The Role of Dispatcher Assisted Cardiopulmonary Resuscitation in Out-Of-Hospital Cardiac Arrest: A Systematic Review and Meta- Analysis
Article Information
Yu Wang1, Abhijit Adhikary2 and Hong Zhang1
1Department of Emergency Medicine, The First Affiliated Hospital of Anhui Medical University, Hefei City, Anhui Province, China
2Department of Emergency Medicine, EMS and HEMS, Nepal Mediciti Hospital, Nepal
*Corresponding author: Hong Zhang, Department of Emergency Medicine, The First Affiliated Hospital of Anhui Medical University, Hefei City, Anhui Province, China
Received: 14 December 2019; Accepted: 19 December 2019; Published: 02 January 2020
Citation: Yu Wang, Abhijit Adhikary and Hong Zhang. The Role of Dispatcher Assisted Cardiopulmonary Resuscitation in Out-Of-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. Cardiology and Cardiovascular Medicine 4 (2020): 009-020.
View / Download Pdf Share at FacebookAbstract
Objectives The role of Dispatcher Assisted Cardiopulmonary Resuscitation (DACPR) has not been widely reported. The objectives of the study were to perform a systematic review and meta-analysis of observational studies addressing whether DACPR, compared with independent Bystander Cardiopulmonary Resuscitation (BCPR), increased the rates of BCPR, and whether they altered survival outcomes compared with no BCPR in Out-of-hospital Cardiac Arrest (OHCA).
Methods We searched the relevant articles from PubMed and Cochrane databases. The basic information and outcome data (BCPR rates, survival to hospital discharge, 1-month survival) were extracted from the included studies. Meta-analyses were performed by using STATA 11.0 software.
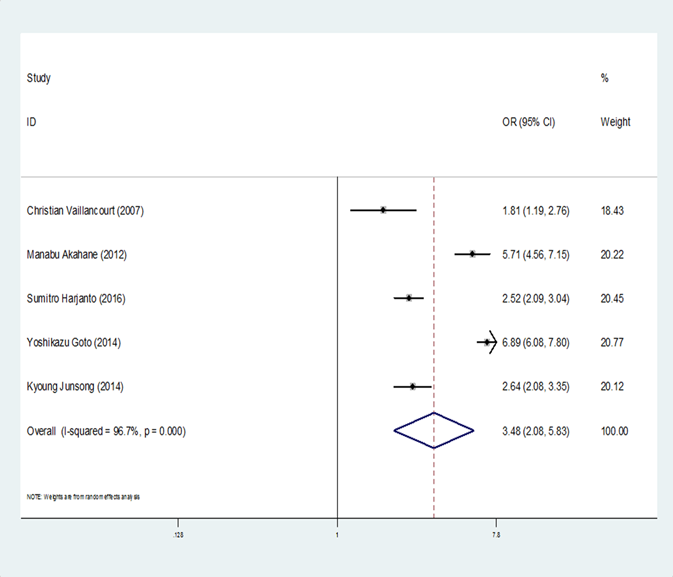
Results Eight studies involving 65,148 patients were eligible. Overall meta-analysis showed that DACPR was associated with statistically improved rates of BCPR (Odds Ratio [OR] =3.48, 95% confidence interval[CI]: 2.08-5.83, I2= 96.7%), and survival to discharge/ 1-month survival (OR=1.51, 95%CI: 1.40- 1.63, I2= 24.9%) when compared with no BCPR. However, no significant effect of DACPR in survival rate was found, when compared with independent BCPR (OR=0.84, 95% CI: 0.62-1.14, I2 = 88.6%).
Conclusion This study found that DACPR resulted in significantly higher rates of BCPR as compared with independent BCPR in OHCAs. Considering that DACPR also resulted in greater survival rate compared with no BCPR, DACPR should be a standard protocol for EMS systems worldwide.
Keywords
Cardiopulmonary Resuscitation; Dispatcher Assisted Cardiopulmonary Resuscitation; Bystander Cardiopulmonary Resuscitation; Out-of-hospital Cardiac Arrest
Cardiopulmonary Resuscitation articles, Dispatcher Assisted Cardiopulmonary Resuscitation articles, Bystander Cardiopulmonary Resuscitation articles, Out-of-hospital Cardiac Arrest articles.
Article Details
Introduction
Cardiac arrest (CA) is the leading cause of death worldwide. OHCA has high incidence and low survival rate, and is the serious public issue [1]. Early cardiopulmonary resuscitation is the most effective measure to improve the prognosis of patients with cardiac arrest [2]. The introduction and development of the concept of emergency medical services (EMS) has played a crucial role in decreasing mortality rates and returning to survival in OHCA [3].
The American Heart Association first included DACPR in its guidelines for cardiopulmonary resuscitation In 2015 [4], and it was strongly recommended that dispatchers instruct callers to perform simple chest compression on suspected OHCA adults in 2017 [5]. DACPR is mainly based on the Medical Priority Dispatch System (MPDS) developed by the International Academies of Emergency Dispatch (IAED), which has been widely used in emergency command centers in the United States, Britain and other countries.
A well-established EMS system has been set and greater awareness of regarding CA as well as cardio-pulmonary resuscitation (CPR) knowledge are among the general public and communities in North America and Europe. As a result, they may have a higher rate of BCPR and survival outcomes compared with Asia. One of the main differences in the EMS systems in most of the Asian countries and the western countries is the greater incidence of bystander initiated CPR and the availability of dispatcher assistance for bystanders. This can be invaluable in cases like CA where the prompt initiation of CPR might be the difference between life and death. However, the role of DACPR has not been widely reported, especially in the least developed countries and developing countries.
Methods
We performed a meta-analysis of observational studies to address whether DACPR compared with independent BCPR increased the rates of BCPR in OHCAs, and to determine if in patients with OHCA, the provision of DACPR as opposed to independent BCPR and no BCRP improved survival outcome.
Sources and Search strategy
This systematic review and meta-analysis was based on published articles in related topic from January 1980 to February 2017. The terms ‘dispatcher’, ‘out of hospital’, ‘cardiac arrest’, ‘cardiopulmonary resuscitation’, ‘bystander’, and ‘CPR’ were used to search the PubMed database. The Cochrane database of systematic reviews was searched using the terms ‘cardiopulmonary resuscitation’ and ‘dispatcher’. Further search using the terms ‘Asia’, ‘Africa’, ‘Australia’, ‘Middle East’ was done to ensure coverage of all the regions. Names of some of the countries where dispatcher assistance for CPR is provided, i.e. ‘United States’, ‘Canada’, as well as the PAROS nations ‘Singapore’, ‘South Korea’, ‘Malaysia’, ‘Thailand’, ‘Singapore’, ‘UAE’ and ‘Japan’ were also specified in the search parameters to prevent omission of articles. ‘China’ was used as a keyword to identify native Chinese studies. The search was limited to publications in English and in humans.
Eligibility
The inclusion criteria were as follows:
- Population: both pediatric and adult population suffering an OHCA (defined as receiving chest compressions and/or defibrillation)
- Study types: all studies reporting the primary outcome measure were eligible.
- Intervention or comparison: the study reported intervention of DACPR?independent BCPR and/or no BCPR
- Outcome measure: articles with comparative study of DACPR, independent BCPR or no BCPR with parameters being of either rate or survival or both were selected for this study.
The exclusion criteria were as follows:
- Articles with no information on the size of the study population or with inconsistencies
- Studies that were subgroup reports and reviews
- Primary outcome was not reported.
- Non-English language studies.
Article Selection and data extraction
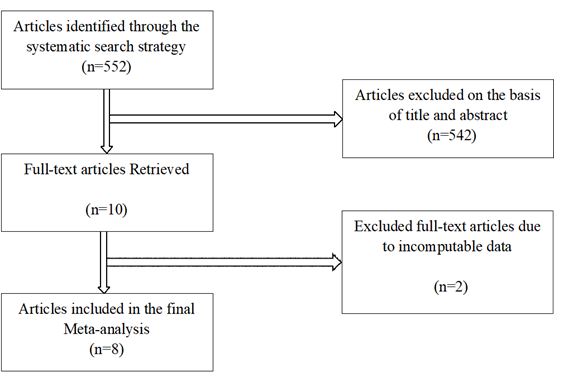
All articles were screened independently by two review authors to identify studies that potentially met the inclusion criteria outlined above. The full text of potentially eligible studies was retrieved and independently assessed for eligibility by two review team members. Any disagreement over the eligibility of particular studies was resolved by discussion with a third reviewer. Afterward, the following data was extracted independently using standardized data extraction forms: the first author’s name, time point, country, sample size, study population, comparisions, study type and end point (Figure1).
Outcome Measures
The primary outcome was the rate of CPR (defined as initiation of CPR in out-of-hospital setting) by bystanders;
For the effect of dispatcher assistance on survival of the patient, the primary outcomes of the study were:
- Survival till discharge from the hospital.
- 1 month survival, irrespective of the neurological outcome.
We originally intended to include survival till discharge from the hospital as the only primary outcome, but the paucity of data and lack of uniformity of outcome parameters in published articles compelled us to add other survival outcomes as the primary outcome. Survival till hospital discharge has been taken as the survival indicator wherever available, while 1 month survival has been taken as the survival indicator in the rest.
Risk of bias (quality) assessment
The Newcastle-Ottawa Scale was used to assess the quality of included Prospective cohort studies [6]. The Agency for Healthcare Research and Quality (AHRQ) was used to assess the quality of cross-sectional studies and retrospective before-after studies [7]. The assessed quality of included studies was shown in Table 1.
|
Article Author |
Time point |
Country |
Sample size |
Study Population |
Comparisons |
Study type |
End Point |
Quality |
|
Kyoung JunSong[4] |
2009-2012 |
South Korea |
8144 |
>15 years |
DI vs. No DI |
Retrospective before-after |
Hospital Discharge |
High |
|
Thomas D. Rea[8] |
1983-2000 |
USA |
7265 |
≥18 years |
DACPR vs. BCPR/No CPR |
Prospective cohort |
Hospital Discharge |
High |
|
Christian Vaillancourt[9] |
2003-2004 |
Canada |
529 |
>16 years |
DI vs. No DI |
Retrospective before-after |
Hospital Discharge |
High |
|
Manabu Akahane[10] |
2005-2008 |
Japan |
1780 |
<20 years |
DI vs. No DI |
Retrospective cohort |
1 month survival |
High |
|
Yoshikazu Goto[11] |
2008-2010 |
Japan |
5009 |
<18 years |
DI vs. No DI; DACPR vs. BCPR/No CPR |
Prospective cohort |
1 month survival |
High |
|
Young Sun Ro[12] |
2012-2014 |
South Korea |
1529 |
<18 years |
DACPR vs. BCPR/No CPR |
Cross-sectional study |
Hospital Discharge |
High |
|
Sumitro Harjanto[13] |
2010-2013 |
Singapore |
2968 |
Child and Adult |
DI vs. No DI; DA-BCPR vs. No DACPR/No CPR |
Retrospective before-after |
1 month survival |
Low |
|
Young Sun Ro[14] |
2012-2013 |
South Korea |
37924 |
≥18years |
DACPR vs. BCPR/No CPR |
Cross-sectional study |
Hospital Discharge |
High |
Table 1: Characteristics of selected studies.
DI: Dispatcher Assisted Cardiopulmonary Resuscitation intervention; BCPR: Bystander Cardiopulmonary Resuscitation; CPR: Cardiopulmonary Resuscitation; DACPR: Dispatcher Assisted Cardiopulmonary Resuscitation; DA-BCPR: Dispatcher Assisted Bystander Cardiopulmonary Resuscitation
Statistical Analysis
All statistical analyses of this meta-analysis were performed using STATA 11.0 software (Stata-Corp, College Station, TX, USA). Pooled odds ratios (ORs) and 95% confidence intervals (95%CI) were calculated by comparing DACPR group, independent BCPR group and no BCPR group. The heterogeneity was measured using the Q-test and statistics, and forest plots were produced using the fixed-effect model when the P-value of the Q-test more than 0.10 and I2 value was less than 50%, otherwise, the random-effect model was used. Subgroup analyses were also performed by ethnicity, population and study type, to find the potential source of high heterogeneity between various studies. The sensitivity analysis was enforced by sequential omission of individual studies. Begg’s rank regression and Egger’s weighted regression were used to estimate potential publication bias, and P value less than 0.05 indicated significance of publication bias.
Results
Literature search and selection
Initially, abstracts of the collected articles were studied. A total of 552 articles reporting OHCA cases with pre-hospital intervention were further analyzed. Finally, articles with comparative study of DACPR, independent BCPR or no BCPR with parameters being of either rate of CPR or survival or both were selected for this study, resulting in inclusion of data from 8 original articles for the purpose of this analysis. 2 studies were from North America (1 from Canada and 1 from The United States) and 6 from Asia (3 from South Korea, 2 from Japan and 1 from Singapore). There was no eligible research of DACPR in any of the countries in Africa and South America.
Characteristics of included studies
The characteristics of the relevant studies with their interventions, population, the results of the quality assessment and outcome measures were presented in Table 1. All the included studies were observational studies, including 1 retrospective cohort study, 2 prospective cohort studies, 3 retrospective before-after studies and 2 cross-sectional studies. The duration of follow-up ranged from 1 month to 1 year. Of the 8 included studies, 2 were conducted in the adult population [8,14], 2 were conducted in the pediatric population [11,12]. With respect to overall risk of bias, 1 study was deemed at low quality assessment, 7 were at high quality assessment. All details of the characteristics of included studies were shown in Table 1.
BCPR rate
5 of the eligible 8 studies compared the rate of administration of CPR by bystanders in DACPR and independent BCPR groups [3, 9, 10, 11, 13] (Table 2). They were conducted in Canada, South Korea, Japan and Singapore. The overall meta-analysis showed that DACPR was associated with statistically increased rate of BCPR when compared with independent BCPR?OR=3.48, 95% CI,: 2.08-5.83,: I2=96.7%) (Figure 2). DACPR in Children was more likely to result in higher rate of BCPR when compared with independent BCPR (OR= 6.89, 95% CI: 6.08-7.80, I2=96.7%). Meanwhile, significantly increased rate of BCPR in the DACPR group compared with independent BCPR group was observed in prospective cohort studies (OR=6.89, 95% CI: 6.08-7.80). Asians had higher rate of BCPR in DACPR(OR=4.03, 95% CI: 2.33-6.98, I2=97.1%) compared with independent BCPR than Caucasians (OR=1.81, 95% CI: 1.19-2.76) (Table 2).
|
Comparison of survival rate |
Group |
Number of study |
Significance |
Heterogeneity |
Publication bias |
||||
|
OR |
95%CI |
P value |
I2(%) |
P value |
P (Begg) |
P(Egger) |
|||
|
DACPR Vs In BCPR |
Overall |
5 |
3.48 |
2.08-5.83 |
<0.001 |
96.7 |
<0.001 |
0.624 |
0.167 |
|
Study type |
|||||||||
|
Prospective cohort [11] |
1 |
6.89 |
6.08-7.80 |
<0.001 |
-- |
-- |
-- |
-- |
|
|
Retrospective [4,9,10,13] |
4 |
2.93 |
1.85-4.63 |
<0.001 |
92.7 |
<0.001 |
1.000 |
0.742 |
|
|
Population |
|||||||||
|
Children [11] |
1 |
6.89 |
6.08-7.80 |
<0.001 |
-- |
-- |
-- |
-- |
|
|
Mixed [4,9,10,13] |
4 |
2.93 |
1.85-4.63 |
<0.001 |
92.7 |
<0.001 |
1.000 |
0.742 |
|
|
Ethnicity |
|||||||||
|
Caucasians [9] |
1 |
1.81 |
1.19-2.76 |
0.006 |
-- |
-- |
-- |
-- |
|
|
Asians [4,10,11,13] |
4 |
4.03 |
2.33-6.98 |
<0.001 |
97.1 |
<0.001 |
0.497 |
0.302 |
|
Table 2: Results of meta-analysis of CPR rate.
CPR: Cardiopulmonary Resuscitation; DACPR: Dispatcher Assisted Cardiopulmonary Resuscitation; In BCPR: Independent Bystander Cardiopulmonary Resuscitation; OR: Odds Ratio; CI: Confidence Interval
Survival rate
Overall, there was a statistically significant advantage for the DACPR group when compared with no BCPR group (OR=1.51, 95%CI: 1.40-1.63.I2=24.9%), the similar results were shown in adults (OR=1.51, 95%CI: 1.39-1.64, I2=0) and children (OR=1.54, 95%CI: 1.28-1.85, I2=71.8%) (Table 3). Independent BCPR group was significant associated with improved survival when compared with no BCPR group (OR=1.97, 95%CI: 1.81-2.14, I2=47.9%). However, there was no difference in survival rate when DACPR group was compared with independent BCPR group (OR=0.84, 95% CI: 0.62-1.14, I2=88.6%).
|
Comparison of survival rate |
Group |
Number of studies |
Significance |
Heterogeneity |
Publication bias |
||||
|
OR |
95%CI |
P value |
I2(%) |
P value |
P (Begg) |
P(Egger) |
|||
|
DACPR Vs No BCPR |
Overall |
5 |
1.51 |
1.40-1.63 |
<0.001 |
24.9 |
0.256 |
1.000 |
0.954 |
|
Study type |
|||||||||
|
Prospective cohort [8][11] |
2 |
1.41 |
1.24-1.61 |
<0.001 |
0 |
0.928 |
0.317 |
-- |
|
|
Cross-sectional study [12][14] |
2 |
1.57 |
1.43-1.72 |
<0.001 |
64.3 |
0.094 |
0.317 |
-- |
|
|
Retrospective before-after [13] |
1 |
0.61 |
0.08-4.47 |
0.626 |
-- |
-- |
-- |
-- |
|
|
Population |
|||||||||
|
Adults [8][14] |
2 |
1.51 |
1.39-1.64 |
<0.001 |
0 |
0.331 |
0.317 |
-- |
|
|
Children [11][12] |
2 |
1.54 |
1.28-1.85 |
<0.001 |
71.8 |
0.059 |
0.317 |
-- |
|
|
Mixed [13] |
1 |
0.61 |
0.08-4.47 |
0.626 |
-- |
-- |
-- |
-- |
|
|
Ethnicity |
|||||||||
|
Caucasians [8] |
1 |
1.41 |
1.19-1.66 |
<0.001 |
|||||
|
Asians [11,12,13,14] |
4 |
1.54 |
1.42-1.68 |
<0.001 |
31.7 |
0.222 |
0.497 |
0.965 |
|
|
In BCPR Vs No BCPR |
Overall |
5 |
1.97 |
1.81-2.14 |
<0.001 |
47.9 |
0.104 |
0.142 |
0.206 |
|
Study type |
|||||||||
|
Prospective cohort [8][11] |
2 |
2.09 |
1.84-2.38 |
<0.001 |
0 |
0.469 |
0.317 |
-- |
|
|
Cross-sectional study [12][14] |
2 |
1.86 |
1.66-2.08 |
<0.001 |
81.7 |
0.022 |
0.317 |
-- |
|
|
Retrospective before-after [13] |
1 |
2.07 |
1.41-3.02 |
<0.001 |
-- |
-- |
-- |
-- |
|
|
Population |
|||||||||
|
Adults [8][14] |
2 |
1.94 |
1.77-2.12 |
<0.001 |
69.4 |
0.071 |
0.317 |
-- |
|
|
Children [11] [12] |
2 |
2.14 |
1.71-2.69 |
<0.001 |
72.1 |
0.058 |
0.317 |
-- |
|
|
Mixed [13] |
1 |
2.07 |
1.41-3.02 |
<0.001 |
-- |
-- |
-- |
-- |
|
|
Ethnicity |
|||||||||
|
Caucasians [8] |
1 |
2.15 |
1.85-2.50 |
<0.001 |
|||||
|
Asians [11,12,13,14] |
4 |
1.88 |
1.71-2.08 |
<0.001 |
46.3 |
0.133 |
0.089 |
0.135 |
|
|
DACPR Vs In BCPR |
Overall |
6 |
0.84 |
0.62-1.14 |
0.265 |
88.6 |
<0.001 |
0.851 |
0.987 |
|
Study type |
|||||||||
|
Prospective cohort [8][11] |
2 |
0.68 |
0.59-0.78 |
<0.001 |
0 |
0.423 |
0.317 |
-- |
|
|
Cross-sectional study [12][14] |
2 |
0.75 |
0.52-1.09 |
0.131 |
61.2 |
0.109 |
0.317 |
-- |
|
|
Retrospective before-after [10][13] |
2 |
0.97 |
0.17-5.54 |
0.973 |
69.3 |
0.071 |
0.317 |
-- |
|
|
Population |
|||||||||
|
Adults [8][14] |
2 |
0.75 |
0.58-0.98 |
0.036 |
85.5 |
0.009 |
0.317 |
-- |
|
|
Children [11][12] |
2 |
0.70 |
0.56-0.87 |
0.002 |
0 |
0.351 |
0.317 |
-- |
|
|
Mixed [10][13] |
2 |
0.97 |
0.17-5.54 |
0.973 |
69.3 |
0.071 |
0.317 |
-- |
|
|
Ethnicity |
|||||||||
|
Caucasians [8] |
1 |
0.65 |
0.56-0.77 |
<0.001 |
-- |
-- |
-- |
-- |
|
|
? |
Asians [10,11,12,13,14] |
5 |
0.89 |
0.60-1.32 |
0.556 |
87.9 |
<0.001 |
1.000 |
0.943 |
Table 3: Results of meta-analysis of survival rate.
DACPR: Dispatcher Assisted Cardiopulmonary Resuscitation; BCPR: Bystander Cardiopulmonary Resuscitation; In BCPR: Independent Bystander Cardiopulmonary Resuscitation; OR: Odds Ratio; CI: Confidence Interval
Publication bias and sensitivity analysis
To assess the stability of the results, sensitivity analysis was conducted by excluding each study sequentially. And the results showed that no study obviously affected the pooled OR, which indicated that the results of meta-analyses were stable. There was no evidence of publication bias according to Begg’s test and Egger’s test.
Discussion
Dispatcher assistance in CPR instructions for OHCAs was not a novel concept. The provision for CPR instructions by the EMS dispatcher was first conceived in 1970s. Our study found that there was significant difference in rate of BCPR between the DACPR group and the independent BCPR group, and DACPR was associated with statistically increased rate of BCPR. Meanwhile there was a significant advantage in survival rate for the DACPR group when compared with no BCPR group. DACPR was found to be effective in getting previously untrained persons to initiate CPR and also in increasing rates of bystander CPR in early stages of its implementation [9]. Dispatchers are able to identify CA as well as the necessity to initiate CPR and this has been shown to be directly related to positive mortality outcomes [15].
While the application of EMS system has not been popularized all over the world, our analysis found DACPR and independent BCPR were significant associated with improved survival when compared with no BCPR group in Asians and Caucasians. The systematic review published in 2010 found that the percentage of VF and survival to discharge rates in Asia were lower (11% and 2%, respectively) than those in Europe (35% and 9%, respectively), North America (28% and 6%, respectively), or Australia (40% and 11%, respectively) (P < 0.001, P < 0.001) [16]. However, we found there was similar results of survival rate in Asians (OR=1.54, 95%CI: 1.42-1.68) and Caucasians (OR=1.41, 95%CI: 1.19-1.66) when DACPR group was compared with no BCPR group. The data in our study extracted from developed Asian countries with perfect EMS systems may result the high survival of OHCAs. But many developing countries and least developed countries have insufficient coverage of EMS systems and lack DACPR studies in Africa and South America, where people's health and medical environment still need to be expanded and improved.
Previous studies showed BCPR drastically increased the chances of survival in out-of-hospital settings [17, 18, 19]. A recent review and meta-analysis draw a conclusion that the provision of DACPR compared with no DACPR was consistently associated with improved outcome across all analyses and comparison of DACPR to bystander CPR produced conflicting results [20]. Our result also showed there was no difference in survival of DACPR compared with independent BCPR. That may be explained by multiple factors. First, the barriers encountered in performing DACPR, such as language barrier, unwillingness of the bystander, limitation of the location, etc. may lead to delay to initial CPR and negative effect in survival. Second, there is also the difference in the quality of CPR when dispatchers provide instruction on how to perform CPR, even for someone performing CPR for the first time [12]. The quality of BCPR as well as the interval from collapse to CPR have been associated with survival in OHCA. Thus, DACPR is theoretically as well as practically preferable to independent BCPR. Therefore, EMS systems should improve training dispatchers for assistance in CPR, people need to be continuously trained about basic medical knowledge and CPR with DACPR instruction so as to initial early BCPR in OHCA and improve survival rate.
Limitations
It is also the case that, we have limitations in our analysis. First, there is no eligible research of dispatcher assistance for CPR in any of the countries in Africa and South America, Our data are based on 8 studies from a total of 552 articles in Caucasians and Asians. Therefore, the study does not reflect the role of BCPR in OHCAs worldwide and we have missed the opportunity to present more complete data on outcomes by restricting eligibility to studies reporting BCPR rate or the survival of DACPR. Second, different countries and EMS systems with different dispatchers instruction protocol are included. Furthermore, they span a period of 37 years and interventions of EMS have changed significantly. Third, the studies which comprise this analysis are largely reports based on retrospective data (6/8). More prospective data collection should be done according to a standardized set of variables and outcome measures. This would enhance the quality of published data and permit comparison across varied settings.
Conclusion
In conclusion, DACPR was associated with a statistically increased rate of BCPR compared with Independent BCPR, meanwhile DACPR resulted in the greater survival rate as compared with no BCPR in OHCAs. DACPR should be a standard protocol for EMS systems worldwide and easy to be followed. It is important to emphasize that further studies need to be conducted to come to a definite conclusion regarding the effectiveness survival benefits of DACPR compared with Independent BCPR. It requires high quality prospective epidemiological studies to provide a sound footing for measures to improve outcomes in this most critical of populations.
References
- McNally B, Robb R, Mehta M, et al. Out-of-hospital cardiac arrest surveillance—Cardiac Arrest Registry to Enhance Survival (CARES),United States, October 1, 2005–December 31, 2010. MMWR Surveill Summ 60 (2011): 1-19.
- Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation 128 (2013): 417-435.
- Song KJ, Shin SD, Park CB, Kim JY, Kim DK, Kim CH, et al. Dispatcher-assisted bystander cardiopulmonary resuscitation in a metropolitan city: A before–after population-based study. Resuscitation 85 (2014): 34–41.
- Travers AH, Perkins GD, Berg RA, et al. Adult basic life support and automated external defibrillation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 132 (2015): S51-83.
- Monica E. Kleinman, Zachary D. Goldberger, Thomas Rea, Robert A. Swor, Bentley J. Bobrow, 2017 American Heart Association Focused Update on Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, Circulation137 (2018): e14.
- GA Wells, B Shea, D O'Connell, J Peterson, V Welch, M Losos, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses, ohri.ca/programs/clinical_epidemiology/oxford.htm (2008, accessed 16 January 2018).
- Rostom A, Dube C, Cranney A, et al. Celiac Disease. Rockville(MD): Agency for Healthcare Research and Quality(US); 2004 sep. (Eidence Rport/Tchnology Asessment, No.104) Appendix D. Quality assessment Forms. Available from: http://www.ncbi.nlm.nih.gov/books/NBK35156/
- Rea TD, Eisenberg MS, Culley LL, Becker L. Dispatcher-assisted cardiopulmonary resuscitation and survival in cardiac arrest. Circulation 104 (2001): 2513–2516.
- Vaillancourt C, Verma A, Trickett J, Crete D, Beaudoin T, Nesbitt L, et al. Evaluating the effectiveness of dispatch assisted cardiopulmonary resuscitation instructions. Acad Emerg Med 14 (2007): 877–883.
- Akahane M, Ogawa T, Tanabe S, Koike S, Horiguchi H, Yasunaga H, et al. Impact of telephone dispatcher assistance on the outcomes of pediatric out-of-hospital cardiac arrest. Crit Care Med 40 (2012): 1410-1416.
- Goto Y, Maeda T, Goto Y. Impact of Dispatcher-Assisted Bystander Cardiopulmonary Resuscitation on Neurological Outcomes in Children With Out-of-Hospital Cardiac Arrests: A Prospective, Nationwide, Population-Based Cohort Study. J Am Heart Assoc 3 (2014): e000499.
- Ro YS, Song KJ, Shin SD, Hong KJ, Ahn KO, Kim DK, et al. Effects of Dispatcher-assisted Cardiopulmonary Resuscitation on Survival Outcomes in Infants, Children, and Adolescents with Out-of-hospital Cardiac Arrests. Resuscitation 108 (2016): 20–26.
- Harjanto S, Na MXB, Hao Y, Ng YY, Goh ES, Leong BSH, et al. A before–after interventional trial of dispatcher-assisted cardio-pulmonary resuscitation for out-of-hospital cardiac arrests in Singapore. Resuscitation 102 (2016): 85–93.
- Ro YS, Shin SD, Lee YJ, Lee SC, Song KJ, Ryoo HW, et al. Effect of Dispatcher-Assisted Cardiopulmonary Resuscitation Program and Location of Out-of-Hospital Cardiac Arrest on Survival and Neurologic Outcome. Ann Emerg Med 69 (2017): 52-61.
- Kuisma M, Boyd J, Väyrynen T, Repo J, Nousila-Wiik M, Holmstr¨om P. Emergency call processing and survival from out-of-hospital ventricular fibrillation. Resuscitation 67 (2005): 89–93.
- Berdowskia J, Bergb RA, Tijssena JGP, Kostera RW. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 81 (2010): 1479–1487.
- Waalewijn RA, de Vos R, Koster RW. Out-of-hospital cardiac arrests in Amsterdam and its surrounding areas: results from the Amsterdam resuscitation study (ARREST) in ‘Utstein’ style. Resuscitation 38 (1998): 157–167.
- Holmberg M, Holmberg S, Herlitz J. Effect of bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest patients in Sweden. Resuscitation 47 (2000): 59–70.
- Herlitz J, Engdahl J, Svensson L, Angquist KA, Young M, Holmberg S, et al. Factors associated with an increased chance of survival among patients suffering from an out-of-hospital cardiac arrest in a national perspective in Sweden. Am Heart J 149 (2005): 61–66.
- Nikolaou N, Dainty KN, Couper K, Morley P, Tijssen J, Vaillancourt C. A systematic review and meta-analysis of the effect of dispatcher-assisted CPR on outcomes from sudden cardiac arrest in adults and children. Resuscitation 138 (2019): 82–105.


 Impact Factor: * 3.5
Impact Factor: * 3.5 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 14.80%
Acceptance Rate: 14.80%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 