Strangulation of Heart Due to Calcified Constrictive Pericarditis Causing Right Heart Failure
Article Information
Md Faisal Talukder, Li Hongxin*, Liang Fei
Department of Cardiovascular Surgery, Shandong Provincial Hospital Affiliated to Shandong University, Jinan, Shandong, 250021, China
*Corresponding author: Li Hongxin, MD; Department of Cardiovascular Surgery, Shandong Provincial Hospital affiliated to Shandong University, Jinan, Shandong, 250021, China
Received: 13 January 2020; Accepted: 18 January 2020; Published: 21 January 2020
Citation: Md Faisal Talukder, Li Hongxin, Liang Fei. Strangulation of Heart Due to Calcified Constrictive Pericarditis Causing Right Heart Failure. Cardiology and Cardiovascular Medicine 4 (2020): 039-044.
View / Download Pdf Share at FacebookAbstract
Background: Constrictive Pericarditis (CP) results from fibrosis and calcification of pericardium. CP can be present with the assemblage of symptoms due to strangulation of heart. However, right heart failure due to localized calcified CP is exceptionally unmatched.
Case Report: A 32-year-old female patient hailing to our hospital with the complaint of dyspnea, right upper abdominal pain, ascites, and bilateral pedal edema in May 2018. After proper investigation, she diagnosed with subacute right heart failure due to localized calcified CP. Therefore, she managed with diuretic therapy and symptomatic treatment. After one year, she suddenly present in the emergency department with the features of right heart failure. Her New York Heart Association (NYHA) score was class-III. After proper medical management of her symptoms, she underwent off-pump partial pericardiotomy with no complaints. Analgesics, Antibiotics, and diuretics were administered in the post-operative period. She was discharged on the 6th post-operative day with no symptoms of right heart failure.
Conclusion: Herein, we report a very unusual presentation with localized CP, causing strangulation of heart, which had been treated successfully with off- pump partial pericardiotomy. Meticulous dissection is the key to a successful pericardiotomy.
Keywords
Constrictive Pericarditis; Strangulation of Heart; Right Heart Failure
Constrictive Pericarditis articles, Strangulation of Heart articles, Right Heart Failure articles
Article Details
Background
Constrictive pericarditis is a rare disease of the pericardial sac, characterized by thick pericardial fibrosis and calcification that causes progressively impaired diastolic filling of the heart [1]. The loss of normal elasticity of the pericardial sac is caused by CP. The presence of calcification supports the diagnosis, but not all patients with constrictive pericarditis have calcification [2]. Localized pericardial constriction was reported as a rare form of constrictive pericarditis [3,4]. The people from underdeveloped countries are suffered from CP mostly. Either viral or bacterial infection can cause CP. However, when CP is caused by bacteria, it is most likely related to tuberculosis. Regrettably, CP can be idiopathic. Early diagnosis is vital for timely medical management as well as pericardiotomy. Timely surgical intervention enhances the post-operative clinical outcome and quality of patient's life. Clinically, early diagnosis is effortful unless until radiological signs (‘egg shell’ sign) appeared in chest X-ray. However, high suspicion index and meticulous evaluation of waveforms of jugular venous pressure can be helpful. An experienced echocardiographer with high-resolution echocardiography machines can identify most of the suspected cases of CP.
Case Presentation
A 32-year-old female was wheeled in our emergency department with the features of RHF and NYHA class-III. She was a farmer and was living with her family in the rural area. Previously, in May 2018, she was admitted to our hospital with the complaint of dyspnea, right upper abdominal pain, ascites, and bilateral pedal edema. Consequently, she was diagnosed with localized calcified CP and was managed by diuretic therapy. During the last two months, she experienced occasional paroxysmal nocturnal dyspnea, which was worsened upon lying flat. She denied any chest pain. She had no history of coronary artery disease, thoracic trauma, diabetes, or any other chronic diseases.
During the physical examination, the patient was restless. It revealed an elevation of jugular venous pressure and tender, mild hepatomegaly. The abdomen and both the jugular veins (JVD ~ > 16mmH2O) were highly distended. Chest auscultation demonstrated a 'cardiac knock,' and both S1 and S2 were muffled. Abdominal palpation revealed gross ascites. The lower extremities were cold to touch with moderate bilateral pitting edema from the knee and below. Arterial blood pressure and the pulse pressure are reduced as the diastolic component remains normal. The elevation of the systolic pressure and pulse pressure are ubiquitous after surgery in these patients. Pre and post-operative vitals are tabulated in Table.1.
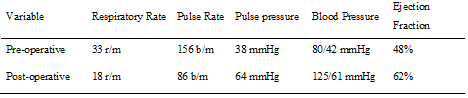
r/m = Respirations per minute, b/m = Beats per minute, mmHg = millimeter of Mercury.
Table 1. Pre-operative and post-operative respiratory and hemodynamic vitals.
Diagnostic Procedures
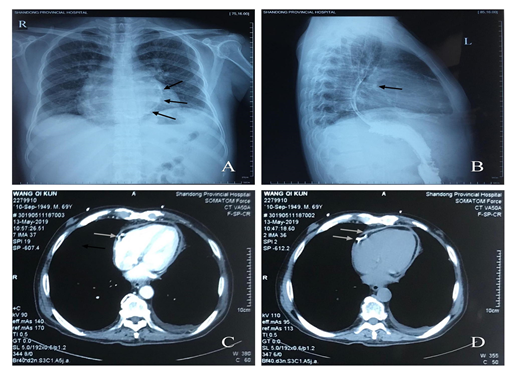
Comprehensive studies established the diagnosis of localized calcified CP. An electrocardiograph revealed low voltage QRS complex, non-specific ST-segment and T wave changes. However, a plain chest X-ray (Figure 1: Panel A and B) showed pericardial calcification (arrows). A TTE (2D, four-chamber view) revealed dyskinesia of the right ventricle (RV) due to the presence of a thickened (calcified) pericardium on its wall, mild right atrium enlargement and ejection fraction (EF) of 48%. Abdominal ultrasonography demonstrated hepatic vein engorgement, mild hepatomegaly, and moderate to severe ascites. However, a CTA (Figure 1: Panel C and D) demonstrated calcification of pericardium (arrows).
Operative Procedure
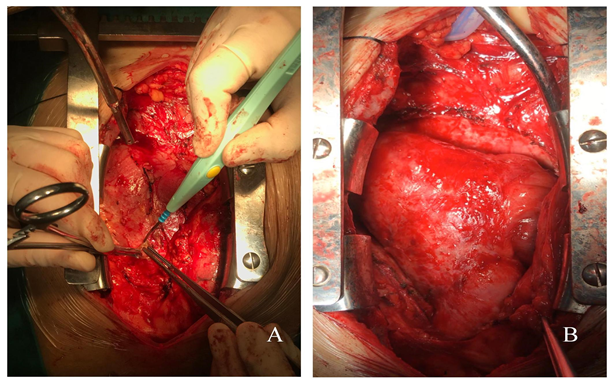
With evidence of CP confirmed, the patient underwent through an off-pump partial pericardiectomy by a standard midline sternotomy that was performed in the cardiac surgery operation theatre. We approached the pericardium from the free RV wall (junction with right atrium) by using a combination of cautery, scissors, and sharp hooks (Figure 2: Panel A). After the decortication process (Figure 2: Panel B), the freed from strangulation, and these led to adjustments of ventricular pressures and cardiac output. A tissue sample from pericardium was sent for histopathological study and was noted to have.
Discussion
Our case was unusual in both course and presentation. Commonly, CP is known to take a chronic course, and medical therapy plays a palliative role in most of the cases. Unanticipatedly, our patient was presented with sudden RHF that was unusual in someone with a very unremarkable past medical history. Our patient experienced these clinical symptoms because there were right ventricular free wall compression and strangulation of heart. CP should be taken into consideration when generalized symptoms of RHF and decreased cardiac out-put are present [5]. Elevation and equalization of ventricular filling pressures is also a common presentation in patients with CP.
The most common etiologies of CP include viral infection, bacterial infection/tuberculosis, various neoplasm, following cardiac surgery, connective tissue disorder, trauma, renal failure, radiation therapy, foreign body in the pericardium, pacemaker/AICD insertion, and idiopathic. In our patient, there was no such history. Moreover, pericardial histopathology report revealed no evidence of tuberculosis, acute inflammation, granulomatous inflammation, and tumor. Therefore, in our case, the final diagnosis was idiopathic localized calcified CP. Oftentimes there is an occult event that sparks inflammation of the pericardium, leading to fibrosis with calcification.
The myriad of complications, including death, are associated with pericardiectomy (partial or complete). Preoperative functional status is an influential risk factor for death in the early hazard phase after operation [6]. Thus, early risk approaches zero for patients in New York Heart Association (NYHA) functional class I or II preoperatively, 10% (CL 8%-14%) for those in NYHA class III, and 46% (CL 29%-64%) for those in NYHA class IV [6].In a recent European study (Busch et al.) revealed RV dilation and EF < 55% were the risk factors for (early/late) mortality in post-pericardiotomy period. Despite NYHA class III and EF of 48%, our patient recovered spontaneously due to standard ventricular dimensions and absence of associated lesions (tricuspid or septal). Post-operative treatment was centered on pain management using NSAIDs and liquidation of edema and ascites using low doses of Spironolactone and Furosemides. On the 6th post-operative day, the patient was discharged from the hospital with free of symptoms (NYHA-Class I).
The prognosis is poor if the pericardiotomy cannot be performed because it is the only established treatment for chronic constrictive pericarditis. The morbidity of patients increases gradually. Later, patients become bedridden and need frequent paracentesis for recurrent ascites. In comparison with medical treatment, surgical treatment inarguably improves the post-operative prognosis. Nowadays, with the advancement of surgical and anesthetic techniques, the mortality rate of CP is < 5%.
Conclusion
It is highlighted that each patient presenting with dyspnea, ascites, hepatomegaly, and raised jugular venous pressure should be thoroughly investigated for CP. The significance of these painstaking investigations in a patient with suspected CP arises from the fact that, if appropriately diagnosed, a surgical procedure (pericardiotomy) will be curative.
Abbreviations
CP: Constrictive pericarditis;
RHF: Right heart failure;
CTA: Computed tomography angiography;
EF: Ejection fraction;
TTE: Transthoracic echocardiography;
NYHA: New York Heart Association.
Acknowledgments
None.
Consent
Hospital Ethics committee approved publication. Informed consent was obtained from the patient for publication of this report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
References
- Butany J, El DD, Collins MJ, Nair V, Israel N, Woo A, Cusimano RJ. Constrictive pericarditis: case presentation and a review of the literature. The Canadian journal of cardiology 20 (2004): 1137-1144.
- Bogaert J, Francone M. Pericardial disease: value of CT and MR imaging. Radiology 267 (2013): 340-356.
- Iseki H, Kayaba Y, Tamura T, Uzawa H, Suko Y, Miyamoto K. Localized pericarditis with calcifications mimicking a pericardial tumor. Internal medicine 38 (1999): 355-358.
- Schofield RS, Dorman Jr SM, Aranda Jr JM, Hill JA, Pauly DF, Klodell CT. Constrictive pericarditis presenting as a calcified anterior cardiac mass. The Annals of thoracic surgery 87 (2009): 1597-1599.
- Kwan DM, Dhaliwal G, Baudendistel TE. Thinking inside the box. Journal of hospital medicine 3 (2008): 71–76.
- McCaughan BC, Schaff HV, Piehler JM, Danielson GK, Orszulak TA, Puga FJ, Pluth JR, Connolly DC, McGoon DC. Early and late results of pericardiectomy for constrictive pericarditis. The Journal of Thoracic and Cardiovascular Surgery 89 (1985):340-350.


 Impact Factor: * 3.5
Impact Factor: * 3.5 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 14.80%
Acceptance Rate: 14.80%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 