognosis of intervertebral disc diseases. International Society for the Study of the Lumbar Spine Seattle, Washington, June 1994. Spine 20 (1995): 635-639.
- Word Health Organization. Draft action plan for the prevention and control of noncommunicable diseases 2013–2020 [Internet]. SIXTY-SIXTH WORLD Heal. Assem (2013): p.1–50.
- Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychological Bulletin 130 (2004): 601.
- Fox KR, Stathi A, McKenna J, et al. Physical activity and mental well-being in older people participating in the Better Ageing Project. European Journal of Applied Physiology 100 (2007): 591-602.
- Word Health Organization. Coronavirus disease (COVID-19): Staying active [Internet]. 2020 [cited 2020 Nov 11]. Available from: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-staying-active
- Word Health Organization. WHO Guidelines on physical activity, sedentary behaviour [Internet]. World Heal. Organ. Geneva; 2019. Available from: https://apps.who.int/iris/bitstream/handle/10665/325147/WHO-NMH-PND-2019.4-eng.pdf?sequence=1&isAllowed=y%0A
http://www.who.int/iris/handle/10665/311664%0Ahttps://apps.who.int/iris/handle/10665/325147 - Word Health Organization. Stay physically active during self-quarantine [Internet]. 2020 [cited 2020 Nov 11]. Available from: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/publications-and-technical-guidance/noncommunicable-diseases/stay-physically-active-during-self-quarantine?fbclid=IwAR2RQYVYBnmpDCMjBwqmoz0hZxzmit_9yKzXu6ZhjGNywRTEzWOUQefU8


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
