Prospective Clinical Study of Traumatic Stricture Urethra
Article Information
Dhananjaya Kumar B R1, Shivalingaiah M2, Mayank Jain3*, Pramod Adiga3, Navaneeth Srinidhi R3
1Department of Urology, Institute of Nephrourology, Karnataka, India
2Professor in Urology, Department of Urology, Institute of Nephrourology, Victoria hospital, Karnataka, India
3Assistant Professor, Department of Urology, Institute of Nephrourology, Victoria hospital campus, Karnataka, India
*Corresponding Author: Dr. Mayank Jain Assistant Professor, Department of Urology, Institute of Nephrourology, Victoria hospital campus, K R Market, Bengaluru, Karnataka-560002, India
Received: 21 April 2020; Accepted: 20 May 2020; Published: 14 July 2020
Citation: Dhananjaya Kumar B R, Shivalingaiah M, Mayank Jain, Pramod Adiga, Navaneeth Srinidhi R. Prospective Clinical Study of Traumatic Stricture Urethra. Archives of Nephrology and Urology 3 (2020): 049-060.
View / Download Pdf Share at FacebookAbstract
Introduction: Traumatic stricture urethra is a rare entity, with surgery being the only treatment modality. We aim to evaluate and analyse the surgical outcomes and erectile function in patients who undergo surgical treatment for traumatic urethral stricture disease at our institution.
Material and Methods: A prospective study was conducted on 57 male patients who presented between Aug 2015 and Dec 2017 in our institution, with post traumatic stricture urethra. The urethral rupture was confirmed by RGU and patients underwent suprapubic catheterisation initially. At 3 months these patients underwent delayed anastomotic urethroplasty. The patients were followed up for 6 months- 24 months. Erectile function was assessed by IIEF-5 questionnaire pre operatively and post-operatively at 6 months.
Results: Mean age of patients was 38.5 years. Majority of the patients (36.84%) were between 21 to 30 years of age..Majority of the patients (32) had road traffic accidents (indirect) and 12 patients had history of fall/direct trauma to perineum or urethra. Twelve (21.05%) patients developed complications postoperatively. Early complications of wound infection occurred in 08 (14.03%) patients. Late complications were seen in 12 (21%) patients i.e. restenosis. Erectile dysfunction is seen in 42.11% patients at the end of six months. Overall surgical success rate was 78.9 % at 6 months.
Conclusion: Delayed anastomotic urethroplasty is an effective procedure for traumatic urethral strictures with good surgical results. Recurrence of stricture is most common complication. But, surgical procedure leads to some degree of erectile function.
Keywords
Post-traumatic stricture; Posterior urethra; Anastomotic urethroplasty; Erectile dysfunction
Post-traumatic stricture articles, Posterior urethra articles, Anastomotic urethroplasty articles, Erectile dysfunction articles
Post-traumatic stricture articles Post-traumatic stricture Research articles Post-traumatic stricture review articles Post-traumatic stricture PubMed articles Post-traumatic stricture PubMed Central articles Post-traumatic stricture 2023 articles Post-traumatic stricture 2024 articles Post-traumatic stricture Scopus articles Post-traumatic stricture impact factor journals Post-traumatic stricture Scopus journals Post-traumatic stricture PubMed journals Post-traumatic stricture medical journals Post-traumatic stricture free journals Post-traumatic stricture best journals Post-traumatic stricture top journals Post-traumatic stricture free medical journals Post-traumatic stricture famous journals Post-traumatic stricture Google Scholar indexed journals Posterior urethra articles Posterior urethra Research articles Posterior urethra review articles Posterior urethra PubMed articles Posterior urethra PubMed Central articles Posterior urethra 2023 articles Posterior urethra 2024 articles Posterior urethra Scopus articles Posterior urethra impact factor journals Posterior urethra Scopus journals Posterior urethra PubMed journals Posterior urethra medical journals Posterior urethra free journals Posterior urethra best journals Posterior urethra top journals Posterior urethra free medical journals Posterior urethra famous journals Posterior urethra Google Scholar indexed journals Anastomotic urethroplasty articles Anastomotic urethroplasty Research articles Anastomotic urethroplasty review articles Anastomotic urethroplasty PubMed articles Anastomotic urethroplasty PubMed Central articles Anastomotic urethroplasty 2023 articles Anastomotic urethroplasty 2024 articles Anastomotic urethroplasty Scopus articles Anastomotic urethroplasty impact factor journals Anastomotic urethroplasty Scopus journals Anastomotic urethroplasty PubMed journals Anastomotic urethroplasty medical journals Anastomotic urethroplasty free journals Anastomotic urethroplasty best journals Anastomotic urethroplasty top journals Anastomotic urethroplasty free medical journals Anastomotic urethroplasty famous journals Anastomotic urethroplasty Google Scholar indexed journals Erectile dysfunction articles Erectile dysfunction Research articles Erectile dysfunction review articles Erectile dysfunction PubMed articles Erectile dysfunction PubMed Central articles Erectile dysfunction 2023 articles Erectile dysfunction 2024 articles Erectile dysfunction Scopus articles Erectile dysfunction impact factor journals Erectile dysfunction Scopus journals Erectile dysfunction PubMed journals Erectile dysfunction medical journals Erectile dysfunction free journals Erectile dysfunction best journals Erectile dysfunction top journals Erectile dysfunction free medical journals Erectile dysfunction famous journals Erectile dysfunction Google Scholar indexed journals Suprabupic Catherisation articles Suprabupic Catherisation Research articles Suprabupic Catherisation review articles Suprabupic Catherisation PubMed articles Suprabupic Catherisation PubMed Central articles Suprabupic Catherisation 2023 articles Suprabupic Catherisation 2024 articles Suprabupic Catherisation Scopus articles Suprabupic Catherisation impact factor journals Suprabupic Catherisation Scopus journals Suprabupic Catherisation PubMed journals Suprabupic Catherisation medical journals Suprabupic Catherisation free journals Suprabupic Catherisation best journals Suprabupic Catherisation top journals Suprabupic Catherisation free medical journals Suprabupic Catherisation famous journals Suprabupic Catherisation Google Scholar indexed journals dialysis articles dialysis Research articles dialysis review articles dialysis PubMed articles dialysis PubMed Central articles dialysis 2023 articles dialysis 2024 articles dialysis Scopus articles dialysis impact factor journals dialysis Scopus journals dialysis PubMed journals dialysis medical journals dialysis free journals dialysis best journals dialysis top journals dialysis free medical journals dialysis famous journals dialysis Google Scholar indexed journals
Article Details
1. Introduction
Trauma has a predilection for young adults and results in the loss of more productive work years than cancer and heart disease combined [1]. The urogenital system has consistently been shown to be involved in 10% of patients presenting after trauma and is therefore a significant factor in trauma-induced morbidity and mortality [2]. 4% of genitourinary trauma accounts for urethral injuries, but have the propensity to incur substantial long term morbidity including intractable stricture disease, incontinence, impotence, and infertility [3, 4]. When the urethra is injured, 65% are complete disruptions with the remaining 35% resulting in partial tears [5]. Men are approximately 5 times more likely to have a urethral injury than women, which is attributed to the longer length and reduced mobility of the male urethra [6, 7]. Posterior urethral injuries associated with pelvic fractures are the most common non iatrogenic urethral injury in industrialized societies and are approximately 4 times more common than anterior urethral injuries [8]. The posterior urethra is initially stretched and then partially or completely disrupted at the bulbomembranous junction [9]. S traddle fracture and sacroiliac joint diastasis accounts for 24 times higher risk of urethral injury [10]. Most of the patients had specific inferomedial pubic bone fractures or pubic symphysis diastasis, with > 1cm displacement seen in 88% of these patients. In anterior urethral injuries blunt injury to the anterior urethra occurs approximately one-quarter as often as posterior injury and is generally a -straddle type? injury of the bulbar urethra [11]. Slightly less commonly, the anterior urethra is injured during a fracture of the penis or gunshot wound [12, 13, 14].
2. Materials and Methods
The study was conducted to analyse the outcome in patients who underwent surgical treatment for traumatic urethral stricture disease at our institution including mode, degree of urethral injury, associated types and pattern of pelvic injury, surgical techniques/ approach, outcomes in terms of voiding pattern and sexual health and failure rates. This prospective study included 57 male patients who presented between Aug 2015 and Dec 2017 at our institution, with post traumatic stricture urethra. Only patients with normal erectile function ,before trauma were included in study. Patients in paediatric age group, inflammatory urethral stricture, iatrogenic stricture urethra, recurrent stricture, associated bladder/bladder neck injuries and patients not willing for strict follow up were excluded from the study. Informed written consent was obtained from all the patients. Institutional ethical review board committee approval was taken with id= INU/RRC/01/2016-17. All patients were followed up to minimum 6 months after injury, and follow up period ranged from 3 months to 2 years. Patients with suspected urethral injury who presented to casualty were carefully assessed, haemodynamically stabilized and subsequently evaluated with detailed history for mode of injury, associated solid organ injury, presence of blood at meatus, acute urinary retention, associated pelvic fracture – including type, stability and need of intervention. Incremental Retrograde Urethrogram(RGU) was done in all cases and urethral injury was graded. Only for Grade I injury gentle catheterisation attempted; if failed SPC was done. Other than Grade I injury, diversion is done by Suprabupic Catherisation (SPC). (Grade IV injury is not included in the study).{McCullum Colapinto Classfication}
2.1 Three-Month delay
We wait 3 months from the time of injury before performing urethroplasty to allow time for the initial extravasations to heal, hematoma to resolve, and the extent of the injury to become clearly defined and to provide “urethral rest”.
2.2 Preoperative urethral imaging and cystoscopy
As preoperative workup, urethroscopy, ante-grade cystoscopy, and simultaneous Micturating Cystourethrogram (MCU) and RGU were done, that depicts the exact length and location of the defect, using standard techniques. Distraction defect/Stricture length was calcutaed from RGU and MCU. Patients were also assessed about the erectile function. Patients were evaluated by using validated questionnaires, International Index of Erectile Function-5 (IIEF-5) preoperatively and six months after surgical repair.
2.3 Posterior urethral reconstruction
A mandatory sterile urine culture was done before surgery. Our protocol was to administer cephalosporin and Amikacin,
but we adjust the antibiotics if indicated based on the culture
result.
2.4 Surgical technique
A midline perineal incision, made along the line of the raphe, from scrotal margin to anal margin. Standard surgical steps were followed for bulbar urethral mobilisation. Bulbar urethra is freed from penobulbar junction till membranous urethra. For pelvic fracture urethral injuries bulbar arteries were ligated, which can be preserved in bulbar urethral trauma. The urethra is then transected through the site of obliteration, trimmed back to healthy tissue on either side, spatulated dorsally on one side and ventrally on the other. Healthy tissue was identified by a healthy looking epithelium and a granular appearance of the spongiosum with no plaques of scar tissue on either side. In an uncomplicated situation- Six to eight 4/0 polyglactin absorbable sutures are placed around the circumference of the repair with a spatulated anastomosis. In each suture full thickness of the dorsal aspect of the distal urethra, is taken with tunica albuginea at the site where the anastomosis rests, with full thickness of the distal aspect of the proximal urethra, and hence knots lying inside of the urethra. For more proximal bulbar anastomosis, all eight sutures are placed, clipping the two ends one by one, and retracting them out of the way ‘parachute style’, and then tying them all, one after the other, at the end.

Figure 1: Xray pelvis - showing fracture of both superior and inferior pubic rami.

Figure 2: RGU showing abrupt cut off.
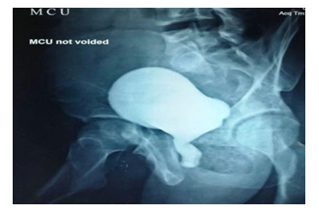
Figure 3: MCU- showing dilated posterior urethra.
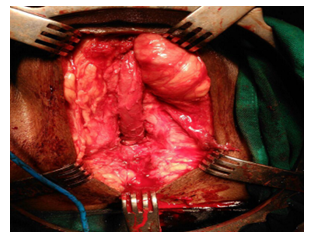
Figure 4: Intraoperative picture of ananstomotic urethroplasty- Foleys catheter passed in proximal and distal urethra after excision of stricturous part.
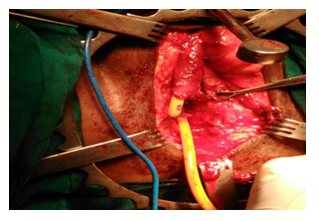
Figure 5: After successful completion of end to end anastomosis.
2.4.1 In more complicated cases: Where there has been a more significant loss of length, three sequential manoveres were performed as per the need i.e corporeal separation, inferior Pubectomy and urethral rerouting were performed. If inferior wedge pubectomy is performed, the two crura then need to be retracted laterally off the pubic symphysis ligating and dividing the deep dorsal vein of the penis. The dorsal arteries and nerves to be identified, retracted and therefore preserved. Post procedure, a 16 F silicone Foley urethral catheter was placed and if a wedge pubectomy has been used, a small drain is left in the cavity, which was removed after 48 hours. The patient is usually allowed orally and mobilized by next day. Per-urethral catheter is left for a minimum period of 3 weeks. A peri-catheter urethrogram is performed after 3 weeks to ensure that there is healing of the anastomosis. Catheter free trail void was given if there is no leakage on RGU.
2.5 Success was defined as
- Patient voids well with adequate calibre as before trauma.
- Continence and adequate urethra at the site of repair.
- Secondary or auxiliary procedures needed.
- No restenosis.
2.6 Failure was defined as
- Not voiding as before catheter removal.
- Narrowing or arrest of contrast medium at the site of repair on urethrography.
- The need for repeat dilatation or repeat DVIU.
3. Results
Mean age was 38.35 yrs with maximum numbers of patients are from age 21-30 yrs. Age ranged from 16-72 years (Table 1). With refrence to mode of Injury more than half of patients were secondary to RTA (Table 2). Only 4 patients required immediate exploration. Out of which 2 patients had associated bowel injury that underwent colostomy. One patient had bladder perforation with urethral injury and one patient was explored for haemoperitoneum. In rest 93% of patients urethral injury was managed conservatively by placing SPC. In our study we found that maximum 30 (52.63%) patients had Grade III urethral injury that accounts for nearly 52.63%, followed by 16 Grade V (28.07%) injuries. 8.7% (5) patients had Grade II and Grade I urethral injuries. 6 patients required orthopaedic intervention for unstable pelvic fracture prior to urethroplasty. 70% (40) patients had stable fractures while 11 patients did not sustained associated pelvic fracture. Patients with unsatable fractures were first stabilised with fixators by orthopedecian and once cleared by orthopedecian were taken up for surgery. Rest other patients were managed conservatively. After putting SPC initially stricture length was assessed using RGU. 2-3 cm was most common length of defect with stricture length ranging from 0.5 cm to 8 cm.
Meawhile bulbomembranous junction was the most common site of stricture i.e 29 patients, followed by bulbobulbar (19) and lastly 9 patients had high up urethral trauma site at bulbo-prostatic junction.Only bulbar urethral mobilisation(simple perineal anastomosis) was sufficient in 23(40.35%) patients; while rest of the patients needed elaborated perineal approach.Out of which 17(29.82%) patients needed crural separation, 14 (24.56%) needed inferior pubectomy and 5 patients needed urethral rerouting for tension free anastomosis. In our study post-operative complications were seen only in 12 patients (21.05%). All were managed conservatively except for one patient. One patient on first post-op day, had pulled out his PUC accidentally, for which he required cystoscopic assisted per urethral Catherisation.
Surgical site infection was most common complication seen in 8 (14%) patients, 2 had fever, 1 had hematoma at operative site. Pericatheter RGU was done at 3-4 weeks if urine culture is sterile and patient is asymptomatic. 53 patients had no leak and were subjected to trial void. Patients with contrast extravasation were advised to keep per urethral catheter for additional 1 week, followed by catheter removal. After catheter removal uroflowmetry was done to know the Qmax. Qmax was assessed at 1 month and 3months after surgery. Qmax of > 15ml was seen in all patients At six months post urethroplasty, 2 patients required cystoscopic dilatation and 1 patient under went VIU. On follow up between 6 to 12 months after surgery, 5 patients underwent VIU and 4 patients required cystoscopic dilatation, thus in our study the overall success rate at the end of one year 78.94%. Out of 57 patients,31(54.38%) patients had erectile dysfunction pre-operatively. In that majority of the patients had Mild ED (15 patients), 8 patients had Mild-Moderate ED, and 2 patients had severe ED and 6 patients had moderate ED. Patients were subjected to IIEF-5 questionnaire 6 months after successful surgical repair and erectile function was reassessed. In our study we found to that there is no significant improvement in sexual function i.e., 57.89 % of patients. Maximum number of patients had mild ED (12 patients), 6 patients had Mild-moderate ED and 5 patients had moderate ED 1 patient had severe ED. overall 42.11% (24 patients) had ED at the end of six months after surgical repair. We followed up patients from 3 months to 2½ years. (Table 3). Wilcoxon sign rank test was done to compare the pre-operative and post-operative IIEF-5 scoring and we found P value is not significant i.e., 0.0577 Wilcoxon sign rank test was done to compare pre & post-op IIEF scorings for ED (Table 4).
|
Age Group (Years) |
No.of Patients |
Percentage (%) |
|
16-20 |
4 |
7.01% |
|
21-30 |
21 |
36.84 % |
|
31-40 |
9 |
15.78 % |
|
41-50 |
8 |
14.03 % |
|
51-60 |
9 |
15.78 % |
|
61-70 |
4 |
7.01 % |
|
>70 |
2 |
3.5 % |
Table 1: Number of Patients distributed in different age groups.
|
Mode Of Injury |
No.of Patients |
Percentage (%) |
|
Pulled Out Catheter |
2 |
3.5 % |
|
Penetrating Injury |
3 |
5.26 % |
|
Fall From Height |
8 |
14.03% |
|
Straddle Injury |
12 |
21.05 5 |
|
Road Traffic Accidents (Rta) |
32 |
56.14 % |
|
Total |
57 |
100 % |
Table 2: Mode of injury.
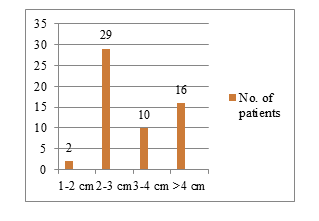
Figure 6: Urethral defect length.
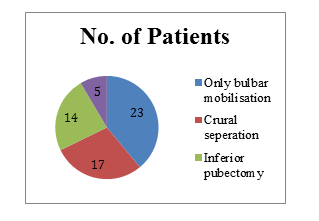
Figure 7: Additional manoveres.
|
Grade of Erectile Function |
Preoperative Ed |
Post Operative Ed (At 6 Months) |
||
|
No. of Patients |
Percentage |
No. of Patients |
Percentage |
|
|
Mild |
15 |
26.31 % |
12 |
21.05 % |
|
Mild- Moderate |
8 |
14.03 % |
6 |
11 % |
|
Moderate |
6 |
10.52 % |
5 |
9 % |
|
Severe |
2 |
3.5 % |
1 |
1.75 % |
|
NO |
26 |
45.61 % |
33 |
57.89 % |
|
100 % |
100 % |
|||
Table 3: Grades of Erectile function Pre and Post operatively.
|
Mean (SD) |
P-Value |
|
|
Preop ED |
18.31(4.81) |
0.0577 |
|
Post op ED |
19.92 (4.13) |
Table 4: Wilcoxon sign rank comparing pre and post op ED.
4. Discussion
Posterior urethral disruption is one of most demanding urological injuries to manage following pelvic trauma .Early intervention may be complicated by bleeding, huge pelvic hematoma, concomitant injuries to other organs. Suprapubic cystostomy, with delayed anastomotic perineal anastomotic urethroplasty remains the gold standard with long term success rates exceeding 90%. But other modality like primary endoscopic re-alignment of urethra can reduce the need for further more complicated intervention. Adequate mobilization and tension-free spatulated urethral anastomosis is the key to success. Ideal stricture length for simple end-to-end anastomosis urethroplasty should be less than 2 cm.For longer defects in which resection and anastomosis are not possible, substitution techniques by grafts or flaps (substitution urethroplasty) are used. Various sequential maneuvers are applied, for the adequate mobilization of the urethra (progressive perineal Urethroplasty technique) to achieve a successful tension free repair. Mean age in our study was 38.35 years. Our study confirms the finding of by Barbagli et al, that patient age is not a factor in the success of procedure higher age is not a contraindication for anastomotic urethroplasty [15]. In our present study most of the patients had RTA (motor vehicle collision), that is 32 patients (56.14%). In a study conducted by Barbagli et al. [16], he has stated that PFUDD is due to prevalent agricultural activity, accidents on work site followed by bicycles and motor vehicle collisions. In a retrospective observational study conducted by Fu Qiang et al. [17] he has found that most of the patients 58.24% had motor vehicle collision followed by straddle injuries 22.34% as a etiology for PFUDD, which is comparable to our present study. Optimal timing (immediate vs. delayed) and surgical approach (endoscopic vs. open) of PFUDD remain controversial. Immediate repair was advisable in patients with concomitant bladder injury, severe prostatomembranous dislocation or rectal injury [18]. But in our study all the subjects were managed initially with SPC followed by urethroplasty at 3 months. In a systematic review analysis study conducted by Elshout PJ et al. [19]. Outcomes of Early endoscopic realignment (EER) versus suprapubic Cystostomy and delayed anastomotic urethroplasty for pelvic fracture urethral injuries. Author concluded that EER has poor success rates, poor functional outcomes and there is need of auxiliary procedures in EER when compared to Delayed urethroplasty. In our study delayed anastomotic urethroplasty was performed without previous urethral manipulation or surgery, as in a study conducted by Culty T et al [20].
In primary case the success rate of anastomotic urethroplasty is about 90-95 % [21], but in a prospective study conducted by Koraitim MM et al. [22], success rate is about 88% while in study conducted by Flynn BJ et al. [23] it was 95%. In a prospective study conducted by Odoemene CA et al. [24] on 87 patients showed success rate 86.21%. A retrospective study in 172 patients at Sharma university of health sciences, Rohtak by Singh et al showed overall success rate of about 91.28%. He had success rate of 93.4% for simple anastomotic urethroplasty, 90.4% for perineal anastomosis with separation of corporal bodies, 88% with inferior pubectomy and 66.7% with corporal rerouting of urethra [21]. In our clinical prospective study, 57 patients were included during study period. All patients underwent Delayed anastomotic urethroplasty. Mean stricturelength is about 2.76cm with a follow up period ranged from 1 month to 30 months. In our study we had overall success rate of 78.94% at the end of one year. In a prospective study conducted by Gupta et al [25] on 138 patients underwent anastomotic urethroplasty, mean age was 28.1 years (range 6-71) and mean stricture length was 2.2 cm (range 0.7-6.0). Average follow-up was 26.7 months (range 6-60). 114 (82.6%) had excellent outcome. Seventeen patients developed complications: 5had wound infection, 3 had epididymorchitis, 2 had failure to void, 2 each had incontinence and perineal hematoma, and on patient had accidentally pulled his catheter out and had urethrocutaneous fistula. In our prospective study out of 57 patients, 8 (14.03%) patients had wound infection, 2 patients had UTI, 1 patient had perineal haematoma on POD-1 which was managed conservatively. One patient had pulled out his catheter for which he required cystoscopic catherisation under anaesthesia. Similarly in a study conducted by Esteban-María et al. [21], reported wound infection in 4.0%. Urethrocutaneous fistula observed in different studies ranged from 02-15% [26]. In our study the incidence of urethrocutaneous fistula is 0%. In our study, the incidence of recurrent stricture was 21.05%. In a study conducted by Dakum et al. [26] reported its incidence 34.4%. Similarly study conducted by Mundy et al. [27] and Tijani et al. [28] showed recurrent stricture rate is 12% and 22.5% respectively. In our study during the follow up of 1 month, 3 months and 6months, no incidence of incontinence was found as patients with bladder neck injury were not included in the study. In a systemic review and meta-analysis by Blaschko SD et al [29], in de novo ED after PFUI, in their study fourteen studies (total 815patients) included information on ED after PFUI. These studies assessed patients who later underwent delayed anastomotic urethroplasty . The pooled estimate of the proportion (95% CI) of patients with ED after PFUI but before delayed urethroplasty was 34 (25–45) %, with ED ranging from of 0–100% in these studies. In our study we found to have higher percentage of ED after PFUI i.e. around 54.38 %, thus we have found higher incidence of ED compared to the mentioned studies. It can be attributed to lack of confidence to attempt sexual intercourse or to initiate in sexual act as patients are hindered by their co-morbidities. The proportion of patients with de novo ED after delayed urethroplasty was 3 (2–5) %, with a range of de novo ED after delayed urethroplasty of 0–34%. In study conducted by El-Assmy A et al. [30], 81 patients were included. The incidences of ED following urethroplasty for traumatic urethral injury were 72.3, 35.3 and 0% in cases due to pelvic fracture, straddle and iatrogenic injuries, respectively with no deterioration of erectile function (EF) after urethroplasty. Seven (13.5%) patients reported recovery of their EF within 2 years after trauma. The probability of recovery of EF after PFUI was 9 % compared to 28.6 and 100 % in patients with straddle and iatrogenic urethral injuries, respectively. Patients with type C pelvic fracture had no chance for EF recovery (Table 5). In our study out of 57 patients, 54.38% of patients had erectile dysfunction after traumatic urethral injury (pre-operatively). All the patients were evaluated for sexual function outcomes at the end of six months after surgical repair by IIEF-5 scoring system. In our study 42.10% of patients had erectile dysfunction. Out of which 1 patient (1.75%) had severe ED and majority of the patients had mild ED (21.05%). In our study we have seen improvement in erectile function after urethroplasty only in few patients. However long term follow-up is required to assess the outcomes of erecticle dysfunction.
|
Parameter |
Lumen et al |
Bhandari et al |
Fu Q et al |
Singh et al |
Present Study |
|
Study Design |
Prospective |
Retrospective |
Retrospective |
Retrospective |
Prospective |
|
No of patients |
21 |
50 |
573 |
172 |
57 |
|
Mean Age (years) |
48 |
35 |
36 |
34 |
38.35 |
|
Stricture length (cm) |
4.2 |
2.2 |
2.18 |
3.4 |
2.76 |
|
Time to Surgery (months) |
4.5 |
6 |
6-24 |
5.5 |
6.12 |
|
Complications (%) |
3 |
8 |
9.2 |
21 |
|
|
Success Rate (%) |
84 |
80 |
86.2 |
84.62 |
78.94 |
Table 5: Comparision with other Studies.
5. Conclusion
Road traffic accidents are the major cause of pelvic fracture urethral distraction, significantly affects younger population. Perineal anastomotic urethroplasty is the gold standard technique. There are no significant complications associated with progressive perineal urethroplasty. Location of distraction defects, length of the defect, and amount of fibrosis and presence of callous in between the distracted ends of urethra are the factors that determine the selection of the surgical procedure. Recurrence of stricture is most common complication. Anastomotic Urethroplasty can lead to erectile dysfunction and improvement in erectile function after surgical repair is less likely.
References
- Bonnie RJ, Fulco CE, Liverman CT. Institute of Medicine (US) Committee on Injury Prevention and Control, Reducing the Burden of Injury: Advancing Prevention and Treatment. Washington (DC): National Academies Press (US) (1999).
- Shewakramani S, Reed KC. Genitourinary trauma. Emerg Med Clin North Am 29 (2011): 501-518.
- Bariol SV, Stewart GD, Smith RD, et al. An analysis of urinary tract trauma in Scotland: impact on management and resource needs. Surgeon 3 (2005): 27-30.
- Mundy AR. Pelvic fracture injuries of the posterior urethra. World J Urol 17 (1999): 90-95.
- Webster GD, Mathes GL, Selli C. Prostatomembranous urethral injuries: a review of the literature and a rational approach to their management. J Urol 130 (1983): 898-902.
- Lowe MA, Mason JT, Luna GK, et al. Risk factors for urethral injuries in men with traumatic pelvic fractures. J Urol 140 (1988): 506-507.
- Carter CT, Schafer N. Incidence of urethral disruption in females with traumatic pelvic fractures. Am J Emerg Med 11 (1993): 218-220.
- Mundy AR, Andrich DE. Urethral trauma. Part I: introduction, history, anatomy, pathology, assessment and emergency management. BJU Int 108 (2011): 310-327.
- Koraitim MM. Pelvic fracture urethral injuries: the unresolved controversy. J Urol 161 (1999): 1433-1441.
- Koraitim MM, Marzouk ME, Atta MA, et al. Risk factors and mechanism of urethral injury in pelvic fractures. Br J Urol 77 (1996): 876-880.
- Chapple C, Barbagli G, Jordan G, et al. Consensus statement on urethral trauma. BJU Int 93 (2004): 1195-1202.
- Cendron M, Whitmore KE, Carpiniello V, et al. Traumatic rupture of the corpus cavernosum: evaluation and management. The Journal of Urology 144 (1990): 987-991.
- Sant GR. Rupture of the corpus cavernosum of the penis. Arch Surg 116 (1981): 1176-1178.
- Lynch TH, Martínez-Piñeiro L, Plas E, et al. EAU guidelines on urological trauma. Eur Urol 47 (2005): 1-15.
- Udekwu PO, Gurkin B, Oller DW. The use of compu-ted tomography in blunt abdominal injuries. Am Surg 62 (1996): 56-59.
- Gopalakrishnan G. Re: Guido Barbagli. History and evolution of transpubic urethroplasty: a lesson for young urologists in training. Eur urol 52 (2007): 1290-1292.
- Fu Q, Zhang J, Sa YL, et al. Recurrence and complications after transperineal bulboprostatic anastomosis for posterior urethral strictures resulting from pelvic fracture: a retrospective study from a urethral referral centre. BJU Int 112 (2013): E358-E363.
- Singh SK, Pawar DS, Khandelwal AK, et al. Transperineal bulboprostatic anastomotic repair of pelvic fracture urethral distraction defect and role of ancillary maneuver: A retrospective study in 172 patients. Urol Ann 2 (2010): 53-57.
- Elshout PJ, Veskimae E, MacLennan S, et al. Outcomes of Early Endoscopic Realignment Versus Suprapubic Cystostomy and Delayed Urethroplasty for Pelvic Fracture-related Posterior Urethral Injuries: A Systematic Review. Eur Urol Focus 3 (2017): 545-553.
- Culty T, Boccon-Gibod L. Anastomotic urethroplasty for posttraumatic urethral stricture: previous urethral manipulation has a negative impact on the final outcome. The Journal of Urology 177 (2007): 1374-1377.
- Esteban-María J, Mendoza-Lucio L. Urethroplasty as urethral stricture treatment at the Hospital Universitario Dr. José Eleuterio González; Monterrey, Nuevo León, Mexico. Rev Mex Urol 70 (2010): 79-83.
- Koraitim MM, Kamel MI. Perineal repair of pelvic fracture urethral injury: in pursuit of a successful outcome. BJU Int 116 (2015): 265-270.
- Flynn BJ, Delvecchio FC, Webster GD. Perineal repair of pelvic fracture urethral distraction defects: experience in 120 patients during the last 10 years. J Urol 170 (2003): 1877-1880.
- Odoemene CA, Okere P. One-stage Anastomotic Urethroplasty for Traumatic Urethral Strictures. January 2004-January 2013. Niger J Surg 21 (2015): 124-129.
- Gupta NP, Mishra S, Dogra PN, et al. Outcome of end-to-end urethroplasty: single-center experience. Urol Int 82 (2009): 179-182.
- Dakum NK, Ramyil VM, Amu CO. Outcome of urethroplasty for urethral stricture at Jos Universitry Teaching Hospital. Niger J Clin Pract 11 (2008): 300-304.
- Mundy AR. Urethroplasty for posterior urethral strictures. Br J Urol 78 (1996): 243-247.
- Tijani KH, Ogo CN, Adeyomoye A. Excision and end-to-end anastomotic urethroplasty in the management of post-traumatic urethral stricture disease: experience and challenges in a Nigerian teaching hospital. Niger Postgrad Med J 17 (2010): 185-189.
- Blaschko SD, Sanford MT, Schlomer BJ, et al. Villalta et al. The incidence of erectile dysfunction after pelvic fracture urethral injury: A systematic review and meta-analysis. Arab J Urol 13 (2015): 68-74.
- El-Assmy A, Harraz AM, Benhassan M, et al. Erectile dysfunction post-perineal anastomotic urethroplasty for traumatic urethral injuries: analysis of incidence and possibility of recovery. Int Urol Nephrol 47 (2015): 797-802.


 Impact Factor: * 2.3
Impact Factor: * 2.3 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 