Rare Coexisting Pyloric Stenosis, Oesophageal Peptic Stricture and Hiatal Hernia
Article Information
Sarah BENAMMI MD*, Youness BAKALI MD, Mouna ALAOUI MD, PhD, Farid SABBAH MD, PhD, Mohamed RAISS MD, PhD, Abdelmalek HRORA MD PhD
Surgical Department “C” Ibn Sina University Hospital, University Mohamed V, Rabat, Morocco
*Corresponding Author: Dr. Sarah Benammi MD, Surgical Department “C” Ibn Sina University Hospital, University Mohamed V, Rabat, Morocco
Received: 05 May 2020; Accepted: 02 June 2020; Published: 08 July 2020
Citation: Sarah BENAMMI, Youness BAKALI, Mouna ALAOUI, Farid SABBAH, Mohamed RAISS, Abdelmalek HRORA. Rare Coexisting Pyloric Stenosis, Oesophageal Peptic Stricture and Hiatal Hernia. Archives of Clinical and Medical Case Reports 4 (2020): 633-637.
View / Download Pdf Share at FacebookAbstract
Introduction: Our purpose is to report the clinical presentation of a rare coexistence of pyloric stenosis, peptic esophageal stricture associated with hiatal hernia, and discuss the therapeutic strategy decided with criterion of decision-making and outcome.
Presentation of Case: We experienced a case of 67-year-old man with history of duodenal ulcer presenting a co-existing pyloric stenosis, peptic esophageal stricture and hiatal hernia. Clinical presentation consisted of an evolving gastrooesophageal reflux disease GERD symptoms along with gastric discomfort. Further exploration characterized a benign stricture between middle and lower esophagus with sliding hiatal hernia, a stasis stomach attaining pelvic area, and a second post-bulbar stenosis with double bubble aspect. The therapeutic strategy decided was medical preparation with subsequent endoscopic esophageal dilatation, followed by a Roux-en-Y diversion with antrectomy surgery and bilateral vagotomy. Evolution was uneventful.
Conclusion: To our knowledge we report the first case of duodenal ulcer with pyloric stenosis associated with esophageal peptic stenosis and hiatal hernia reviewed in literature. The condition can be arguably considered as a complication of gastric emptying delay due to pyloric stenosis, and triggered by the duodenal ulcer disease in addition to hiatal hernia. Association of endoscopic dilation and Roux-Y gastrojejunostomy diversion after antrectomy and bivagotomy in our case meets all the requirements. Indeed the approach enables further exploration of the stomach comforting the histological diagnosis of benign strictures, treat the surgical stricture, reduce volume of toneless dilated stomach, and treat GERD. Nissen fundoplication is not indicated.
Keywords
Pyloric stenosis; Oesophageal Peptic Stricture; Hiatal Hernia; GERD; Roux-Y gastrojejunostomy
Pyloric stenosis articles, Oesophageal Peptic Stricture articles, Hiatal Hernia articles, GERD articles, Roux-Y gastrojejunostomy articles
Pyloric stenosis articles Pyloric stenosis Research articles Pyloric stenosis review articles Pyloric stenosis PubMed articles Pyloric stenosis PubMed Central articles Pyloric stenosis 2023 articles Pyloric stenosis 2024 articles Pyloric stenosis Scopus articles Pyloric stenosis impact factor journals Pyloric stenosis Scopus journals Pyloric stenosis PubMed journals Pyloric stenosis medical journals Pyloric stenosis free journals Pyloric stenosis best journals Pyloric stenosis top journals Pyloric stenosis free medical journals Pyloric stenosis famous journals Pyloric stenosis Google Scholar indexed journals stenosis articles stenosis Research articles stenosis review articles stenosis PubMed articles stenosis PubMed Central articles stenosis 2023 articles stenosis 2024 articles stenosis Scopus articles stenosis impact factor journals stenosis Scopus journals stenosis PubMed journals stenosis medical journals stenosis free journals stenosis best journals stenosis top journals stenosis free medical journals stenosis famous journals stenosis Google Scholar indexed journals Oesophageal Peptic Stricture articles Oesophageal Peptic Stricture Research articles Oesophageal Peptic Stricture review articles Oesophageal Peptic Stricture PubMed articles Oesophageal Peptic Stricture PubMed Central articles Oesophageal Peptic Stricture 2023 articles Oesophageal Peptic Stricture 2024 articles Oesophageal Peptic Stricture Scopus articles Oesophageal Peptic Stricture impact factor journals Oesophageal Peptic Stricture Scopus journals Oesophageal Peptic Stricture PubMed journals Oesophageal Peptic Stricture medical journals Oesophageal Peptic Stricture free journals Oesophageal Peptic Stricture best journals Oesophageal Peptic Stricture top journals Oesophageal Peptic Stricture free medical journals Oesophageal Peptic Stricture famous journals Oesophageal Peptic Stricture Google Scholar indexed journals Hiatal Hernia articles Hiatal Hernia Research articles Hiatal Hernia review articles Hiatal Hernia PubMed articles Hiatal Hernia PubMed Central articles Hiatal Hernia 2023 articles Hiatal Hernia 2024 articles Hiatal Hernia Scopus articles Hiatal Hernia impact factor journals Hiatal Hernia Scopus journals Hiatal Hernia PubMed journals Hiatal Hernia medical journals Hiatal Hernia free journals Hiatal Hernia best journals Hiatal Hernia top journals Hiatal Hernia free medical journals Hiatal Hernia famous journals Hiatal Hernia Google Scholar indexed journals GERD articles GERD Research articles GERD review articles GERD PubMed articles GERD PubMed Central articles GERD 2023 articles GERD 2024 articles GERD Scopus articles GERD impact factor journals GERD Scopus journals GERD PubMed journals GERD medical journals GERD free journals GERD best journals GERD top journals GERD free medical journals GERD famous journals GERD Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Roux-Y gastrojejunostomy articles Roux-Y gastrojejunostomy Research articles Roux-Y gastrojejunostomy review articles Roux-Y gastrojejunostomy PubMed articles Roux-Y gastrojejunostomy PubMed Central articles Roux-Y gastrojejunostomy 2023 articles Roux-Y gastrojejunostomy 2024 articles Roux-Y gastrojejunostomy Scopus articles Roux-Y gastrojejunostomy impact factor journals Roux-Y gastrojejunostomy Scopus journals Roux-Y gastrojejunostomy PubMed journals Roux-Y gastrojejunostomy medical journals Roux-Y gastrojejunostomy free journals Roux-Y gastrojejunostomy best journals Roux-Y gastrojejunostomy top journals Roux-Y gastrojejunostomy free medical journals Roux-Y gastrojejunostomy famous journals Roux-Y gastrojejunostomy Google Scholar indexed journals kidney articles kidney Research articles kidney review articles kidney PubMed articles kidney PubMed Central articles kidney 2023 articles kidney 2024 articles kidney Scopus articles kidney impact factor journals kidney Scopus journals kidney PubMed journals kidney medical journals kidney free journals kidney best journals kidney top journals kidney free medical journals kidney famous journals kidney Google Scholar indexed journals gastrojejunostomy articles gastrojejunostomy Research articles gastrojejunostomy review articles gastrojejunostomy PubMed articles gastrojejunostomy PubMed Central articles gastrojejunostomy 2023 articles gastrojejunostomy 2024 articles gastrojejunostomy Scopus articles gastrojejunostomy impact factor journals gastrojejunostomy Scopus journals gastrojejunostomy PubMed journals gastrojejunostomy medical journals gastrojejunostomy free journals gastrojejunostomy best journals gastrojejunostomy top journals gastrojejunostomy free medical journals gastrojejunostomy famous journals gastrojejunostomy Google Scholar indexed journals
Article Details
1. Introduction
Pyloric Stenosis is defined as an obstruction to gastric emptying due to any cause situated above the biliary ampulla. Left untreated, pyloric stenosis may lead to severe denutrition, gastric stasis and discomfort, eventually Gastroesophageal reflux disease GERD. Findings of systemic review show that the incidence of peptic esophagal stricture is 12% [1]. The incidence of adult pyloric stenosis is not yet certainly determinated [2]. Thus the association of both esophageal stenosis and pyloric stenosis regardless of the aetiology is rare. The co-existence of both esophageal stricture and pyloric stenosis imposes to evaluate the adequate therapeutic approach. Hence our purpose is to report the clinical presentation of a rare coexisting peptic esophageal stricture and pyloric stenosis, the decision-making process, and finally the outcome. Oral and written consent were acquired
2. Clinical Case
2.1 Patient history
The patient was a 67-year-old North African man, chronic smoker with history of gastric ulcer at the age of 31 years-old. Clinical evolution was clear until 2009 when the patient reported experiencing gastroesophageal reflux syndrome worsened progressively until 2012 where symptoms of dysphagia occurred, associated with vomitus, which mainly consisted of undigested food. The patient also reported abdominal distention and discomfort with persistence of abdominal pain. His medical history assessed a weight loss of 19kg over 9 years.
2.2 Clinical findings
Physical exam revealed abdominal wheelbase in the epigastric area. The remainder of the examination was standard except a BMI of 16.56. The patient’s biology tests revealed no hydroelectrolitic disorders. An upper endoscopy (EGD) demonstrated regular, fibrous and impassable stenosis beginning 32cm from the incisor teeth. No biopsy could be taken. To complete further exploration of the digestive tract the patient underwent barium-meal examination of Oeso-gastroduodenal transit revealing extended central stenosis of the lower esophagus. The barium-filling imprint showed a dilatation of the middle and upper esophagus, thus marking a luminal diameter disparity (Figure 1.1). The images revealed in addition a stasis stomach with antrum mark attaining the pelvic area and post-bulbar double bubble appearance (Figure 1.2). A contrast-enhanced abdominal computed tomography (CT) Scan showed stasis stomach on pyloric stenosis. The clinical presentation and the examination findings comforted the diagnosis of a benign esophageal stricture.
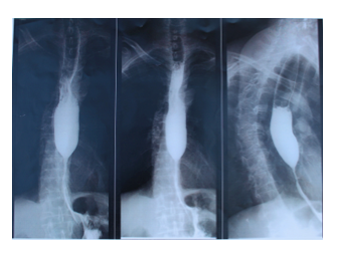
Figure 1.1: Barium-filling imprint showing a dilatation of the middle and upper esophagus, thus marking a luminal diameter disparity.
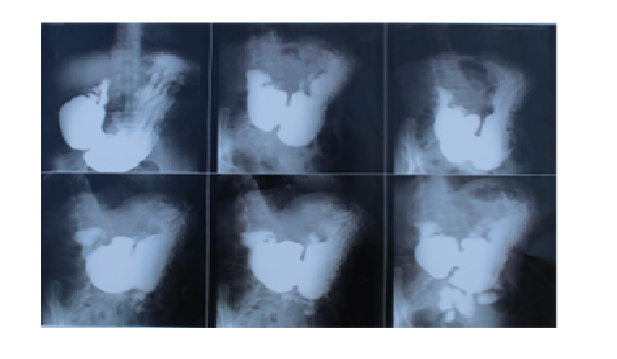
Figure 1.2: Barium-filling imprint revealing a stasis stomach with antrum mark attaining the pelvic area and post-bulbar double bubble appearance.
2.3 Therapeutic intervention
The therapeutic strategy decided was an endoscopic eosophageal dilatation and medical preparation followed by an antrectomy and Roux-en-Y diversion surgery. Upper endoscopy (EGD) with Endoscopic dilatation was preceded by two consecutive weeks of medical preparation consisting of double dose of Proton Pomp Inhibitor medication. The upper endoscopy showed a persistence of the fibrous central stenosis. Dilation succeeded applying a pressure of 2 to 4 ATM (Automated Teller Machine) with balloon dilators. Exploration of the stomach proceeded showing a stasis stomach with large dilatation. In total five biopsies were taken, three from the antrum and two from the fundus, showing a chronic funditis and chronic antritis, a stomach Helicobacter Pylori free, and no sign of metaplasia or dysplasia. The pyloric stenosis appeared morphologically homogeneous and symmetric without induration nor inflammatory signs. Thereafter, the operation went under general anesthesia by median laparotomy due to previous surgical intervention. Surgical Exploration found a stasis stomach presentation. Antrectomy was performed followed by a Roux-en-Y anastomisis. The surgery was uneventful and the anatomo-pathology examination of the operative specimen confirmed no malignancy.
2.4 Follow-up and outcome
Two days after surgery the nasogastric tube was removed, and the patient was advised initially on a clear liquid diet for the first 24h hours. The diet was advanced to full liquids on the following day and the patient was discharged home 4 days later. Six months after surgery, the patient was symptom free and tolerating a regular diet.
3. Discussion
We experienced a rare association of co-existing pyloric stenosis and peptic esophageal stricture, described in published literature in very few articles since 1979 [3]. The treatment of peptic pyloric stenosis is inevitably surgical, but medical preparation is nonetheless key to better outcome, aiming to regulate ulcer activity, restore hydroelectrolitic disorders if there is, and improve patient’s general condition. Three surgical techniques are possible: antrectomy with gastroduodenostomy (Billroth I), with gastrojejunostomy (billroth II), and most recently antrectomy with Roux-Y gastrojejunostomy; all associated with a selective vagotomy. Billroth I and Billroth II were the most used methods of alimentary reconstruction following gastric resection for decades, meanwhile since its introduction by Anton Wolfer in 1883 Roux-en-Y has gained acceptance and proved effectiveness in the management of bilious vomiting, retro anastomotic herniation, blind loop syndrome and dumping syndrome [4]. In an article of duodenal ulcer disease cases studies comparing gastroduodenostomy with Roux-Y gastrojejunostomy after antrectomy and selective gastric vagotomy demonstrated that Roux-Y gastrojejunostomy procedure was effective in preventing bile reflux [4]. However, postoperative complication and clinical course, such as morbidity rate were similar [4]. Therefore we chose Roux-Y gastrojejunostomy after antrectomy technic.
The treatment of peptic esophageal stricture on the other hand is consensual and includes a variety of therapeutic options, including balloon dilation, temporary stent placement, surgery, intralesional steroid injection and incisional therapy. The treatment selection follow an algorithm previously described by van Boeckel and Siersema, which starts by Endoscopically or fluoroscopically guided dilation [5] which is a safer, rapid and economical alternative. Considering the co-existence of both conditions with an important toneless stomach stasis and imbalance of gastric emptying due stenosis of both ends, we decided to initially dilate the peptic esophageal stricture and carry on Roux-Y gastrojejunostomy after antrectomy with bivagotomy. The association of both techniques meets all requirements. Indeed the endoscopic dilatation enable further exploration of the stomach and comfort the histological diagnosis of benign stricture, while Roux-Y gastrojejunostomy after antrectomy with bivagotomy allows to reduce gastric stasis and treat the stricture, the gastric reflux and finally the ulcer.
References
- Repici C. Hassan, SHARMA P, et al. Systematic review: the role of self-expanding plastic stents for benign oesophageal strictures Epub (2010): doi: 10.1111/j.1365-2036.2010.04301.x.
- Louis Kreel', Harold Ellis. Pyloric stenosis in adults: A clinical and radiological study of 100 consecutive patients Gut 6 (1965): 253.
- Calvet J, Claux J, Coll J. Peptic stenosis of the cardia with pyloric stenosis. 2 cases. 86 (1969): 517-522.
- Ulf H. Haglund, Roland L. Jansson, Jacob GE, et al. Primary Roux-Y gastrojejunostomy versus gastroduodenostomy after antrectomy and selective vagotomy 159 (1990): 546-549.
- Van Boeckel PG, Siersema PD. Refractory esophageal strictures: what to do when dilation fails. 10.1007/s11938-014-0043-6.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
