Plant-Based Diet to Reverse/ Regress Vulnerable Plaque: A Case Report and Review
Article Information
Dasaad Mulijono1,2,3*, Albert M Hutapea2,4, I Nyoman E Lister2,5, Mondastri K Sudaryo6, and Helwiah Umniyati7
1Department of Cardiology, Bethsaida Hospital, Tangerang-Indonesia
2Indonesian College of Lifestyle Medicine, Indonesia
3Department of Cardiology, Faculty of Medicine, Prima University, Medan-Indonesia
4Department of Pharmacy, Faculty of Life Sciences, Advent University, Bandung-Indonesia
5Department of Biomolecular and Physiology, Faculty of Medicine, Prima University, Medan-Indonesia
6Department of Epidemiology, Faculty of Public Health, University of Indonesia, Jakarta-Indonesia
7Department of Community Nutrition, Faculty of Dentistry, Yarsi University, Jakarta-Indonesia
*Corresponding Author: Prof. Dr. Dasaad Mulijono, Department of Cardiology, Bethsaida Hospital, Tangerang-Indonesia
Received: 05 May 2024; Accepted: 17 May 2024; Published: 26 June 2024
Citation: Dasaad Mulijono, Albert M Hutapea, I Nyoman E Lister, Mondastri K Sudaryo, and Helwiah Umniyati. Plant-Based Diet to Reverse/ Regress Vulnerable Plaque: A Case Report and Review. Archives of Clinical and Medical Case Reports. 8 (2024): 126-135.
View / Download Pdf Share at FacebookAbstract
A considerable proportion of fatalities resulting from acute myocardial infarction (AMI) occur suddenly in asymptomatic patients. Approximately 68% of AMIs are caused by coronary stenosis ≤ 50%, which is most likely due to the rupture of vulnerable plaques (VPs). A 55-year-old asymptomatic cardiologist who had been following preventive measures according to international guidelines and had reasonable metabolic-laboratory parameters underwent a cardiac check-up involving the use of coronary artery calcium (CAC) and computed tomography coronary angiography (CTCA), which revealed the presence of VP causing 50% stenosis in his proximal left anterior descending artery (LAD). Recognizing that his previous preventive measures, which were adopted from the guidelines, had failed to protect him from developing atherosclerosis, he chose to adopt a plant-based diet (PBD) while continuing on optimal medical therapy (OMT). After three years, there was a substantial regression in his CAC score and stenosis. The PBD program he adopted was specifically designed, taking into consideration the quality, quantity, and method of food processing, as well as the consumption of specific vitamins and minerals. This case report and review emphasize the importance of prevention to avoid the development of atherosclerosis or VP, especially in high-risk patients. Prevention involves not only the use of OMT but also the modification of one's lifestyle, particularly the adoption of a healthy and proper diet that can prevent the development of atherosclerosis, reduce inflammation, and promote the regression and stabilization of vulnerable plaques if they have already formed. The case also highlights CAC and CTCA as the most efficient, practical, reliable, safe, and economical methods for identifying VPs. The tests are widely accessible in most cardiac centers. Thus, we offer a novel, non-invasive diagnostic method for diagnosing VP and provide the most practical, efficient, and affordable approach to regress or stabilize VP. Consequently, the current guidelines for managing chronic coronary syndrome (CCS) are recommended to be revised. Specifically, it is suggested that the guidelines be amended to advise high-risk asymptomatic patients to consider the role of CAC and CTCA. Additionally, it is recommended that lifestyle modifications be reinforced in conjunction with OMT to manage VP and promote regression and reversal of atherosclerosis effectively.
Keywords
Plant-based diet; Lifestyle; Optimal medical therapy; Vulnerable plaque; Atherosclerosis; Coronary artery calcification; and Computed tomography coronary angiography
Article Details
1. Introduction
More than 50% of fatalities caused by AMI occur in individuals who are not exhibiting any symptoms, which is referred to as silent ischemia [1]. Furthermore, approximately 68% of AMI occur due to a lesion in the vessel that is less than 50% occluded, which is most likely due to the rupture of a VP [2]. There has been considerable debate over the screening of asymptomatic patients who may have coronary artery disease (CAD) in order to prevent major adverse cardiovascular events (MACE) or death [3]. Critics have raised concerns about the reliability of using a dynamic exercise test (DET) for certain individuals, citing the limited negative predictive values associated with these tests. This is because some individuals may not be able to reach the test target, which could affect the accuracy of the results [4]. Moreover, individuals with VP may display normal results on physiological tests, including the fractional follow reserve (FFR) [5]. In accordance with the most recent publications and expert opinions, it is now recommended to screen asymptomatic individuals for CAD using CAC and CTCA, particularly those with a substantial risk [6-9]. Nowadays, it is easy to access such tests. This tool and risk stratification are crucial for determining the appropriate preventive therapy for asymptomatic patients [10]. Our case involves an asymptomatic 55-year-old interventional cardiologist who possesses significant coronary risk factors, including familial history of CAD/ cerebrovascular disease (CVD) and elevated low-density lipoprotein (LDL), low high-density lipoprotein (HDL) and increased lipoprotein a or Lp (a) levels. Even though DETs consistently yielded favorable outcomes, this patient elected to undergo CAC and CTCA screenings on a regular basis in contravention of the guidelines. Before the presentation, he always produced normal results for both CAC and CTCA on his regular cardiac check-ups. However, the most recent screening revealed positive CAC and intermediate stenosis in his LAD. Upon further evaluation, a VP was discovered. He decided to integrate a PBD regimen along with the OMT that he had been practicing for more than three decades prior to his VP diagnosis. According to extensive research, it has been proven that PBDs not only hinder the development of atherosclerosis but also encourage the regression of existing coronary plaques [11-17], which led to the patient’s decision to incorporate PBD in his treatment regimen. The administration of OMT is continued mostly on the basis of lipid studies, which suggest that it can minimally regress atherosclerotic plaque [18-20,22]. He used anti-platelet medications to decrease his risk of acute coronary syndrome (ACS) [21,22]. In the discussion, we will explore the current predicament of managing asymptomatic high-risk CAD patients, the limitations of relying solely on OMT to prevent atherosclerosis development, and the importance of adopting a healthy lifestyle, specifically following a correct diet to reduce inflammation and regress or stabilize VP. We will review the current state-of-the-art approaches for diagnosing and managing VP and compare them with our proposed approaches. We will also discuss how PBDs can regress or stabilize VPs. Lastly, we will address the dilemma faced by the medical community in adopting lifestyle modifications, particularly the implementation of PBDs.
2. Case Description
Dr. X, a 55-year-old interventional cardiologist and an asymptomatic individual, underwent a CAC and CTCA as part of his regular cardiac checkup. Two years ago, his CTCA yielded normal results with a calcium score of zero, and his most recent DET also indicated normal findings. Upon presentation at the cardiology clinic, he had a BMI of 23 kg/mm2, a systolic blood pressure of 110 mmHg, a diastolic blood pressure of 76 mmHg, and a heart rate (HR) of 64 pulses per minute. His blood glucose level was 95 mg/dL, and his serum creatinine was 0.9 mg/dL. The laboratory results showed HbA1C at 5.7%, LDL at 70 mg/dL, HDL at 38 mg/dL, Lp (a) at 40 mg/dL (desirable threshold of <14 mg/dL), and elevated hs-CRP of 3.0 mg/L which was three times the upper limit. There is a significant familial predisposition to cardiovascular disease, as both his parents experienced a heart attack and stroke at a tender age before reaching 40 years old. He has been following an omnivorous diet since childhood. He exercised regularly (> 150 minutes of moderate exercise per week) and maintained a low weight through restricted calorie intake. He has been taking statin for over three decades and ezetimibe 10 mg for more than 15 years, consistently maintaining his LDL levels in accordance with the American College of Cardiology (ACC)/ American Heart Association (AHA) guidelines. Prior to the commencement of lipid therapy, his LDL level was between 180-200 mg/dL. The initiation of statin medication was carried out by his professor of lipidology and his professor of cardiology during his internship in Australia. The assessment and quantification of his atherosclerotic plaque were accomplished using a 128-slice CTCA. During the procedure, a non-ionic contrast was administered, and his resting HR was 60 beats per minute, with a breath hold of 15 seconds. The CTCA revealed a calcium score of 58, concentrated in the proximal LAD, with a stenosis of approximately 50%. The plaque was characterized as calcified, fibrotic, and containing a large lipid core, filling the criteria of a VP. The plaque measurements were 24.2 mm3 for the calcified plaque, 96.4 mm3 for the fibrotic plaque, and 15 mm3 for the lipid core. To evaluate the physiological effects of his VP, the patient underwent DET and myocardial perfusion imaging scans, which produced normal findings.
He decided to enter a lifestyle program to regress/reverse his coronary atherosclerotic plaque. He changed his atorvastatin to rosuvastatin 20 mg and continued on 10 mg of ezetimibe. He started on 75 mg of clopidogrel to change his platelet hyperaggregation state to hypoaggregation. He took supplements (vitamin B12, vitamin D, and K2) as he went along with his lifestyle program (adopting a PBD, avoiding unhealthy foods, and continuing regular exercise, at least 150 minutes of moderate-intensity exercise per week). At the PBDs site, patients carefully evaluate the selection of foods, considering their quality, quantity, and processing methods. For instance, raw vegetables are preferred over cooked ones to preserve nitrate content. For breakfast, the patient would have a one-liter blender containing 400 grams of raw vegetables such as spinach, arugula, celery, parsley, or any vegetables rich in fiber, nitrates, carotenoids, and phytochemicals. This will be mixed with 400 grams of fresh fruits such as pomegranates, berries, grapes, or fruits full of antioxidants and phytonutrients. Two tablespoons of flaxseeds or chia seeds were added to the blender and mixed to fulfill the omega requirement. For lunch, he consumed 500-750 ml of porridge made from legumes, including 50g of soybeans, 100g of green beans, and 50g of barley, mixed with two dates for flavor. For dinner, he had a colorful fruit salad consisting of apples, kiwis, oranges, mangos, and berries paired with 100-200 grams of whole grains mixed with 200-300 ml of soy or almond milk. The patient would also consume Indonesian spices like ginger, turmeric, clove, cinnamon, lemongrass, and fermented foods in his diet, which are rich in antioxidants and act as anti-inflammatories. Fruits and vegetables would be procured from supermarkets that offer good quality products. He drank coffee and green tea without any added sugar. Food restriction in terms of quantity is no longer required due to the satiating effect of PBD. Additionally, the patient consumed 250 micrograms of vitamin B12, 10,000 International Units of vitamin D, 360 micrograms of vitamin K2, and one multivitamin tablet that conformed to the recommended daily intake for an adult male. It is worth noting that the patient's vitamin D levels were maintained within the range of 60-80 nanograms per milliliter. Three years after implementing a lifestyle intervention, his BMI decreased to 21 kg/m2. Additionally, his blood pressure and pulse remained unchanged from three years prior. His HbA1C level significantly decreased to 5.2%, while his LDL cholesterol levels decreased to 50 mg/dL. His Lp(a) level decreased by 40%, and HDL cholesterol increased by 30%. His hs-CRP levels became normalized (one of the indicators of systemic inflammation), and he regularly measured his nitric oxide (NO) levels using an NO strip under his tongue [23], in which satisfactory readings were obtained. Additionally, he ensured that his urine readings remained alkaline most of the time (alkaline urine is one of the markers of following a correct PBD) [24]. His CAC/ CTCA after three years of follow-up showed a calcium score of 42, which had regressed by 28% from 58, and his proximal LAD stenosis, which was previously measured 50%, had decreased to 30%, a regression of 40%. The measurements of the plaque calcification, which amounted to 17.3 mm3, showed a regression of approximately 30%. The fibrotic plaque, amounting to 57.8 mm3, showed a regression of 40%, while the lipid core, amounting to 7.3 mm3, experienced a decrease of 50%. These results can be seen in Figure 1.
3. Discussion
The case report highlights the challenges faced by individuals who, despite being asymptomatic and having negative DET, turn out to have VP on CAC and CTCA screening. Consequently, if the current international guidelines, which recommend managing such asymptomatic individuals based on a negative treadmill test, are followed, this patient may have unfavorable consequences (experiencing an acute coronary syndrome or sudden death) [25,26]. Individuals who have received negative results from DET screenings have frequently experienced cardiac incidents, including fatalities, causing unease within our community. To address this issue, our community has been implementing the use of CAC and CTCA as part of coronary risk assessments for asymptomatic patients in Indonesia for several years. It is important to note that the cost of conducting these tests is covered by private insurance. Not all aspects of health services provided in low-mid-income countries are considered inferior to those provided in high-income countries. Our case report is an example of such a discrepancy. CAC and CTCA are typically reserved only for patients displaying symptoms in the United States. However, recent publications and expert opinions have highlighted their use for high-risk CAD patients in wealthy countries [6-9]. As a result, the scope of current cardio-prevention guidelines for managing asymptomatic patients warrants further investigation. It is crucial to acknowledge the limitations present within these guidelines, such as the absence of tailored-personalized care, the slow incorporation of new knowledge, and the over-cautious of therapeutic approaches taken. Additionally, the guidelines themselves are often extensive and complex, making them less interesting to numerous practitioners who must also navigate multiple sets of recommendations [27]. The individual, in this case, possesses an unusually large number of risk factors for a coronary event, including a family history of cardiovascular events occurring before the age of 40 and a diagnosis of familial hyperlipidemia, with markedly elevated levels of LDL, low HDL and increased Lp(a) cholesterols. Many practitioners may fail to identify such high-risk patients and may not consider conducting CAC or CTCA in asymptomatic patients with negative DET results. Furthermore, it is well-established that over half of all coronary events occur in individuals who are asymptomatic and lack a prior history of CAD [1]. Thus, patients without chest pain but deemed high-risk may be barred from undergoing CAC and CCTA studies [28], which could potentially have negative consequences for their health. Another important consideration is that a substantial proportion of individuals with CAD may actually be experiencing cardiac symptoms, but they are often misclassified as asymptomatic or labeled as having atypical non-cardiac chest pain. It is essential to consider these factors when managing patients with CAD. Undoubtedly, it is essential to evaluate the use of CTCA for individuals engaged in occupations that pose a considerable threat to the well-being of others, such as pilots [29]. In these situations, the possibility of experiencing a cardiac event during work duties makes the implementation of CTCA an imperative consideration. Similarly, it would be prudent to consider the feasibility of this screening approach for medical practitioners who carry out procedures where the operator's sudden cardiac event during the procedure could jeopardize the life of their patients.
Although the patient was following the statin regimen recommended by his Australian mentors to address his elevated LDL level, in accordance with the literature and previous guidelines [10,30], he still developed a vulnerable plaque. Before receiving his VP diagnosis, the patient had already implemented a diet in accordance with the guidelines, restricting his consumption of animal products, sugary foods, oils, and processed foods. He believed that these measures would be sufficient to prevent him from developing CAD. However, these efforts failed miserably to prevent the development of the patient’s atherosclerosis. All of his previous CAC and CTCA results were normal, but at the age of 55, his guideline-directed lifestyle changes and prescribed OMT were unable to halt the development of atherosclerosis. Although numerous early studies revealed regression with high doses of statins [19,20], there have been no subsequent studies to prove the effectiveness of long-term statin usage in the primary prevention of atherosclerosis development. This was the basis for the patient's decision to continue taking statins in the hope of boosting his PBD intervention in regressing and stabilizing his vulnerable plaque. While following a predominantly omnivorous diet, the patient found it difficult to maintain his LDL levels. To achieve an LDL level of 70 g/dL, he required 40 mg of atorvastatin in combination with 10 mg of ezetimibe. The high dose of statin sometimes elevated his liver transaminases, especially if his weight is increased. So, the patient maintained his weight to avoid fatty liver disease to safeguard his liver from statin side effects. The patient initiated the administration of clopidogrel, as per the guidelines for managing CCS patients [22], with the intent of transitioning from a state of hyperaggregation to hypoaggregation. The patient did not alter his exercise regimen since he had done physical activity per established guidelines and adhered to these recommendations. Following adopting a PBD, the patient could reduce his LDL levels to below 55 g/dL and decrease his Lp(a) by 40%. Although no studies have demonstrated that reducing Lp(a) levels can reverse atherosclerosis, the potential impact of PBDs in lowering Lp(a) and inducing regression warrants further exploration. His low BMI (21 kg/m2) has prevented him from experiencing elevated transaminases. Furthermore, the patient reported improved overall health, including not falling ill with the flu and recuperating from COVID-19 within five days, which he attributed to the PBD he had adopted. The above-mentioned case highlights the importance of altering one's diet to promote regression, as the patient had already taken lipid-lowering medication, adhered to recommended LDL levels, followed regular exercise routines, and, most importantly, modified his omnivorous diet in accordance with guidelines, yet still experienced vulnerable plaque. Thus, satisfactorily fulfilling the guidelines is not guaranteed in mitigating atherosclerotic development. At medical schools, minimal training in nutrition is provided to students, which is inadequate for them to implement lifestyle changes effectively upon becoming medical practitioners [32-34]. Despite the numerous studies that have demonstrated the benefits of PBD in managing atherosclerosis [35-37], many practitioners remain opposed to such recommendations due to their lack of nutritional knowledge, and the guidelines do not explicitly state that proper nutrition can lead to regression of atherosclerotic plaque [38]. For our case study patient, a medical specialist who possessed extensive medical knowledge, it took approximately one year to comprehend suitable food choices, the importance of vitamin intake, and the metabolic parameters to be monitored, as well as to develop the motivation necessary to adopt such a complex regimen and relinquish their previously enjoyed, unhealthy diet.
The selection of PBDs varies greatly, as evidenced by the patient's informed choices regarding their food's quality, quantity, and processing. Moreover, the patient asserted that his diet adequately incorporated both macro and micronutrients, encompassing the intake of vital vitamins and minerals. The PBDs have been subject to numerous critiques concerning their insufficient provision of vital nutrients, a factor that each individual should consider before adopting this dietary regimen [39-41]. Furthermore, it is crucial to understand which vitamins may aid in plaque regression. Research has demonstrated the significant role of vitamin D and vitamin K2 in regressing atherosclerotic plaques [42-45]. The patient routinely monitors his salivary NO levels and ensures his NO readings are satisfactory and his urine remains alkaline. These monitors are an indispensable component of precise PBD implementation. Based on the complexity of implementing such a diet, it has become evident that many physicians will likely fail to do so correctly when advising their patients to make dietary changes. Lifestyle modifications, particularly dietary adjustments, are strongly recommended as a first-line therapy in managing CCS [22]. However, the practical application of these guidelines in daily life often falls short of expectations due to the aforementioned factors. In addition, many physicians' limited knowledge of dietary nutrition and reluctance to engage in extended discussions with patients regarding these changes also contribute to this situation. Compared to traditional medical practices, a dietary approach is perceived as impractical because it is often challenging, time-consuming, and potentially offers less immediate gratification than interventions, surgeries, or medication prescriptions. However, providing patients with a thorough education on the intricacies of a complex diet is essential for effectively managing chronic conditions.
Most AMIs are linked to less than 50% stenosis, as demonstrated in a study [2]. This level of stenosis could indicate the presence of a VP, which is frequently overlooked during CTCA and may not receive the appropriate treatment. In recent years, CTCA has developed software to detect VP [46-48], as detailed in our case report. However, few hospitals in our country have an expert in interpreting VP obtained through CTCA. Thus, it is essential to have an experienced and knowledgeable radiologist in CTCA to recognize VP. A variety of advanced, invasive diagnostic tools are currently available for detecting VP, including IVUS in combination with OCT, or hybrid IVUS-OCT/OFDI, NIRS-IVUS (near-infrared spectroscopy), NIRF-IVUS (near-infrared fluorescence), IVPA-IVUS (molecular imaging intravascular photoacoustics), and TRFS-IVUS (time-resolved fluorescence spectroscopy) [49,50]. Although these advanced tools have demonstrated remarkable capabilities, they are not yet widely accessible, even in developed and affluent countries. This is largely due to their high cost, intrusive nature, and the fact that they are still in the research and development phase. Thus, our case has demonstrated that CAC and CTCA are non-invasive, effective, practical, cost-effective, safe, and reliable methods for diagnosing VP.
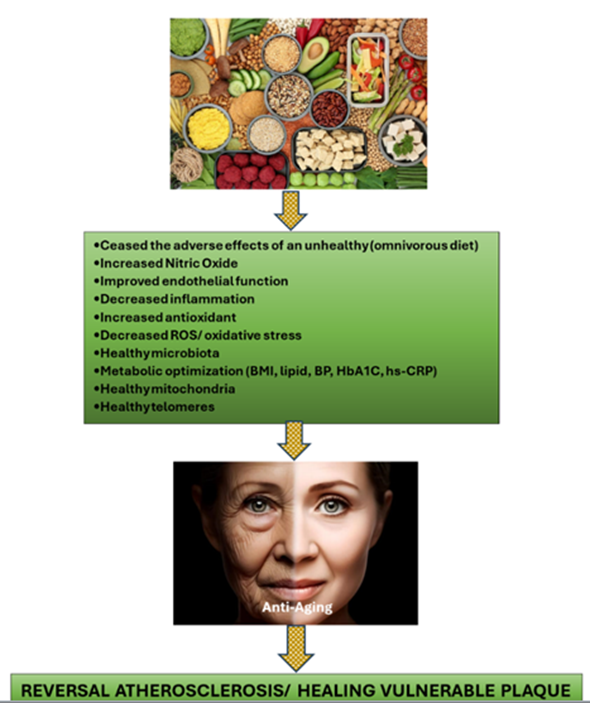
Experts have recently recommended using drug-eluting stent (DES) and drug-eluting balloon (DEB) technologies to manage VP. According to the primary report, these interventions are safe and effective in treating VP compared to only the OMT approach [51-54]. In our case study, the outcome experienced by the patient offers an opportunity for practitioners and their patients to consider an alternative approach to managing VP. We support the options chosen by the patient in our case report as they are practical and cost-effective while also adhering to the latest publications for managing CCS [22]. Instead of relying solely on intervention, the current guidelines recommend using OMT and lifestyle changes, which can significantly reduce healthcare costs. It is important to note that atherosclerosis is a systemic disease resulting from metabolic dysfunction and persistent inflammation rather than a localized process. Consequently, it should be classified as a metabolic chronic inflammatory condition. Patients who have experienced VP due to the atherosclerosis process have typically exhibited a state of metabolic disorder and systemic inflammation for a prolonged period. Therefore, it would not be prudent to rely solely on interventions such as stent implantation or DCB technology to manage this problem. Following extensive and intrusive intervention, failure to adequately control the patient's atherosclerosis on a systemic level may result in the recurrence of atherosclerotic plaques either at the original site or in new locations. The systemic process affecting the patient will persist. Therefore, it cannot be deemed appropriate to manage such individuals solely with OMT, as demonstrated by our patient's previous history, where OMT alone failed to prevent the development of his atherosclerosis. The systemic process can only be halted fully by changing our patient' lifestyles, most importantly, their unhealthy dietary habits. This explains why clinical trials that compared percutaneous coronary intervention (PCI) with OMT have produced disappointing results for PCI [55-57]. Interventional cardiologists frequently overlook the metabolic and systemic issues of their patients, which can result in a higher incidence of MACE after PCI. In addition, miscalculating VP can lead to incomplete revascularization, which can also contribute to MACE when comparing intervention with OMT in CCS patients [58]. Studies have demonstrated that complete revascularization is achieved in only approximately 50% of PCI cases [59-63], primarily due to inadequate VP management. Consuming diets high in sugar, devoid of fiber-phytonutrients, highly processed, and containing saturated fats and trans fats, cholesterol, and chemicals (pesticides, hormonal use in animal farms) can lead to a range of negative health outcomes, including elevated LDL cholesterol, obesity, and insulin resistance. Furthermore, these unhealthy dietary habits can also promote chronic inflammation, significantly contributing to VP development [64,65]. Hence, relying solely on OMT to manage atherosclerosis may not be entirely satisfactory, as the inflammatory process contributing to atherosclerotic plaque progression will persist. In our case study, the level of hs-CRP, which serves as an indicator of inflammation, was normalized only after the patient adhered to PBD. Eating healthy PBD with adequate supplementation will enhance our body's ability to fight against inflammation. Healthy foods such as vegetables, fruits, and legumes contain carotenoids, isoflavones, phytoestrogens, and phytosterols, which have been shown to prevent atherosclerosis. These polyphenols and phytochemicals' role in molecular signaling are anti-inflammatory, antiplatelet aggregation, inhibitor to VSMCs proliferation and migration, and safeguard for lipid oxidation [66,67]. Oxidized LDL (ox-LDL), in addition to its infamous role in causing atherosclerosis, also plays a significant part in developing VP [11], in which PBD has its role. The processes through which PBD aids in the regression of atherosclerotic plaque include enhancing NO availability, modifying the microbiota, repairing endothelial dysfunction, reducing inflammation, protecting against oxidative stress, fortifying mitochondria, and extending telomeres [58]. It is crucial for individuals who utilize PBD for regressing coronary plaque purpose, to pay close attention to their food choices and consume items that possess properties that suppress inflammation, combat oxidative stress, increase NO availability, support healthy microbiota, strengthen mitochondria, heal telomeres, and exhibit anti-thrombotic properties [68-74] as can be seen in Figure 2.
It has been three decades since Ornish et al. presented their famous atherosclerosis regression study [35]. Shortly thereafter, Esselstyn et al. revealed a picture that demonstrated a significant regression of coronary artery stenosis (Figure 3) [36]. However, no large studies have ever been conducted, particularly by interventional cardiologists, to clarify the role of a PBD in reversing atherosclerosis. Reading about the advantages of PBD in publications is not the same as personally experiencing the benefits of PBD treatment. Our case studies demonstrate the dramatic way in which the patient's life has changed, enabling him to lead the lifestyle movement in his career path in Indonesia, where lifestyle medicine was previously unpracticed. As with the former president of the ACC, Kim A. Williams, who used PBD to treat his hypertension successfully and subsequently promoted the practice, personal experience can serve as a powerful catalyst for change. The patient, an interventional cardiologist, initially expressed skepticism towards lifestyle modifications, as did his peers. However, after personally testing the PBD method, he became a fervent proponent of its use in interventional cardiology. He now leads initiatives to inform and promote PBD to both his patients and professional circle.
Conclusion
The case study underscored the importance of primary prevention in reducing the incidence of atherosclerosis. Implementing healthy lifestyle choices, particularly adopting the healthiest diet, at an early age is particularly important for individuals who are at a high risk of developing CHD. By halting the progression of atherosclerosis plaque earlier, future occlusion and complications can be prevented. It is important to note that high-risk asymptomatic patients can benefit from receiving CAC and CTCA evaluations to assess their risk for future coronary events and to identify the presence of VP. The evaluations are non-invasive and boast several benefits, including effectiveness, practicality, reliability, affordability, and high patient tolerability. Furthermore, they are widely accessible in many countries. Invasive treatments may not always be necessary for managing VP in asymptomatic patients; lifestyle changes, particularly the implementation of PBD, in our case, have been shown to offer regression and stabilization of these plaques in conjunction with OMT. However, OMT alone has been deemed insufficient in managing chronic inflammation, and CAD is widely recognized as a chronic inflammatory disease. Proper patient education regarding dietary changes requires deep comprehension of PBDs, specialized communication skills & techniques, and a willingness to educate and follow up with patients despite limited rewards. Physicians who have personally experienced the profound benefits of PBD interventions in treating dangerous diseases, such as VP, can serve as influential role models for the future adoption of lifestyle medicine, which, in this case, entails the application of PBDs. It is unclear whether knowledge exists regarding the use of PBD in mitigating chronic inflammatory diseases for the last three decades or its presence in human history since the beginning. As the Bible states, "The thing that hath been, it is that which shall be; and that which is done is that which shall be done; and there is no new thing under the sun" (Ecclesiastes 1:9). This appears to be a fitting description of the concept of PBD.
Author Contributions
Conceptualization, D.M.; Writing-original draft, D.M.; Writing-review and editing, D.M., A.M.H., I.N.E.L., M.K.S., and H.U. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
Given the problems associated with protecting patients' personal data, data confirming the results presented can be obtained from the corresponding author upon any reasonable request.
Acknowledgments
We would like to thank Dr. Daniel Ruslim for providing CAC and CTCA data analysis.
Conflict of Interest
The authors declare no conflict of interest.
References
- Ahmed AH, Shankar K, Eftekhari H, et al. Silent myocardial ischemia: Current perspectives and future directions. Exp Clin Cardiol 12 (2007): 189-196.
- Doenst T, Haverich A, Serruys P, et al. PCI and CABG for Treating Stable Coronary Artery Disease: JACC Review Topic of the Week. J Am Coll Cardiol 73 (2019): 964-976.
- Bergström G, Persson M, Adiels M, et al. Prevalence of Subclinical Coronary Artery Atherosclerosis in the General Population. Circulation 144 (2021): 916-929.
- Laslett LJ, Rubin J, Bringhurst E, et al. Predictive Value of a Negative Exercise Electrocardiogram. In Cardiology 79 (1991): 280-283.
- Zimmermann FM, Pijls NHJ, Gould KL, et al. Stenting "Vulnerable" But Fractional Flow Reserve-Negative Lesions: Potential Statistical Limitations of Ongoing and Future Trials. JACC Cardiovasc Interv 14 (2021): 461-467.
- Expert Panel on Cardiac Imaging; Ghoshhajra BB, Hedgire SS, Hurwitz Koweek LM, et al. ACR Appropriateness Criteria® Asymptomatic Patient at Risk for Coronary Artery Disease: 2021 Update. J Am Coll Radiol 18 (2021): S2-S12.
- Hatzidakis A, Savva E, Perisinakis K, et al. CT coronary angiography in asymptomatic male patients with high atherosclerosis risk: Is it justified? Hellenic J Cardiol 62 (2021): 129-134.
- Graby J, Soto-Hernaez J, Murphy D, et al. Coronary artery calcification on routine CT has prognostic and treatment implications for all ages. Clin Radiol 78 (2023): 412-420.
- Graby J, Khavandi A, Thompson D, et al. CT coronary angiography-guided cardiovascular risk screening in asymptomatic patients: is it time? Clin Radiol 76 (2021): 801-811.
- Makover ME, Shapiro MD, Toth PP. There is urgent need to treat atherosclerotic cardiovascular disease risk earlier, more intensively, and with greater precision: A review of current practice and recommendations for improved effectiveness. Am J Prev Cardiol 12 (2022): 100371.
- Peña-Jorquera H, Cid-Jofré V, Landaeta-Díaz L, et al. Plant-Based Nutrition: Exploring Health Benefits for Atherosclerosis, Chronic Diseases, and Metabolic Syndrome—A Comprehensive Review. Nutrients 15 (2023): 3244.
- Salehin S, Rasmussen P, Mai S, et al. Plant Based Diet and Its Effect on Cardiovascular Disease. Int J Environ Res Public Health 20 (2023): 3337.
- Koutentakis M, Surma S, Rogula S, et al. The Effect of a Vegan Diet on the Cardiovascular System. J Cardiovasc Dev Dis 10 (2023): 94.
- Tucci M, Marino M, Martini D, et al. Plant-Based Foods and Vascular Function: A Systematic Review of Dietary Intervention Trials in Older Subjects and Hypothesized Mechanisms of Action. Nutrients 14 (2022): 2615.
- Islam SU, Ahmed MB, Ahsan H, et al. Recent Molecular Mechanisms and Beneficial Effects of Phytochemicals and Plant-Based Whole Foods in Reducing LDL-C and Preventing Cardiovascular Disease. Antioxidants (Basel) 10 (2021): 784.
- Mehta P, Tawfeeq S, Padte S, et al. Plant-based diet and its effect on coronary artery disease: A narrative review. World J Clin Cases 11 (2023): 4752-4762.
- Bruns A, Greupner T, Nebl J, et al. Plant-based diets and cardiovascular risk factors: a comparison of flexitarians, vegans and omnivores in a cross-sectional study. BMC Nutr 10 (2024): 29.
- Hafiane A. Vulnerable Plaque, Characteristics, Detection, and Potential Therapies. J Cardiovasc Dev Dis 6 (2019): 26.
- Dawson LP, Lum M, Nerleker N, et al. Coronary Atherosclerotic Plaque Regression: JACC State-of-the-Art Review. J Am Coll Cardiol 79 (2022): 66-82.
- Rivera FB, Cha SW, Varona MC, et al. Atherosclerotic coronary plaque regression from lipid-lowering therapies: A meta-analysis and meta-regression. Am J Prev Cardiol 18 (2024): 100645.
- Antithrombotic Trialists' Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 324 (2002): 71-86.
- Virani SS, Newby LK, Arnold SV, et al. Peer Review Committee Members. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients with Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation 148 (2023): e9-e119.
- Babateen AM, Shannon OM, Mathers JC, et al. Validity and reliability of test strips for the measurement of salivary nitrite concentration with and without the use of mouthwash in healthy adults. Nitric Oxide 91 (2019): 15-22.
- Welch AA, Mulligan A, Bingham SA, et al. Urine pH is an indicator of dietary acid-base load, fruit and vegetables and meat intakes: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Norfolk population study. Br J Nutr 99 (2008): 1335-1343.
- Schroeder AP, Falk E. Vulnerable and dangerous coronary plaques. Atherosclerosis 118 (1995): S141-149.
- Moss AJ, Adamson PD, Andrews JP, et al. 9 Vulnerable plaque detection in sudden cardiac death: post-mortem CT coronary angiography 104 (2018): A4.
- Allan S, Pencina M, Thanassoulis G. Clinical reasoning and prevention of cardiovascular disease. J Clin Lipidol 15 (2021): 394-398.
- Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 144 (2021): e368-e454.
- Holland J, Eveson L, Holdsworth D, et al. Coronary artery calcium scoring vs. coronary CT angiography for the assessment of occupationally significant coronary artery disease. J Cardiovasc Comput Tomogr 16 (2022): 454-459.
- Holven KB. Plasma cholesterol levels in infancy: a neglected resource. Eur Heart J 44 (2023): 4419-4421.
- Aygun S, Tokgozoglu L. Comparison of Current International Guidelines for the Management of Dyslipidemia. J Clin Med 11 (2022): 7249.
- Jallinoja P, Absetz P, Kuronen R, et al. The dilemma of patient responsibility for lifestyle change: perceptions among primary care physicians and nurses. Scand J Prim Health Care 25 (2007): 244-249.
- Mogre V, Stevens FCJ, Aryee PA, et al. Why nutrition education is inadequate in the medical curriculum: a qualitative study of students' perspectives on barriers and strategies. BMC Med Educ 18 (2018): 26.
- Bharati R, Kovach KA, Bonnet JP, et al. Incorporating Lifestyle Medicine Into Primary Care Practice: Perceptions and Practices of Family Physicians. Am J Lifestyle Med 17 (2022): 704-716.
- Ornish D, Brown SE, Scherwitz LW, et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet 336 (1990): 129-133.
- Esselstyn CB Jr. Updating a 12-year experience with arrest and reversal therapy for coronary heart disease (an overdue requiem for palliative cardiology). Am J Cardiol 84 (1999): 339-341.
- Gupta SK, Sawhney RC, Rai L, et al. Regression of coronary atherosclerosis through healthy lifestyle in coronary artery disease patients--Mount Abu Open Heart Trial. Indian Heart J 63 (2011): 461-469.
- Reddy KR, Freeman AM, Esselstyn CB. An Urgent Need to Incorporate Evidence-Based Nutrition and Lifestyle Medicine into Medical Training. Am J Lifestyle Med 13 (2018): 40-41.
- Neufingerl N, Eilander A. Nutrient Intake and Status in Adults Consuming Plant-Based Diets Compared to Meat-Eaters: A Systematic Review. Nutrients 14 (2021): 29.
- Jedut P, Glibowski P, Skrzypek M. Comparison of the Health Status of Vegetarians and Omnivores Based on Biochemical Blood Tests, Body Composition Analysis and Quality of Nutrition. Nutrients 15 (2023): 3038.
- Selinger E, Neuenschwander M, Koller A, et al. Evidence of a vegan diet for health benefits and risks - an umbrella review of meta-analyses of observational and clinical studies. Crit Rev Food Sci Nutr 63 (2023): 9926-9936.
- Khanolkar S, Hirani S, Mishra A, et al. Exploring the Role of Vitamin D in Atherosclerosis and Its Impact on Cardiovascular Events: A Comprehensive Review. Cureus 15 (2023): e42470.
- Carbone F, Liberale L, Libby P, et al. Vitamin D in atherosclerosis and cardiovascular events. Eur Heart J 44 (2023): 2078-2094.
- Hariri E, Kassis N, Iskandar JP, et al. Vitamin K2-a neglected player in cardiovascular health: a narrative review. Open Heart 8 (2021): e001715.
- Hasific S, Øvrehus KA, Hosbond S, et al. Effects of vitamins K2 and D3 supplementation in patients with severe coronary artery calcification: a study protocol for a randomised controlled trial. BMJ Open 13 (2023): e073233.
- Blake SR, Heseltine TD, Murray S, et al. A vulnerable plaque identified on CT coronary angiography: when should we act in stable coronary artery disease? BMJ Case Rep (2017).
- Stefanadis C, Antoniou CK, Tsiachris D, et al. Coronary Atherosclerotic Vulnerable Plaque: Current Perspectives. J Am Heart Assoc 6 (2017): e005543.
- Canu M, Broisat A, Riou L, et al. Non-invasive Multimodality Imaging of Coronary Vulnerable Patient. Front Cardiovasc Med 9 (2022): 836473.
- van Veelen A, van der Sangen NMR, Delewi R, et al. Detection of Vulnerable Coronary Plaques Using Invasive and Non-Invasive Imaging Modalities. J Clin Med 11 (2022): 1361.
- Tomaniak M, Katagiri Y, Modolo R, et al. Vulnerable plaques and patients: state-of-the-art. Eur Heart J 41 (2020): 2997-3004.
- Stone GW, Maehara A, Ali ZA, et al. PROSPECT ABSORB Investigators. Percutaneous Coronary Intervention for Vulnerable Coronary Atherosclerotic Plaque. J Am Coll Cardiol 76 (2020): 2289-2301.
- Park SJ, Ahn JM, Kang DY, et al. Preventive percutaneous coronary intervention versus optimal medical therapy alone for the treatment of vulnerable atherosclerotic coronary plaques (PREVENT): a multicentre, open-label, randomized controlled trial (2024): 00413-416.
- van Veelen A, van der Sangen NMR, Henriques JPS, et al. Identification and treatment of the vulnerable coronary plaque. Rev Cardiovasc Med 23 (2022): 39.
- van Veelen A, Küçük IT, Fuentes FH, et al. First-in-Human Drug-Eluting Balloon Treatment of Vulnerable Lipid-Rich Plaques: Rationale and Design of the DEBuT-LRP Study. J Clin Med 12 (2023): 5807.
- Boden WE, O'Rourke RA, Teo KK, et al. COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 356 (2007): 1503-1516.
- Al-Lamee R, Thompson D, Dehbi HM, et al. ORBITA investigators. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomized controlled trial. Lancet 391 (2018): 31-40.
- Maron DJ, Hochman JS, Reynolds HR, et al. ISCHEMIA Research Group. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N Engl J Med 382 (2020): 1395-1407.
- Mulijono D, Plant-Based Diet in Regressing/ Stabilizing Vulnerable Plaques to Achieve Complete Revascularization. Archives of Clinical and Biomedical Research. 8 (2024): 236-244.
- Kurup R, Wijeysundera HC, Bagur R, et al. Complete Versus Incomplete Percutaneous Coronary Intervention-Mediated Revascularization in Patients With Chronic Coronary Syndromes. Cardiovasc Revasc Med 47 (2023): 86-92.
- Garcia S, Sandoval Y, Roukoz H, et al. Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol 62 (2013): 1421-1431.
- Sandoval Y, Brilakis ES, Garcia S. Completeness of revascularization in multivessel coronary artery disease. J Thorac Dis 8 (2016): E1493-E1496.
- Iqbal MB, Moore PT, Nadra IJ, et al. British Columbia Cardiac Registry Investigators. Complete revascularization in stable multivessel coronary artery disease: A real world analysis from the British Columbia Cardiac Registry. Catheter Cardiovasc Interv 99 (2022): 627-638.
- Williams T, Mittal A, Karageorgiev D, et al. e-Ultimaster investigators. Complete revascularization optimizes patient outcomes in multivessel coronary artery disease: Data from the e-Ultimaster registry. Catheter Cardiovasc Interv 99 (2022): 961-967.
- Rose, Stewart D. “A Comprehensive Review of the Prevention and Treatment of Heart Disease with a Plant-Based Diet.” Journal of Cardiology & Cardiovascular Therapy (2018).
- Bilal M, Ashraf S, Zhao X. Dietary Component-Induced Inflammation and Its Amelioration by Prebiotics, Probiotics, and Synbiotics. Front Nutr 9 (2022): 931458.
- Upadhyay S, Dixit M. Role of Polyphenols and Other Phytochemicals on Molecular Signaling. Oxid Med Cell Longev (2015): 504253.
- Wu YT, Chen L, Tan ZB, et al. Luteolin Inhibits Vascular Smooth Muscle Cell Proliferation and Migration by Inhibiting TGFBR1 Signaling. Front Pharmacol 9 (2018): 1059.
- Hong CG, Florida E, Li H, et al. Oxidized low-density lipoprotein associates with cardiovascular disease by a vicious cycle of atherosclerosis and inflammation: A systematic review and meta-analysis. Front Cardiovasc Med 9 (2023): 1023651.
- Marchio P, Guerra-Ojeda S, Vila JM, et al. Targeting Early Atherosclerosis: A Focus on Oxidative Stress and Inflammation. Oxid Med Cell Longev (2019): 8563845.
- Adarsh Ray, Krushna Ch. Maharana, et al. Endothelial dysfunction and its relation in different disorders: Recent update, Health Sciences Review 7 (2023): 100084.
- Monsalve B, Concha-Meyer A, Palomo I, et al. Mechanisms of Endothelial Protection by Natural Bioactive Compounds from Fruit and Vegetables. An Acad Bras Cienc 89 (2017): 615-633.
- Almeida C, Barata P, Fernandes R. The influence of gut microbiota in cardiovascular diseases-a brief review. Porto Biomed J 6 (2021): e106.
- Pollicino F, Veronese N, Dominguez LJ, et al. Mediterranean diet and mitochondria: New findings. Exp Gerontol 176 (2023): 112165.
- Cinegaglia N, Antoniazzi L, Rosa D, et al. Shortening telomere is associated with subclinical atherosclerosis biomarker in omnivorous but not in vegetarian healthy men. Aging (Albany NY) 11 (2019): 5070-5080.




 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
