Recovery of Sudden Cardiac Death- Role of Chain of Survival: A Case Report
Article Information
José Edgar Cervantes-Navarro1, Jorge Ayón-Aguilar2, Ernesto López-Luna1, Jander Narváez-Acosta1, Anita Gutiérrez-Romero3
1Hospital General “Dr. Eduardo Vázquez Navarro”, Puebla, México
2Hospital General Regional # 36. Instituto Mexicano del Seguro Social, Puebla, México
3Universidad Autónoma de Tlaxcala, México
*Corresponding Author: Dr. Jorge Ayón-Aguilar, Hospital General Regional # 36, Instituto Mexicano de Seguro Social, 10 poniente 2721, Colonia San Alejandro, Puebla, Puebla, México.
Received: 20 November 2019; Accepted: 04 December 2019; Published: 13 January 2020
Citation: José Edgar Cervantes-Navarro, Jorge Ayón-Aguilar, Ernesto López-Luna, Jander Narváez-Acosta, Anita Gutiérrez-Romero. Recovery of Sudden Cardiac Death- Role of Chain of Survival: A Case Report. Archives of Clinical and Medical Case Reports 4 (2020): 080-085.
View / Download Pdf Share at FacebookAbstract
Sudden cardiac death consists in a sudden cardiac collapse or heart failure secondary to arrhythmia, which unexpectedly occurs within the first hour after the onset of symptoms. Fibrillation and ventricular tachycardia are two arrhythmias responsible for most sudden cardiac arrest events. Others arrhythmias that produce this is asystole and pulseless electrical activity. The backbone in the treatment of sudden cardiac death is the immediate activation of the Chain of Survival with de early implementation of CPR and defibrillation, thus improving the prognosis of survival of patients. The automated implantable cardioverter defibrillator is a device with a high chance of reverting events caused by these arrhythmias to a sinus rhythm. We report a case of a 40-year old man who presented symptoms 20 minutes before being admitted to emergency services. An electrocardiogram was obtained, showing presence of QRS complex overlap in DI, DII and aVF. A skull computerized axial tomography scan showed no evidence of cerebral edema or located injuries. An echocardiogram showed normal heart size, left ventricle ejection fraction of 70%, valves without injuries, and no data regarding pulmonary arterial hypertension. Five days after the cardiac arrest event, an AICD was implanted as primary prevention strategy.
Keywords
Sudden cardiac death (SCD); Chain of survival (COS); Automated implantable cardioverter defibrillator (AICD)
Sudden cardiac death (SCD) articles, Chain of survival (COS) articles, Automated implantable cardioverter defibrillator (AICD) articles
Sudden cardiac death articles Sudden cardiac death Research articles Sudden cardiac death review articles Sudden cardiac death PubMed articles Sudden cardiac death PubMed Central articles Sudden cardiac death 2023 articles Sudden cardiac death 2024 articles Sudden cardiac death Scopus articles Sudden cardiac death impact factor journals Sudden cardiac death Scopus journals Sudden cardiac death PubMed journals Sudden cardiac death medical journals Sudden cardiac death free journals Sudden cardiac death best journals Sudden cardiac death top journals Sudden cardiac death free medical journals Sudden cardiac death famous journals Sudden cardiac death Google Scholar indexed journals SCD articles SCD Research articles SCD review articles SCD PubMed articles SCD PubMed Central articles SCD 2023 articles SCD 2024 articles SCD Scopus articles SCD impact factor journals SCD Scopus journals SCD PubMed journals SCD medical journals SCD free journals SCD best journals SCD top journals SCD free medical journals SCD famous journals SCD Google Scholar indexed journals Chain of survival articles Chain of survival Research articles Chain of survival review articles Chain of survival PubMed articles Chain of survival PubMed Central articles Chain of survival 2023 articles Chain of survival 2024 articles Chain of survival Scopus articles Chain of survival impact factor journals Chain of survival Scopus journals Chain of survival PubMed journals Chain of survival medical journals Chain of survival free journals Chain of survival best journals Chain of survival top journals Chain of survival free medical journals Chain of survival famous journals Chain of survival Google Scholar indexed journals COS articles COS Research articles COS review articles COS PubMed articles COS PubMed Central articles COS 2023 articles COS 2024 articles COS Scopus articles COS impact factor journals COS Scopus journals COS PubMed journals COS medical journals COS free journals COS best journals COS top journals COS free medical journals COS famous journals COS Google Scholar indexed journals Automated implantable cardioverter defibrillator articles Automated implantable cardioverter defibrillator Research articles Automated implantable cardioverter defibrillator review articles Automated implantable cardioverter defibrillator PubMed articles Automated implantable cardioverter defibrillator PubMed Central articles Automated implantable cardioverter defibrillator 2023 articles Automated implantable cardioverter defibrillator 2024 articles Automated implantable cardioverter defibrillator Scopus articles Automated implantable cardioverter defibrillator impact factor journals Automated implantable cardioverter defibrillator Scopus journals Automated implantable cardioverter defibrillator PubMed journals Automated implantable cardioverter defibrillator medical journals Automated implantable cardioverter defibrillator free journals Automated implantable cardioverter defibrillator best journals Automated implantable cardioverter defibrillator top journals Automated implantable cardioverter defibrillator free medical journals Automated implantable cardioverter defibrillator famous journals Automated implantable cardioverter defibrillator Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals defibrillator articles defibrillator Research articles defibrillator review articles defibrillator PubMed articles defibrillator PubMed Central articles defibrillator 2023 articles defibrillator 2024 articles defibrillator Scopus articles defibrillator impact factor journals defibrillator Scopus journals defibrillator PubMed journals defibrillator medical journals defibrillator free journals defibrillator best journals defibrillator top journals defibrillator free medical journals defibrillator famous journals defibrillator Google Scholar indexed journals patient articles patient Research articles patient review articles patient PubMed articles patient PubMed Central articles patient 2023 articles patient 2024 articles patient Scopus articles patient impact factor journals patient Scopus journals patient PubMed journals patient medical journals patient free journals patient best journals patient top journals patient free medical journals patient famous journals patient Google Scholar indexed journals cardioverter defibrillator articles cardioverter defibrillator Research articles cardioverter defibrillator review articles cardioverter defibrillator PubMed articles cardioverter defibrillator PubMed Central articles cardioverter defibrillator 2023 articles cardioverter defibrillator 2024 articles cardioverter defibrillator Scopus articles cardioverter defibrillator impact factor journals cardioverter defibrillator Scopus journals cardioverter defibrillator PubMed journals cardioverter defibrillator medical journals cardioverter defibrillator free journals cardioverter defibrillator best journals cardioverter defibrillator top journals cardioverter defibrillator free medical journals cardioverter defibrillator famous journals cardioverter defibrillator Google Scholar indexed journals AICD articles AICD Research articles AICD review articles AICD PubMed articles AICD PubMed Central articles AICD 2023 articles AICD 2024 articles AICD Scopus articles AICD impact factor journals AICD Scopus journals AICD PubMed journals AICD medical journals AICD free journals AICD best journals AICD top journals AICD free medical journals AICD famous journals AICD Google Scholar indexed journals
Article Details
Abbreviations:
SCD: Sudden Cardiac Death; V-fib: Ventricular Fibrillation; VT: Ventricular Tachycardia; COS: Chain Of Survival; CPR: Cardiopulmonary Resuscitation; EMS: Emergency Medical Services; AICD: Automated Implantable Cardioverter Defibrillator; CT: Computarized Tomography Scan; GCS: Glasgow Coma Scale
1. Introduction
Sudden cardiac death (SCD) consists in a sudden cardiac collapse or heart failure after heart arrhythmia in subjects with or without heart disease, and causes death if not treated within the minutes after its onset. Some of these subjects show symptoms shortly before the event, but in order to establish a definitive diagnosis of a SCD episode, the symptoms should last for at least one hour [1].
2. Definition
An event is considered SCD if it occurs unexpectedly within the first hour after the onset of symptoms or if it happens in the absence of any witnesses when the deceased was seen in good condition 24 before dying [2].
3. History
There is data of SCD events from long ago. The Ebers papyrus states “if a subject shows signs of pain in the arm and the left half of the thorax, it is a death threat”. Later in China, 2,500 years ago, Chio matched SCD with arrhythmia when he said, “intermittent pulse is a predictor for imminent death”. Hippocrates also claimed “intense precordial pain irradiating to the collarbone and the back is a sign of a bad prognosis” [3].
4. Incidence and Prevalence
SCD is a global public health issue. It is a leading cause of death in children and young adults. The most common causes of SCD are congenital abnormalities, presumed primary arrhythmia and coronary artery disease [4]. However, a certain percentage of autopsy-negative cases of SCD in the young (< 35 years) remain unexplained even after a post-mortem genetic testing. Autoantibodies against cardiac proteins may be potentially involved in the pathogenesis of different heart diseases and in the occurrence of unexplained SCD [5]. It has been reported in different locations and it still makes up 20-30% of cardiac-related deaths; the incidence is 32.1 events per million inhabitants/year in France, 41.3 events per 100,000 inhabitants/year in China, and between 70 and 155 events per 100,000 inhabitants/year in the USA. We still don’t know the incidence and prevalence in Mexico, but we can estimate the number of victims of SCD; in 2008, 59,579 adults died of ischemic cardiomyopathy, and is likely that in at least 30% of that population it was a sudden event, which represents 17,873 events/year [6].
5. Arrhythmias Causing SCD
Ventricular fibrillation (V-fib) and ventricular tachycardia (VT) are two arrhythmias responsible for most sudden cardiac arrest events. Other rhythms causing this event are asystole and pulseless electrical activity. The involvement of substrates and triggers of arrhythmia, substrates plus ischemia, myocardial fibrosis and genetic anomalies are required for an episode of V-fib or VT to happen [6]. Non-pacemaker myocardial cells from atriums and ventricles, which in normal conditions don’t show spontaneous activity, could show automation properties. A significant difference between an altered normal automatism and an anomalous automatism is that the latter is less sensitive to suppression by overstimulation; in these circumstances an automatic locus can exhibit features from other mechanisms of arrhythmia (VT) [7].
6. Chain of Survival
Chain of survival (COS) aims to demonstrate the interrelationship between key stages of resuscitation and emphasises the need for all links to be fast and effective in order to optimize the chances of achieving neurologically intact survival. COS focuses on specific interventions rather than the potential for the effectiveness of each. The contribution of each of the four interventions (1. Early recognition and call for help, 2. Early CPR, 3. Early defibrillation and 4. Post-resuscitation care) diminishes rapidly as patients succumb at each stage and the actual attrition rate results in rapidly decreasing numbers of patient progressing along the chain, with only a small minority of patients who enter the initial link in the COS actually progressing through to the final link. Greatest benefit in improving outcome will be achieved by focussing on improving care at links in the chain where there is the greatest number of patients [8]. COS could lead to the survival of a considerable number of SCD victims if executed quickly. Those actions must be perfectly connected with each other to be efficient [9]. From “Early recognition and call for help” to “Early CPR”. Although multifactorial, a surprisingly low proportion of patients identified by the Emergency Medical Services (EMS) as being in cardiac arrest progress to an actual resuscitation attempt by and EMS responder. Although bystander rates of resuscitation are generally improving globally, the majority of patients in cardiac arrest still receive their initial CPR by an EMS responder. From “Early recognition and call for help” to “Early defibrillation”. The proportion of patients in a shockable rhythm as their initial rhythm has declined over the past 20 years. Currently, are reporting shockable initial rhythms in approximately 25% of cardiac arrests. From “Early recognition and call for help” to “Post-resuscitation care”. Sustained return of spontaneous circulation has been reported in 25% of cases [8].
7. Early Defibrillation
The backbone of effective treatment of sudden cardiac death is early defibrillation, an essential link within the COS [9]. The automated implantable cardioverter defibrillator (AICD) is a device with a high chance of reverting V-fib or VT to a sinus rhythm, since it is able to defibrillate any of these arrhythmias in less than 15 seconds. The AICD has proven its value both in primary prevention of SCD in subjects with an ejection fraction less than 35%, and in secondary prevention in subjects that already survived a sudden cardiac arrest event [6]. The AICD successfully treats arrhythmic events and reduces total mortality in patients after the first occurrence of cardiac arrest.
The MADIT study represents the first primary prevention analysis using therapy involving AICD; this study showed a significant decrease in mortality rates with conventional therapy [10]. The MADIT II study is the sequel of the previous study, in which a significant benefit in patients with previous myocardial infarct, low ejection fraction, spontaneous non-continuous VT and continuous VT was already proven; it was conducted in 71 USA centers and 5 European centers, and it included over 1,200 patients [11]. On the other hand, AVID study compared the effectiveness of anti-arrhythmic drugs (empiric amiodarone) versus AICD in patients with documented severe VT; this study had a premature termination once it proved that mortality rates were decreased by 39% in the group with implanted AICD [12]. Survival rate after 5 years is 89.9% [13].
8. Case Presentation
Patient: 40-year-old male, public transportation driver with relevant cardiovascular background, such as a) obesity; b) sedentary lifestyle; c) occasional consume of alcohol; and d) occasional smoker. The symptoms started 20 minutes before being admitted to emergency services; he was sitting at home; he showed signs of hyperextension of both arms, as well as arched neck and conjugate gaze deviation (descerebrate posture) without recovering his alert state, which is why he was assigned to our unit 5 minutes before an episode of respiratory arrest.
Upon his arrival to the Shock area, the patient was screened and he showed inconsistency of miotic and isochoric pupils and he also was pulseless, so COS was activated for cardiac arrest to start CPR. The heart rate was monitored and V-fib was spotted, which was defibrillated with 200 J two-phase shock twice, resulting in a sinus rhythm (Figure 1) with carotid pulse and restoration of spontaneous circulation and vital signs such as: heart rate 86 beats per minute, blood pressure 100/59 mmHg. An electrocardiogram was obtained, showing presence of QRS complex overlap in DI, DII and aVF. Post-cardiac arrest care and mechanical ventilation were included, and also laboratory analysis: hemoglobin by hematic biometry 15.4 g/dl; platelets 243,000 10<3/μL, white blood cells 10.63 <3/μ, neutrophils 46.1%, partial thromboplastin time 26.0 sec, prothrombin time 15.8 sec, percentage 81%, INR 1.16, glucose 142 mg/dl, blood urea nitrogen (BUN) 9 mg/dl, urea 19.3 mg/dl, creatinine 1.0 mg/dl, creatinine phosphokinase (CK) 114 U/L, creatinine kinase MB fraction (CK MB) 99 U/L, cholesterol 160 mg/dl, triglycerides 260 mg/dl, sodium 140 mmol/L, potassium 3.4 mmol/L, chloride 101 mg/dl, total bilirubin 1.2 mg/dl, lactate dehydrogenase 1660 U/L, overall urinalysis: density 1.015, negative for ketone bodies, white blood cells 6-10 counts/mL.
A skull computerized axial tomography scan (CT) was performed, which showed no evidence of cerebral edema or located injuries. An echocardiogram was also performed, resulting: normal heart size, left ventricle ejection fraction of 70%, valves without injuries, and no data regarding pulmonary arterial hypertension. We requested the assistance of control laboratories, and the results were: CK 360 U/L, CK MB 47 U/L, albumin 3.4 g/dl, sodium 143 mmol/L, potassium 4.0 mmol/L, chloride 107 mg/dl, glucose 127 mg/dl, BUN 17 mg/dl, urea 36.4 mg/dl, creatinine 1.1 mg/dl. A control electrocardiogram 12 hours after showed a sinus rhythm with no evidence of injury, ischemia or necrosis.
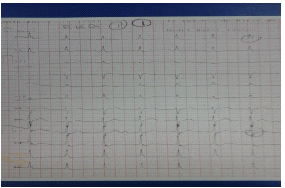
Figure 1: Patient electrocardiogram after CPR upon arriving to emergency services.
During his stay in the Shock area 48 hours after the event, the tubes were successfully removed. The neurological assessment showed no signs of cognitive impairment, no focalization data and a Glasgow Coma Scale (GCS) 15/15.
A coronarography was performed, and it showed healthy arteries. Five days after the cardiac arrest event, an AICD was implanted as primary prevention strategy (Figure 2), which was placed on the eighth day with the following conclusions: a) idiopathic VT; b) recovery from sudden cardiac death; c) VDD BIOTRONIK pacemaker implanted. He was discharged 9 days after his admission, with GCS 15/15, neurologically intact, and he was scheduled for several follow-up cardiology appointments.
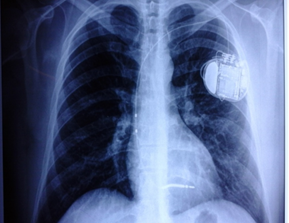
Figure 2: Thorax radiography taken before discharging the patient, in which the AICD is shown.
Acknowledgements
We would like to thank to Guillaume Marc Jackie Leriche for supporting us to translate this manuscript.
Conflicts of Interest:
None
References
- González-Melchor L, Villareal-Molin T, Iturralde-Torres P, et al. Muerte súbita cardíaca en el corazón estructuralmente normal: una actualización (Sudden cardiac death in a structurally normal heart: an update). Mex Card Arch 84 (2014): 293-304.
- Bayés de Luna A, Elousa R. Muerte súbita (Sudden death). Rev Esp Card 65 (2012): 1039-1052.
- Gutiérrez-Báez YM, Castellanos-Rojas R, Ferrer-Herrera I, et al. Muerte súbita cardiovascular (Sudden cardiac death). Revista Finlay 5 (2015).
- Garritano NF, Willmarth-Stec M. Student athletes, sudden cardiac death, and lifesaving legislation: A review of literature. J Ped HC 29 (2015): 233-242.
- Ryabkova VA, Shubik YV, Erman MV, et al. Lethal immunoglobulins: autoantibodies and sudden cardiac death. J Autorev 18 (2018): 415-425.
- Rodríguez-Reyes H, Muñoz-Gutiérrez M, Márquez MF, et al. Muerte súbita cardiaca. Estratificación de riesgo, prevención y tratamiento (Sudden cardiac death. Risk stratification, prevention and treatment). Mex Card Arch 85 (2015): 329-336.
- Gaztañaga L, Marchlinski FE, Betensky BP. Mecanismo de arritmias cardíacas (Mechanism of cardiac arrhythmias). Rev Esp Card 65 (2012): 174-185.
- Deakin CD. The chain of survival: not all links are equal. J Resuscitation 126 (2018): 80-82.
- Marín-Huerta E, Peinado R, Asso A, et al. Muerte súbita cardíaca extrahospitalaria y desfibrilación precoz (Outpatient sudden cardiac death and early defibrillation). Rev Esp Card 53 (2000): 851-865.
- Mendoza-González C. Utilidad del desfibrilador automático implantable en la prevención de muerte súbita. Resultados de la medicina basada en evidencia (Using the automated implantable cardioverter defibrillator for sudden death prevention. Results of evidence-based medicine). Mex Card Arch 77 (2007): 44-46.
- Brugada P. La interrupción prematura del Estudio MADIT II: ¿un gran impacto a la economía sanitaria? (Early termination of the MADIT II study: a huge impact on health economy?) Rev Esp Card 55 (2002): 87-88.
- Porres-Aravama JM, Marco-Garde P. Muerte súbita cardíaca y MADIT II (Sudden cardiac death and MADIT II). Med Int 27 (2003): 410-416.
- Carmona-Salinas JR, Basterra-Sola N. Prevención de muerte súbita en pacientes en espera de trasplante cardíaco (Prevention of sudden death in patients waiting for heart transplantation). Rev Esp Card 53 (2000): 736-745.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
