Survival for Ten Years after Aggressive Surgery for Pericardial Recurrent Thymoma with Proton-Beam Radiation Therapy for An Unresectable Intramyocardial Lesion: A Case Report
Article Information
Ryuta Fukai1,2, Yoshihito Irie3, Tetsuo Akimoto4, Keiichi Akasaka5, Kentaro Nakano6
1Department of General Thoracic Surgery, Shonan Kamakura General Hospital, Kamakura, Kanagawa, Japan
2Department of General Thoracic Surgery, Dokkyo Medical University, Mibu, Tochigi, Japan
3Department of Cardiovascular Surgery, Iwaki Kyoritsu General Hospital, Iwaki, Fukushima, Japan
4Department of Radiation Oncology, National Cancer Center Hospital East, Kashiwa, Chiba, Japan
5Department of Respiratory Medicine, Saitama Red Cross Hospital, Saitama, Saitama, Japan
6Department of Respiratory Medicine and Clinical Immunology, Dokkyo Medical University Saitama Medical Center, Koshigaya, Saitama, Japan
*Corresponding Author: Dr. Ryuta Fukai, Department of General Thoracic Surgery, Shonan Kamakura General Hospital, 1370-1 Okamoto, Kamakura, Kanagawa, 247-8533, Japan
Received: 12 August 2020; Accepted: 08 September 2020; Published: 21 September 2020
Citation: Ryuta Fukai, Yoshihito Irie, Tetsuo Akimoto, Keiichi Akasaka, Kentaro Nakano. Survival for Ten Years after Aggressive Surgery for Pericardial Recurrent Thymoma with Proton-Beam Radiation Therapy for An Unresectable Intramyocardial Lesion: A Case Report. Archives of Clinical and Medical Case Reports 4 (2020): 940-945.
View / Download Pdf Share at FacebookAbstract
There is no standard treatment for recurrent thymoma, although complete surgical resection reportedly achieves significantly better survival than other treatments. However, surgical treatment of recurrent thymoma in the pericardium is challenging because of the serious surgical stress and the adverse cardiac effects incurred by opening the pericardial space. We treated a female patient with a recurrence of thymoma 5 years after a complete response to radical radiotherapy. We removed the intrapericardial thymoma under cardiac arrest using an artificial-heart lung apparatus; however, we aborted our attempt to remove another intramyocardial lesion overlapping the left circumflex coronary artery. By 3 years after surgery, the residual intramyocardial tumor had increased in size, so we provided proton-beam radiation therapy. The patient has been well for 10 years after surgery with no sign of recurrence. We should consider aggressive treatment for patients in good general health, even for recurrent thymoma in the pericardium. Proton therapy might be effective for unresectable lesions because it appears to minimize damage to cardiac function.
Keywords
Thymoma; Thymic recurrence; Pericardium; Surgery; Proton therapy
Thymoma articles, Thymic recurrence articles, Pericardium articles, Surgery articles, Proton therapy articles
Thymoma articles Thymoma Research articles Thymoma review articles Thymoma PubMed articles Thymoma PubMed Central articles Thymoma 2023 articles Thymoma 2024 articles Thymoma Scopus articles Thymoma impact factor journals Thymoma Scopus journals Thymoma PubMed journals Thymoma medical journals Thymoma free journals Thymoma best journals Thymoma top journals Thymoma free medical journals Thymoma famous journals Thymoma Google Scholar indexed journals Thymic recurrence articles Thymic recurrence Research articles Thymic recurrence review articles Thymic recurrence PubMed articles Thymic recurrence PubMed Central articles Thymic recurrence 2023 articles Thymic recurrence 2024 articles Thymic recurrence Scopus articles Thymic recurrence impact factor journals Thymic recurrence Scopus journals Thymic recurrence PubMed journals Thymic recurrence medical journals Thymic recurrence free journals Thymic recurrence best journals Thymic recurrence top journals Thymic recurrence free medical journals Thymic recurrence famous journals Thymic recurrence Google Scholar indexed journals Pericardium articles Pericardium Research articles Pericardium review articles Pericardium PubMed articles Pericardium PubMed Central articles Pericardium 2023 articles Pericardium 2024 articles Pericardium Scopus articles Pericardium impact factor journals Pericardium Scopus journals Pericardium PubMed journals Pericardium medical journals Pericardium free journals Pericardium best journals Pericardium top journals Pericardium free medical journals Pericardium famous journals Pericardium Google Scholar indexed journals imaging articles imaging Research articles imaging review articles imaging PubMed articles imaging PubMed Central articles imaging 2023 articles imaging 2024 articles imaging Scopus articles imaging impact factor journals imaging Scopus journals imaging PubMed journals imaging medical journals imaging free journals imaging best journals imaging top journals imaging free medical journals imaging famous journals imaging Google Scholar indexed journals Ultrasonography articles Ultrasonography Research articles Ultrasonography review articles Ultrasonography PubMed articles Ultrasonography PubMed Central articles Ultrasonography 2023 articles Ultrasonography 2024 articles Ultrasonography Scopus articles Ultrasonography impact factor journals Ultrasonography Scopus journals Ultrasonography PubMed journals Ultrasonography medical journals Ultrasonography free journals Ultrasonography best journals Ultrasonography top journals Ultrasonography free medical journals Ultrasonography famous journals Ultrasonography Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals laparoscopy articles laparoscopy Research articles laparoscopy review articles laparoscopy PubMed articles laparoscopy PubMed Central articles laparoscopy 2023 articles laparoscopy 2024 articles laparoscopy Scopus articles laparoscopy impact factor journals laparoscopy Scopus journals laparoscopy PubMed journals laparoscopy medical journals laparoscopy free journals laparoscopy best journals laparoscopy top journals laparoscopy free medical journals laparoscopy famous journals laparoscopy Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Proton therapy articles Proton therapy Research articles Proton therapy review articles Proton therapy PubMed articles Proton therapy PubMed Central articles Proton therapy 2023 articles Proton therapy 2024 articles Proton therapy Scopus articles Proton therapy impact factor journals Proton therapy Scopus journals Proton therapy PubMed journals Proton therapy medical journals Proton therapy free journals Proton therapy best journals Proton therapy top journals Proton therapy free medical journals Proton therapy famous journals Proton therapy Google Scholar indexed journals Recurrent Thymoma articles Recurrent Thymoma Research articles Recurrent Thymoma review articles Recurrent Thymoma PubMed articles Recurrent Thymoma PubMed Central articles Recurrent Thymoma 2023 articles Recurrent Thymoma 2024 articles Recurrent Thymoma Scopus articles Recurrent Thymoma impact factor journals Recurrent Thymoma Scopus journals Recurrent Thymoma PubMed journals Recurrent Thymoma medical journals Recurrent Thymoma free journals Recurrent Thymoma best journals Recurrent Thymoma top journals Recurrent Thymoma free medical journals Recurrent Thymoma famous journals Recurrent Thymoma Google Scholar indexed journals
Article Details
1. Introduction
Thymoma is the most common tumor in the anterior mediastinum, and surgical resection is the most effective treatment, typically achieving long-term survival. Unfortunately, recurrence affects 10% to 30% of patients, from a few months to several years after initial radical resection [1-4]. The best management strategy for recurrent thymoma remains controversial, although some authors report that complete resection of recurrent thymoma yields significantly better survival than subtotal resection or other forms of treatment [5, 6]. While local recurrence is reportedly associated with an excellent prognosis [7], there are no definite surgical indications to guide decision-making. Recommendations for using the extent, location, and number of recurrent lesions, or the general condition of the patient, to guide therapy would be useful. The mediastinum is reportedly the most frequent site of thymoma recurrence, accounting for 18.5% to 27.9% of reported recurrences [5, 8]. Treating recurrence in the pericardium is often difficult because of the sensitive location and the potential adverse cardiac effects of treatment. Cardiac movement disturbs the operative procedure, and radiotherapy is associated with cardiac complications such as pericarditis, myocardial infarction, and congestive heart failure [9, 10]. Proton therapy for thymoma is not yet standard, although it has a lower risk of cardiac toxicity than conventional radiotherapy [11].
We encountered a female patient with thymoma recurrent to the pericardium 5 years after radical radiotherapy. We performed radical resection of the tumor and later provided proton therapy for an unresectable intramyocardial lesion discovered at the time of surgery, with good results.
2. Case Presentation
A 46-year-old woman was referred to us for a recurrent thymoma manifesting with symptoms of myasthenia gravis. Her initial lesion was treated with radiotherapy 5 years prior, with a complete response. The recurrent tumor was located in the pericardium, posterior to the heart (Figure 1).
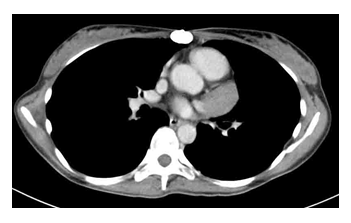
Figure 1: Computed tomography shows a tumor in the pericardium.
We opted for complete resection because the patient was young and in good physical condition, despite the symptoms of myasthenia gravis. Radical resection of the lesion was performed under cardiac arrest with cardiopulmonary bypass. During surgery, we were able to palpate a solid nodule within the cardiac muscle. We were suspicious for another recurrent lesion, but we left the intramyocardial lesion in situ because it overlapped with the left circumflex coronary artery. The resected lesion was examined pathologically, with a final diagnosis of type B2 thymoma according to the World Health Organization classification?system (Figure 2).
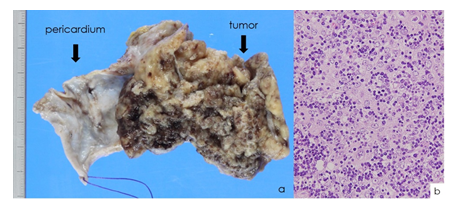
Figure 2: Pathologic examination of the resected specimen. (a) Gross appearance of the tumor and a portion of the pericardium. (b) High-power microscopy.
The patient required artificial respiratory management for 2 weeks after surgery because of complications from myasthenia gravis and a postoperative left pneumothorax. She was discharged on the 43rd postoperative day. The residual intramyocardial lesion was followed for 3 years. When computed tomography showed an increase in size (Figure 3),

Figure 3: Computed tomography 3 years after surgery shows that the residual intramyocardial lesion has increased in size.
She was treated with proton-beam radiation therapy (50 Gy) at National Cancer Center Hospital East. She has required no further treatment, including oral steroids, and has been well for 10 years after surgery, with no signs of myasthenia gravis and no evidence of a recurrent lesion (Figure 4).
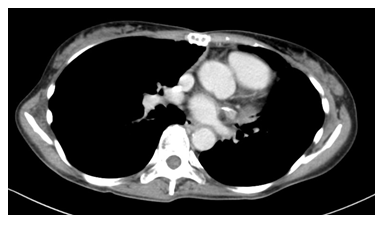
Figure 4: Computed tomography 10 years after surgery shows no sign of recurrence.
Ten years after surgery, echocardiography found no evidence of asynergy at the left ventricular wall, and the ejection fraction was good (77% using the Teichholz formula).
3. Discussion
Many patients with recurrent thymoma experience locoregional recurrence; multimodal aggressive treatment reportedly improves overall survival [5, 6]. We performed radical surgical resection in a patient with recurrent thymoma in the pericardium after radiation therapy 5 years prior. Although we employed cardiac arrest with cardiopulmonary bypass, we were forced to leave behind a second recurrent lesion in the left myocardium because of its sensitive location. The intramyocardial tumor was eventually treated with proton beam radiation therapy, and the patient has been well, without evidence of recurrence, for 10 years after surgery. Ruffini et al report that 10-year survival after the treatment of recurrent thymoma is only 24% [7]. Therefore, intensive multimodal treatment is indicated for localized recurrent thymoma if patients are in a suitable physical condition, even when the lesion is in a sensitive location such as the pericardium.
The treatment of recurrent thymoma varies, and the optimal strategy remains controversial. However, it seems that surgery is the best method for achieving long-term survival when complete resection of the recurrent lesion is possible [5-8]. Margaritora et al note that repeat complete resection yields much better outcomes than partial resection (p < 0.001) [5]. Marulli et al. assessed 82 patients with recurrent thymoma and report that complete surgical resection is associated with significantly better survival than either incomplete resection or nonsurgical treatment (p < 0.0001) [6]. However, resection of a recurrent tumor in the pericardium is typically difficult because of cardiac motion. Ruffini et al note that involvement of the heart, ascending aorta, or main pulmonary artery usually prohibits radical resection [7]. Therefore, we initially considered radiotherapy for our patient. The radiotherapist at our hospital recommended against this tactic, because the additional radiation could increase the risk of cardiac mortality. We then planned for surgery under cardiac arrest because the patient was young, had only a single known lesion, and had no major comorbidities. We were able to successfully treat her recurrent disease, with later proton therapy for an unresectable lesion discovered during surgery.
The use of proton therapy for thymoma is still uncommon; only a few studies report the results of proton therapy for this indication. Vogel and associates describe achieving good local control with proton-beam radiation therapy for adjuvant and definitive treatment of thymoma and thymic carcinoma [10]. It seems that the primary advantage of proton therapy is its low risk of causing damage to mediastinal organs, particularly the heart [11], likely because of its characteristic Bragg peak, even though mediastinal radiation has been shown to increase the long-term risk of death from cardiac disease [12]. Our patient underwent proton therapy 7 years ago for an unresectable lesion and has experienced neither recurrence nor cardiac complications. Proton therapy is not covered by health insurance in Japan, but it should be considered when conventional radiation therapy is deemed risky because of prior radiotherapy.
The mean duration from initial treatment to recurrence in patients with thymoma is between 50 and 92.7 months [5-7, 13]. Therefore, patients require careful follow-up. Margaritora et al assessed 81 patients and found mediastinal relapse in 15 (27.9%) [5]. Sandri et al assessed 81 patients and found mediastinal recurrence in 15 (18.5%) [8]. With mediastinal recurrence being fairly common, clinicians will likely encounter patients with pericardial recurrence. Ruffini et al note that the extent of recurrence is a significant prognostic factor on multivariate survival analysis, and significantly better survival is expected for patients with local recurrent thymoma than those with distant recurrence and pleural dissemination [7]. Surgical resection should be considered for patients with recurrent thymoma in the pericardium, if hematogenous recurrence is absent. Aggressive multimodal treatment is capable of conferring long-term remission, as in our patient.
4. Conclusions
We successfully treated a woman with recurrent thymoma in the pericardium using aggressive surgical resection and subsequent proton therapy for an unresectable intramyocardial lesion. We should consider radical surgery with multimodal therapy for patients with recurrent thymoma who have no evidence of distant recurrence. Proton therapy may be a useful option to avoid putting the mediastinal organs at risk.
Conflicts of Interest
None.
References
- Kirschner PA. Reoperation for thymoma: report of 23 cases. Ann Thorac Surg 49 (1990): 550-555.
- Regnard JF, Magdeleinat P, Dromer C, et al. Prognostic factors and long-term results after thymoma resection: a series of 307 patients. J Thorac Cardiovasc Surg 112 (1996): 376-384.
- Blumberg D, Port JL, Weksler B, et al. Thymoma: a multivariable analysis of factors predicting survival. Ann Thorac Surg 60 (1995): 908-914.
- Maggi G, Casadio C, Cavallo A, et al. Thymoma: results of 241 operated cases. Ann Thorac Surg 51 (1991): 152-156.
- Margaritora S, Cesario A, Cusumano G, et al. Single-centre 40-year results of redo operation for recurrent thymomas. Eur J Cardiothorac Surg 40 (2011): 894-900.
- Marulli G, Margaritora S, Lucci M, et al. Surgical treatment of recurrent thymoma: is it worthwhile? Eur J Cardiothorac Surg 49 (2016): 327-332.
- Ruffini E, Mancuso M, Oliaro A, et al. Recurrence of thymoma: analysis of clinicopathologic features, treatment, and outcome. J Thorac Cardiovasc Surg 113 (1997): 55-63.
- Sandri A, Cusumano G, Lococo F, et al. Long-term results after treatment for recurrent thymoma: a multicenter analysis. J Thorac Oncol 9 (2014): 1796-1804.
- Correa CR, Litt HI, Hwang WT, et al. Coronary artery findings after left-sided compared with right-sided radiation treatment for early-stage breast cancer. J Clin Oncol 25 (2007): 3031-3037.
- Vogel J, Berman AT, Lin L, et al. Prospective study of proton beam radiation therapy for adjuvant and definitive treatment of thymoma and thymic carcinoma: early response and toxicity assessment. Radiother Oncol 118 (2016): 504-509.
- Dabaja BS, Hoppe BS, Plastaras P, et al. Proton therapy for adults with mediastinal lymphomas: the International Lymphoma Radiation Oncology Group guidelines. Blood 132 (2018): 1635-1646.
- Preston DL, Shimizu Y, Pierce DA, et al. Studies of mortality of atomic bomb survivors. Report 13: solid cancer and noncancer disease mortality: 1950-1997. 2003. 178 (2012): AV146-172.
- Fiorelli A, D’Andrilli A, Vanni C, et al. Iterative surgical treatment for repeated recurrences after complete resection of thymic tumors. Ann Thorac Surg 103 (2017): 422-431.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
