Stroke in Setting of Persistent Trigeminal Artery: Report of Two Cases
Article Information
Sandeep Moudgil1, Sapna Jangral2, Lokesh Singh3*, Anupam Jhobta4
1Assistant Professor Neuroradiology, Department of Radiodiagnosis, Block –D IGMC Shimla, India
2Senior Resident, Department of Radiodiagnosis, Block –D IGMC Shimla, India
3Research Associate, Department of Radiodiagnosis, PGIMER, Chandigarh, India
4Professor and Head, Department of Radiodiagnosis, Block –D IGMC Shimla, India
*Corresponding Author: Dr Lokesh Singh, Research Associate, Department of Radiodiagnosis, PGIMER, Chandigarh, India
Received: 08 December 2020; Accepted: 04 January 2021; Published: 13 January 2021
Citation: Sandeep Moudgil, Sapna Jangral, Lokesh Singh, Anupam Jhobta. Stroke in Setting of Persistent Trigeminal Artery: Report of Two Cases. Archives of Clinical and Medical Case Reports 5 (2021): 70-74.
View / Download Pdf Share at FacebookAbstract
Persistent trigeminal artery (PTA), commonest among fetal carotid-vertebrobasilar anastomosis encountered in adult life, is an incidental finding but has often been associated with trigemino-cavernous fistula besides cranial nerve palsies, trigeminal neuralgia, hemifacial spasms, intracranial vascular pathologies like aneurysms, arteriovenous malformations posterior circulation, as TIAs or stroke. We present here an acute posterior circulation stroke and a chronic anterior circulation stroke associated with (PTA), in this case report.
Keywords
Stroke; Persistent trigeminal artery
Stroke articles; Persistent trigeminal artery articles
Stroke articles Stroke Research articles Stroke review articles Stroke PubMed articles Stroke PubMed Central articles Stroke 2023 articles Stroke 2024 articles Stroke Scopus articles Stroke impact factor journals Stroke Scopus journals Stroke PubMed journals Stroke medical journals Stroke free journals Stroke best journals Stroke top journals Stroke free medical journals Stroke famous journals Stroke Google Scholar indexed journals Persistent trigeminal artery articles Persistent trigeminal artery Research articles Persistent trigeminal artery review articles Persistent trigeminal artery PubMed articles Persistent trigeminal artery PubMed Central articles Persistent trigeminal artery 2023 articles Persistent trigeminal artery 2024 articles Persistent trigeminal artery Scopus articles Persistent trigeminal artery impact factor journals Persistent trigeminal artery Scopus journals Persistent trigeminal artery PubMed journals Persistent trigeminal artery medical journals Persistent trigeminal artery free journals Persistent trigeminal artery best journals Persistent trigeminal artery top journals Persistent trigeminal artery free medical journals Persistent trigeminal artery famous journals Persistent trigeminal artery Google Scholar indexed journals trigeminal artery articles trigeminal artery Research articles trigeminal artery review articles trigeminal artery PubMed articles trigeminal artery PubMed Central articles trigeminal artery 2023 articles trigeminal artery 2024 articles trigeminal artery Scopus articles trigeminal artery impact factor journals trigeminal artery Scopus journals trigeminal artery PubMed journals trigeminal artery medical journals trigeminal artery free journals trigeminal artery best journals trigeminal artery top journals trigeminal artery free medical journals trigeminal artery famous journals trigeminal artery Google Scholar indexed journals PTA articles PTA Research articles PTA review articles PTA PubMed articles PTA PubMed Central articles PTA 2023 articles PTA 2024 articles PTA Scopus articles PTA impact factor journals PTA Scopus journals PTA PubMed journals PTA medical journals PTA free journals PTA best journals PTA top journals PTA free medical journals PTA famous journals PTA Google Scholar indexed journals carotid-vertebrobasilar articles carotid-vertebrobasilar Research articles carotid-vertebrobasilar review articles carotid-vertebrobasilar PubMed articles carotid-vertebrobasilar PubMed Central articles carotid-vertebrobasilar 2023 articles carotid-vertebrobasilar 2024 articles carotid-vertebrobasilar Scopus articles carotid-vertebrobasilar impact factor journals carotid-vertebrobasilar Scopus journals carotid-vertebrobasilar PubMed journals carotid-vertebrobasilar medical journals carotid-vertebrobasilar free journals carotid-vertebrobasilar best journals carotid-vertebrobasilar top journals carotid-vertebrobasilar free medical journals carotid-vertebrobasilar famous journals carotid-vertebrobasilar Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals Sclerosis articles Sclerosis Research articles Sclerosis review articles Sclerosis PubMed articles Sclerosis PubMed Central articles Sclerosis 2023 articles Sclerosis 2024 articles Sclerosis Scopus articles Sclerosis impact factor journals Sclerosis Scopus journals Sclerosis PubMed journals Sclerosis medical journals Sclerosis free journals Sclerosis best journals Sclerosis top journals Sclerosis free medical journals Sclerosis famous journals Sclerosis Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals SARS-COV-2 articles SARS-COV-2 Research articles SARS-COV-2 review articles SARS-COV-2 PubMed articles SARS-COV-2 PubMed Central articles SARS-COV-2 2023 articles SARS-COV-2 2024 articles SARS-COV-2 Scopus articles SARS-COV-2 impact factor journals SARS-COV-2 Scopus journals SARS-COV-2 PubMed journals SARS-COV-2 medical journals SARS-COV-2 free journals SARS-COV-2 best journals SARS-COV-2 top journals SARS-COV-2 free medical journals SARS-COV-2 famous journals SARS-COV-2 Google Scholar indexed journals tomography articles tomography Research articles tomography review articles tomography PubMed articles tomography PubMed Central articles tomography 2023 articles tomography 2024 articles tomography Scopus articles tomography impact factor journals tomography Scopus journals tomography PubMed journals tomography medical journals tomography free journals tomography best journals tomography top journals tomography free medical journals tomography famous journals tomography Google Scholar indexed journals
Article Details
1. Introduction
Persistent trigeminal artery (PTA), is the commonest embryological carotid-vertebrobasilar anastomosis persisting into adult life. During early embryonic life, trigeminal artery, among others, connects primitive anterior and posterior circulations and shunts blood from primitive cavernous internal carotid artery (ICA), to paired plexiform longitudinal neural arteries, the precursors of vertebral-basilar system, till later develops and takes over the posterior circulation [1, 2]. PTA has an incidence of ~ 0.68% and has been associated with various cranial nerve palsies (e.g. CN III or CN VI), hemifacial spasm, trigeminal neuralgia, subarachnoid hemorrhage, posterior circulation TIA or stroke, intracranial aneurysms or arteriovenous malformations [2-4]. PTA originates from cavernous ICA proximal to the meningohypophysial trunk and terminate by joining mid basilar trunk between the superior cerebellar artery (SCA) and anterior inferior cerebellar artery origins (AICA) [1, 2]. The posterior communicating arteries (PCoMs) and vertebrobasilar system proximal to the communication may be hypoplastic (Saltzman Type A) with PTA serving as a sole source of blood supply to distal basilar artery in such cases and need to be preserved during intervention [2-4].
Emboli originating from ulcerated carotid plaques are known to travel across PTA leading to posterior circulation ischemic stroke. There have also been reports of vertebrobasilar insufficiency (VBI) attributed to PTA. Most of the later cases have concurrent ICA stenosis. We describe here, a patient with posterior cerebral artery occlusion and another patient with infarct in middle cerebral artery territory associated with PTA.
2. Case Reports
2.1 Case 1
A 55-year-old hypertensive female presented with history of loss of bilateral vision loss, right sided weakness and an episode of headache since 7 days. CT head showed ill-defined hypodensity involving the left medial temporal and adjacent medial left parieto-occipital lobe (Figure 1A). Cerebral angiography of head and neck arteries revealed a complete occlusion of the left posterior cerebral artery beyond P1 segment. The basilar artery was supplied by the
right ICA via the PTA (Saltzman type I) (Figure 1B & C). The basilar artery caudal to the basilar top was attenuated in calibre (Figure 1C). Bilateral carotid arteries were tortuous in course, however, no haemodynamically significant stenosis or extracranial or intracranial atherosclerotic changes were observed. Echocardiography shows left ventricular hypertrophy with left ventricular diastolic dysfunction and the etiology was assumed to be a cardioembolic stroke with clot migrating to left PCA from anterior circulation across PTA.
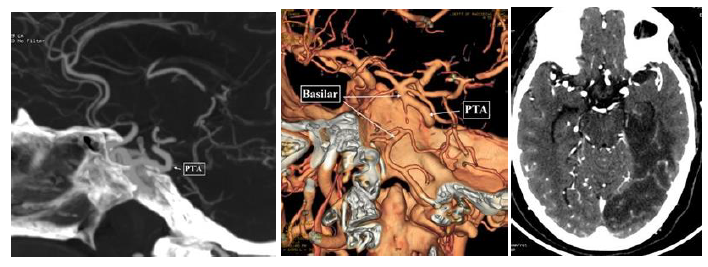
Figure 1: PTA-Acute Stroke: Axial CT head, A) showing hypodensity involving cortex and subcorticular and deep white matter of Left PCA territory; B) PTA was seen (arrow in B) connecting cavernous RICA to basilar artery on Maximum Intensity Projection Coronal view of CT angiograms; C) and on Volume rendered images.
2.2 Case 2
A MRI was done for simple focal right sided seizures followed by headache since last 3 years in a 16 years old female with left sided preference and right sided hemiparesis since birth. Encephalomalacic and gliotic changes with volume loss were seen in the left frontal opercular region and insular region (Figure 2A). MR angiography (TOF) shows fetal origin of right PCA with PTA (Saltzman type IIIa ) and hypoplastic right vertebral and basilar arteries (Figure 2 B, C & D). Left MCA shows paucity of cortical branches. Intracranial portion of bilateral ICA, ACA and right MCA show normal flow related signal.
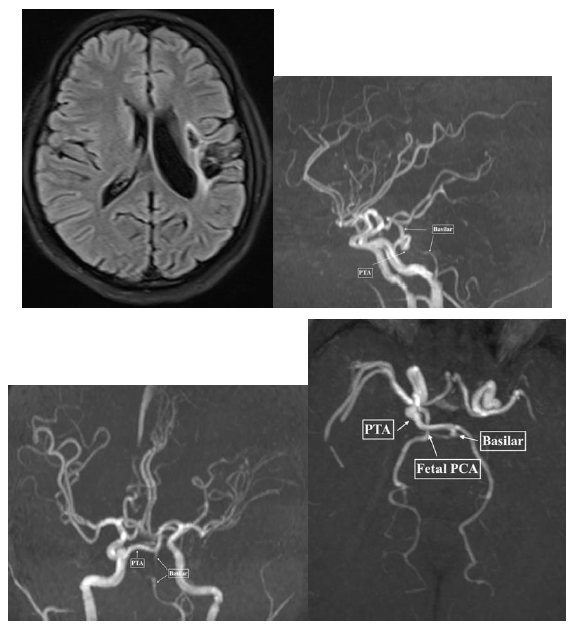
Figure 2: PTA-Chronic Infarct: Axial FLAIR, A) Shows cystic encephalom alacic changes and gliosis in left insular region and frontal operculum, TOF MRA Sagittal; B) Coronal; C) and Axial; D) views demonstrating PTA extending from Cavernous RICA to basilar trunk (arrows).
3. Discussion
During early fetal life, carotid-vertebrobasilar anastomoses connect ICA precursors to paired longitudinal neural arteries and maintains the circulation to hind brain till vertebrobasilar system develops [2, 3]. These regresses subsequently, although their persistence into adult life have been well documented. PTA is, although rare, is most commonly encountered among these persisting vestiges, with a reported incidence of ~0.68% [2-4]. PTA originates from cavernous ICA proximal to the meningohypophysial trunk and terminate by joining mid basilar trunk between the superior cerebellar artery (SCA) and anterior inferior cerebellar artery origins (AICA) [1, 2]. The posterior communicating arteries (PCoMs) and vertebrobasilar system proximal to the communication may be hypoplastic (Saltzman Type A) with PTA serving as a sole source of blood supply to distal basilar artery in such cases and need to be preserved during intervention [2-4]. PTA may not be an important source of posterior circulation when PCoMs and vertebrobasilar system proximal to anastomosis is normal (Saltzman Type 2). At times, PTA may terminate in to SCA, AICA or posterior inferior cerebellar artery (PICA), (Saltzman Type 3a, b and c, respectively) [1, 3-5].
The occurrence ischemic stroke in association with PTA is rarely reported and the role of PTA in ischemic stroke has been poorly understood. Attenuated calibre of proximal basilar artery and bilateral vertebral arteries may have some role to play in posterior circulation stroke. Since PTA shuts the blood from anterior to posterior circulation the boundaries between these two territories are blurred as in first case described above. A thrombus of anterior circulation may freely ‘float’ to posterior circulation across this persistent embryonic conduit. The vast majority of case reports on the role of PTA in the setting of ischemic cerebrovascular disease supported the viewpoint that the existence of PTA may increase the risk of ischemic stroke [6-8]. The compression of pons from the PTA also could cause brainstem transient ischemia stroke [9]. Here we present two cases of supratentorial ischaemic strokes in the setting of PTA, involving PCA territory and cortical branches of MCA territory, both being atypical vascular distributions.
References
- Enomoto T, Sato A, Maki Y. Carotid-cavernous sinus fistula caused by rupture of a primitive trigeminal artery aneurysm. Case report. Journal of Neurosurgery 46 (1997): 373-376.
- Kerber CW, Manke W. Trigeminal artery to cavernous sinus fistula treated by balloon occlusion. Case report. J Neurosurg 58 (1983): 611-613.
- Berger MS, Hosobuchi Y. Cavernous sinus fistula caused by intracavernous rupture of a persistent primitive trigeminal artery. Case report. Journal of Neurosurgery 61 (1984): 391-395.
- Debrun GM, Davis KR, Nauta HJ, et al. Treatment of carotid cavernous fistulae or cavernous aneurysms associated with a persistent trigeminal artery: report of three cases. AJNR Am J Neuroradiol 9 (1988): 749-755.
- Cheng WC, Wang AD. Carotid-cavernous sinus fistula associated with a primitive trigeminal artery. Neurosurgery 27 (1990): 802-805.
- Hiramatsu R, Ohnishi H, Kawabata S, et al. Successful recanalization for internal carotid artery occlusion with persistent primitive trigeminal artery manifesting only as ischemia of the posterior circulation. BMC Neurol 16 (2016): 41.
- Gasecki AP, Fox AJ, Lebrun LH, et al. Bilateral occipital infarctions associated with carotid stenosis in a patient with persistent trigeminal artery. The collaborators of the north American carotid endarterectomy trial (NASCET). Stroke 25 (1994): 1520-1523.
- Schwartz NE, Albers GW. Neurological picture. Acute strokes in the setting of a persistent primitive trigeminal artery. J Neurol Neurosurg Psychiatry 78 (2007): 745.
- Sannegowda RB, Srivastava T, Jain RS, et al. Brainstem transient ischemic attacks due to compression of pons from a persistent primitive trigeminal artery. Neurol India 61 (2013): 321-322.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
