Watching, Reading and Don’t See-Lung surgery: A Case Report
Article Information
Gualtieri E1*, Piccolo A1*, Adducci E1*, Beccia G1, Iacobucci T1, Nachira D2, Congedo MT2, Iaffaldano A2, Pogliani L2, Zanfrini E2, Ferretti G2, Margaritora S2, Sollazzi L1
1Department of Anesthesia and Intensive Care, Catholic University, Rome, Italy
2Department of General Thoracic Surgery, Catholic University, Rome, Italy
*Corresponding Authors: Gualtieri Elisabetta, Department of Anesthesia and Intensive Care, Catholic University, Rome, Italy
Piccolo Annalisa, Department of Anesthesia and Intensive Care, Catholic University, Rome, Italy
Adducci Enrica, Department of Anesthesia and Intensive Care, Catholic University, Rome, Italy
Received: 13 September 2019; Accepted: 30 September 2019; Published: 07 October 2019
Citation: Gualtieri E, Piccolo A, Adducci E, Beccia G, Iacobucci T, Nachira D, Congedo MT, Iaffaldano A, Pogliani L, Zanfrini E, Ferretti G, Margaritora S, Sollazzi L. Watching, Reading and Don’t See-Lung surgery: A Case Report. Journal of Surgery and Research 2 (2019): 231-234.
View / Download Pdf Share at FacebookAbstract
Incorrect preoperative evaluation can lead to some problems in anesthesiologic management, particularly in thoracic anesthesia. We present the case of an old man with a history of adenocarcinoma of the rectum, diagnosed with a solid pulmonary nodule. The thoracic surgery team scheduled an Uniportal Video-Assisted Thoracoscopy (U-VATS) atypical resection of the right lower lobe. Intraoperative airway management was complicated by the unexpected presence of a tracheal diverticulum, a rare pathological issue that can cause many difficulties in airways management Mastery of the bronchoscopy technique by experienced anesthesiologists and their knowledge of alternative choices for pulmonary exclusion, allowed to choose an alternative for the one lung ventilation, without causing any harm to the patient. Correct handling of the bronchoscope is a gold standard tool for modern anesthesiologist. It is also mandatory, from our point of view, to examine diagnostic images with a critical eye, looking for those details that could make the difference on anesthesiologic management of the patients.
Keywords
One lung ventilation (OLV), Tracheal diverticulum, Bronchoscopy
Article Details
1. Introduction
Thoracic anesthesia presents special risks, due to patient morbidities and the complexity of both the surgical and anesthesia care required. Management of thoracic cases can be challenging and incorrect preoperative evaluation of the patient can lead to difficult airways management and can cause iatrogenic injuries.
2. Case Report
We present the case of a 72-years old man with a history of adenocarcinoma of the rectum (pT4, N0, M0) treated with surgery and adjuvant chemotherapy in 2007, who was diagnosed with a solitary solid pulmonary nodule at a follow-up CT scan in April 2018. The nodule was located in the apical segment of the right lower lobe, had a size of 16 × 10 mm, irregular and spiculated margins and signs of pleural retraction. The successive 18-Fluorine fluorodeoxyglucose (18F-FDG) Positron Emission Tomography-Computed Tomography (PET-CT) scan highlighted an increased radiotracer uptake in correspondence with the pulmonary nodule, and no other relevant findings. The patient was therefore referred to our thoracic surgery department. Clinical anamnesis revealed presence of hypertension, abdominal aortic aneurysm (49 × 45 mm), Mediterranean anemia, cerebrovascular disease, left (50%) and right (40%) internal carotid stenosis and chronic kidney disease. A multidisciplinary evaluation of the case decided upon performing a surgical intervention to remove the nodule.
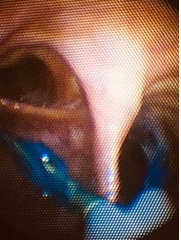
Pre-operative physical examination and routine laboratory tests had results within the normal ranges. A spirometric test diagnosed a mild chronic obstructive pulmonary disease with no contraindications for surgery. The thoracic surgery team scheduled a Uniportal Video-Assisted Thoracoscopy (U-VATS) atypical resection of the right lower lobe. After routine monitoring, intravenous anesthetic induction was performed with Propofol (dosage) and Fentanyl (dosage). Successful manual ventilation was ensured before achieving muscle relaxation through Rocuronium (dosage). Laryngeal view during direct laryngoscopy showed a Cormack-Lehane grade I. A 37 French double lumen tube (DLT) was inserted in the tracheal lumen. An effective right lung ventilation was readily achieved, while there seemed to be an obstacle to the left lung ventilation. Positioning of the DLT was therefore re-evaluated through the use of a bronchoscope: the right main bronchus and the right superior lobar bronchus were well visible, while a continuous layer of mucous tissue prevented the bronchoscope from proceeding into the left main bronchus. Retraction of the DLT under bronchoscopic view revealed the presence of a mucous septum on the left side of the tracheal wall, reducing the entrance space to the left main bronchus (Figure 1). A large tracheal diverticulum was recognized as being the obstacle to the correct intubation of the left main bronchus. (Figure 2). The DLT was therefore removed and replaced with a single 8 mm lumen tube and an EZ-bronchial-blockerTM with the aid of the bronchoscope, in order to isolate the right lung. The attached images were acquired after solving the problem of the pulmonary exclusion. U-VATS atypical resection of the right lower lobe was then performed. Intraoperative and postoperative courses were uneventful. A bronchial 3D reconstruction from CT-scan images was achieved to confirm the presence of a left posterolateral tracheal diverticulum causing the ineffective positioning of the DLT during patient’s intubation procedure (Figure 3).
3. Take Home Messages
Tracheal diverticulum is a rare pathological issue and, when present, can cause many difficulties in airways management. It is a benign condition presenting with one or multiple invaginations of the tracheal wall [1]. They are more often asymptomatic but can otherwise be suspected in case of symptoms such as chronic cough, dyspnea, stridor, or recurrent tracheobronchitis [2]. Endotracheal intubation can be challenging in patients with tracheal diverticula [3-5]. Perforation of a tracheal diverticulum caused by erroneous intubation can result in pneumomediastinum [6]. Tracheal diverticula can be detected by computed tomography (CT) scans. An accurate imaging study during the pre-operative evaluation of patients helps detecting possible causes of difficult airway management, especially when the surgical airway isolation of a lung is needed.
The case we present shows which errors can bring on the misdiagnosis of a tracheal diverticulum. In first place, radiological reports did not describe the presence of a tracheal diverticulum. Secondly, surgeons studying the case focused mainly on the images of the neoplasia. Finally, anesthesiologists read the radiological report without reviewing the images. Therefore, no medical doctor in the multidisciplinary team was aware of the presence of a tracheal diverticulum. Only mastery of the bronchoscopy technique by an experienced anesthesiologist, their knowledge of bronchial anatomy and its anomalies and of alternative choices for pulmonary exclusion, allowed to identify the obstacle and quickly choose an alternative for the one lung ventilation, without causing any harm to the patient [7]. It is therefore of primary importance for anesthesiologists to know the correct handling of the bronchoscope, a gold standard tool that can be used as an aid for routine tracheal intubation, also for difficult airway management, and to confirm airway abnormalities [8, 9]. It is also mandatory, from our point of view, not only to read the radiological reports but also to examine diagnostic images with a critical eye, looking for those details that could make the difference on anesthesiologic management of the patients.
References
- Sayit AT, Elmali M, Saglam D, et al. The diseases of airway-tracheal diverticulum: a review of the literature. J Thorac Dis 8 (2016): 1163-1167.
- Lin H, Cao Z, Ye Q. Tracheal diverticulum: a case report and literature review. Am J Otolaryngol 35 (2014): 542-545.
- Li-Ling Ching S, Yew-Hoong Chow M, Nai Ng H. Difficult lung isolation in a patient with an undiagnosed tracheal diverticulum. Journal of Cardiothoracic and Vascular Anesthesia 17 (2003): 355-356.
- Dinner M, Ward R, Yun E. Case report: Ventilation difficulty secondary to a tracheal diverticulum. Anaesthesiology 77 (1992): 586-587.
- Davies R. Difficult tracheal intubation secondary to a tracheal diverticulum and a 90-degree deviation in the trachea. Anesthesia 55 (2000): 923-925.
- Möller GM, Ten Berge EJ, Stassen CM. Tracheocele: a rare cause of difficult endotracheal intubation and subsequent pneumomediastinum. Eur Respir J 7 (1994): 1376-1377.
- Doolittle AM, Mair EA. Tracheal bronchus (Classification, endoscopic analysis, and airway management). Otolayngol Head Neck Surg 126 (2002): 240-243.
- Klein U, Karzai W, Bloos F, et al. Role of fiberoptic bronchoscopy in conjunction with the use of double-lumen tubes for thoracic anesthesia (A prospective study). Anesthesiology 88 (1998): 346-350.
- Komasawa N, Berg BW. Simulation-based Airway Management Training for Anesthesiologists-A Brief Review of its Essential Role in Skills Training for Clinical Competency. J Educ Perioper Med 19 (2017): 612.




 Impact Factor: * 4.2
Impact Factor: * 4.2 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 